Proximal Humerus Fracture
Overview
Proximal humerus fractures are common shoulder injuries. Proximal humerus fractures are one of the most common broken bones in the shoulder, particularly in the elderly due to osteoporosis. Proximal humerus fractures are the 3rd most common broken bone in patients older the age of 65, after only hip and wrist fractures.
A proximal humerus fracture typically occurs near the shoulder joint and can occur at various levels, with simple or comminuted fracture patterns.
Proximal humerus fracture (PHF) corresponds to all fractures of the anatomical neck, surgical neck, greater tuberosity (GT), or lesser tuberosity, whether isolated or combined.
A proximal humerus fracture occurs when the top segment of the upper arm bone, which appears like a ball, is broken. It may also be known as a shoulder fracture. The primary cause of proximal humerus fractures is a fall, particularly one onto an outstretched hand. High-speed car crashes are another common cause.
A proximal humerus fracture happens if the ball in the ball-and-socket shoulder joint breaks. The fracture is located at the top of the arm bone (humerus). The majority of proximal humerus fractures are non-displaced (not out of position), but 15-20% of these fractures are displaced, which can require more invasive treatment.
Proximal humerus fractures (PHF) contribute to 5-6% of all adult fractures. There is increasing recognition of the significance of managing these fractures in the context of elderly, low-energy falls, as these events contribute to the global impact of both the direct and indirect costs of osteoporosis and fractures due to fragility.
Also, as the general population ages and an increasing proportion of these patients are classified as bone density compromised, the nonoperative and operative management of PHFs continues to receive significant attention in the literature. A proximal humerus fracture typically requires treatment with a sling and a rehabilitation program rather than surgery.
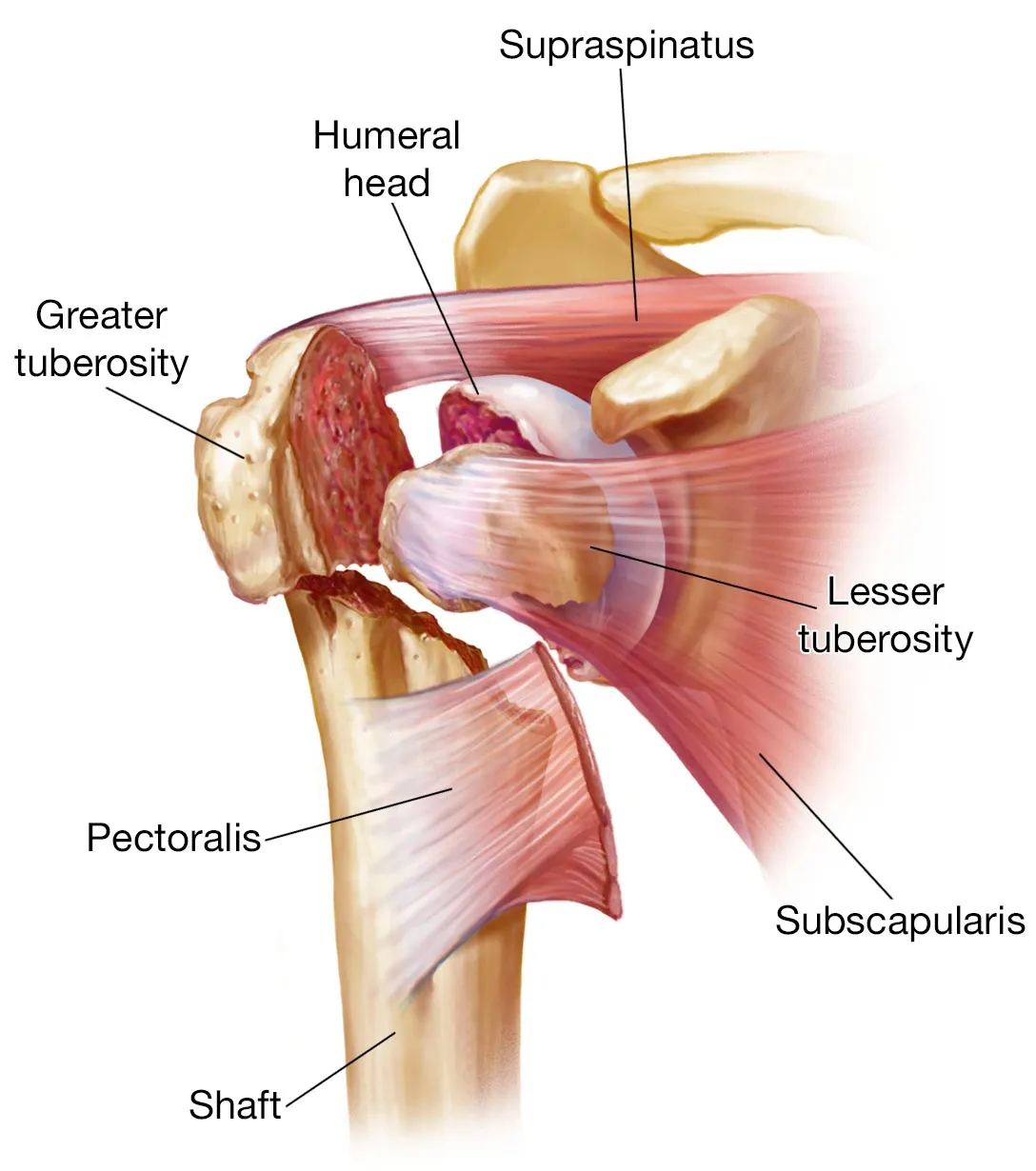
Relevant Anatomy
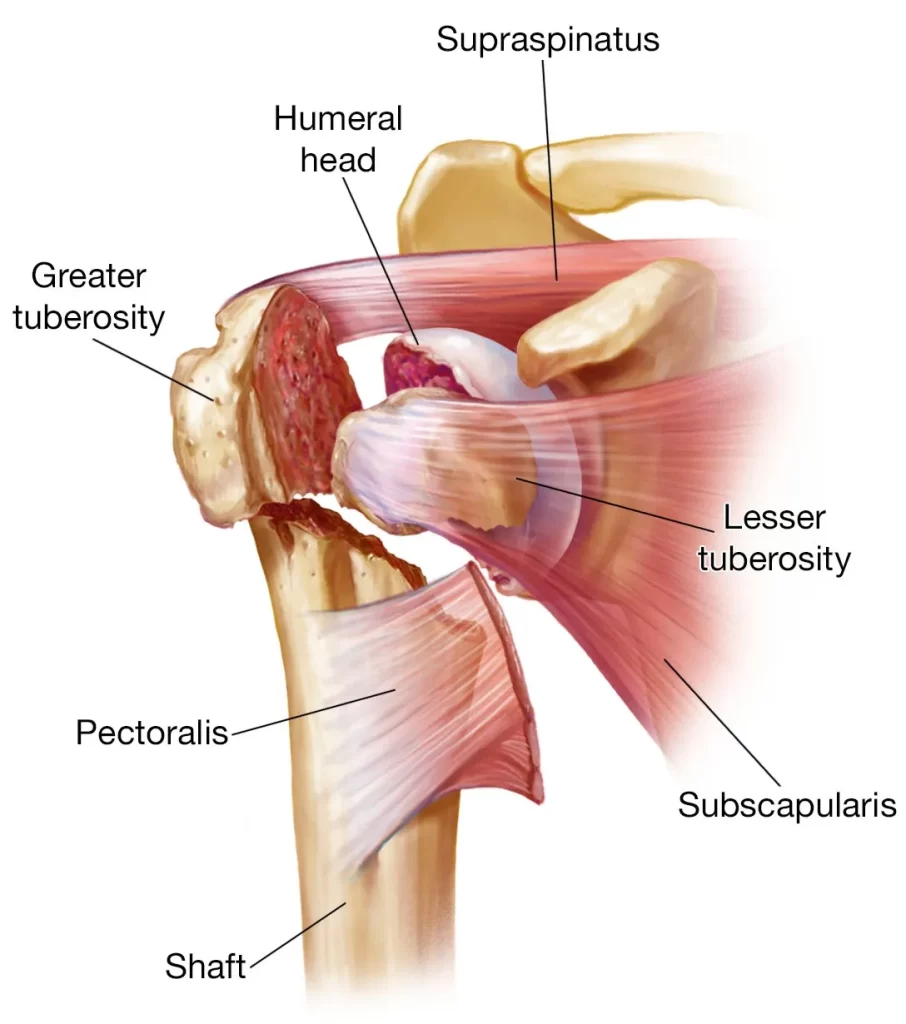
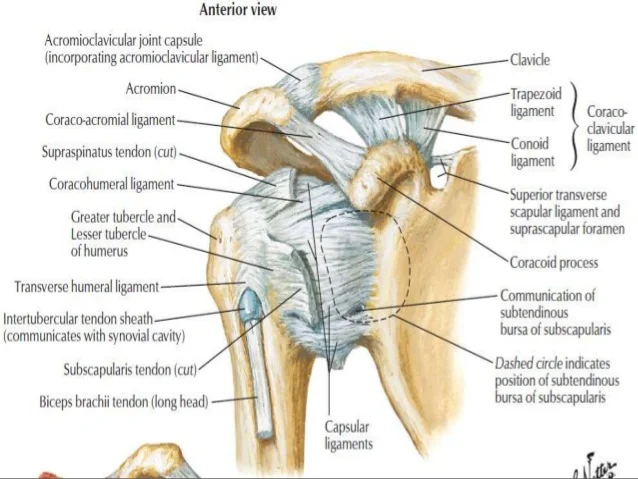
The humerus is a long bone in the upper arm that lies between the shoulder and the elbow, with the top part known as the proximal humerus. The four rotator cuff muscles, which are primarily responsible for shoulder stability and mobility, attach here.
The proximal humerus consists of multiple important components:
- Humeral Head: The upper part of the humerus appears like a ball and is called the humeral head. It lies in a hollow socket formed by part of the blade of the shoulder, which is known as the glenoid fossa, to form the glenohumeral joint or shoulder joint.
- Greater Tuberosity: The greater tubercle is a large nodule (bone lump) that lies on the outer side of the proximal humerus. Three of the four rotator cuffs attach to the greater tubercle: supraspinatus, infraspinatus, and teres minor.
- Lesser Tuberosity: The lesser tubercle is a smaller nodule located on the front of the proximal humerus. The 4th rotator cuff muscle, the subscapularis, attaches here.
- Anatomical Neck: The anatomical neck of the humerus is a diagonal groove that connects the head of the humerus to the greater and lesser tubercles. The articular capsule of the shoulder joint connects here.
- Surgical Neck: The surgical neck runs in the horizontal direction, just beneath the greater and lesser tubercles at the base of the humeral head. The majority of proximal humerus fractures happen at the surgical neck.
- Intertubercular Groove: A narrow groove that connects the greater and lesser tuberosities.
- Humeral Shaft
Function: Serves as an attachment for 13 muscles that contribute to hand and elbow movement, as well as upper limb function.
Muscles: The intrinsic muscles of the shoulder that connect the scapula and/or clavicle to the humerus are:
- Teres major
- Teres minor
- Infraspinatus
- Supraspinatus
- Subscapularis
- Pectoralis major
- Deltoid
- Biceps brachii
- Triceps brachii
- Coracobrachialis
- Latissimus dorsi
Neurovascular Factors:
Based on the pattern of injury, several neurovascular structures may be injured. The most frequently injured nerve in PHFs is the axillary nerve. Arterial injury occurs at a rate of about 5% and is more common in older people population. Two typical cases related to arterial artery injury at presentation are:
- Displaced or comminuted surgical neck fractures
- Subcoracoid dislocation
The posterior humeral circumflex artery is the main source of blood supply to the humeral head. The anterior humeral circumflex artery (AHCA) is noted for its extensive arterial branching and the anastomotic network it forms in the proximal humerus.
This theory was once thought to be the primary blood supply to the proximal humerus, but it has since been debunked. The AHCA has two main branches: the anterolateral ascending branch and the arcuate artery, with the latter one serving as the primary blood supply to the greater tuberosity.
Epidemiology
PHFs are the 3rd most common fracture in the elderly, following proximal femur and distal radius fractures, accounting for 10% of total fractures. PHFs account for approximately 5.7% of adult fractures, and their incidence rises with age. They are one of the most typical fractures in people over the age of 65. The typical age was 70 years (16-97).
In the United States, there were approximately 370,000 ED visits due to humerus fractures, with PHFs accounting for fifty percent of humerus fractures in 2008. A study in South-Eastern Australia found that the average age-standardized incidence rates for PHFs in men and women had been 40.6 (95% CI 32.7, 48.5) and 73.2 (95% CI 62.2, 84.1) per 100,000 person-years, respectively.
The risk of PHF increases with age and is most common in osteoporotic elderly women. In addition to bone fragility resulting from osteopenia or osteoporosis, commonly reported risk factors for falls include a lack of physical activity, impaired balance, or lower limb pain/injury.
Causes of Proximal Humerus Fracture
Proximal humerus fractures make up almost all of the upper arm fractures and five percent of all fractures. The typical causes of a proximal humerus fracture are:
- Falls: Proximal humerus fractures are most commonly caused by falling over onto an outstretched hand. The fall does not have to be from a great height; falling from a standing height is enough to break the bone. The most common cause is a fall down stairs.
- Direct Blow: A high-energy blow to the shoulder, such as a tackle or RTA, can result in a proximal humerus fracture. In these circumstances, the shoulder joint frequently dislocates, which means the head of the humerus slips out of the glenoid socket.
- Age: Proximal humerus fractures are most common in people over 60, as bones weaken and become more brittle with age. Proximal humerus fractures are the 3rd most frequent type of broken bone in the 65s, following hip and wrist fractures.
- Osteoporosis: Osteoporosis weakens bones, increasing the likelihood of fractures.
- Gender: Women are three times more likely to have a proximal humeral fracture than men.
Classification
Proximal humerus fractures can be classified based on the location of the break, the number of pieces broken, and whether or not the broken pieces have moved out of position.
PHF is classified into two categories: Neer and AO/OTA, as well as one specifically for GT fractures.
The Neer Classification
The four-segment classification system classifies PHFs according to the number of displaced segments or parts, with additional categories for articular fracture along with dislocation. The GT, lesser tuberosity, articular surface, and humeral diaphysis are all possible segments involved. Displacement of a segment is defined as a separation of more than 1 cm or a 45° angulation.
A proximal humerus fracture is typically classified using the Neer System, which considers the number of fracture “parts” and the degree of “displacement” between these parts.
Neer System divides the proximal humerus into four “parts”:
- Anatomical Neck
- Surgical Neck
- Greater Tuberosity
- Lesser Tuberosity
He then examines the amount of displacement of the parts. A displaced fracture occurs when a part is separated by more than 1cm or has an angulation greater than 45 degrees.
The Neer system may appear slightly confusing at first because all fracture lines in a given “part” are counted as a single unit rather than as individual fracture lines/segments. This means that even if one of the “parts” has multiple fracture lines, it is still classified as a single-part fracture.
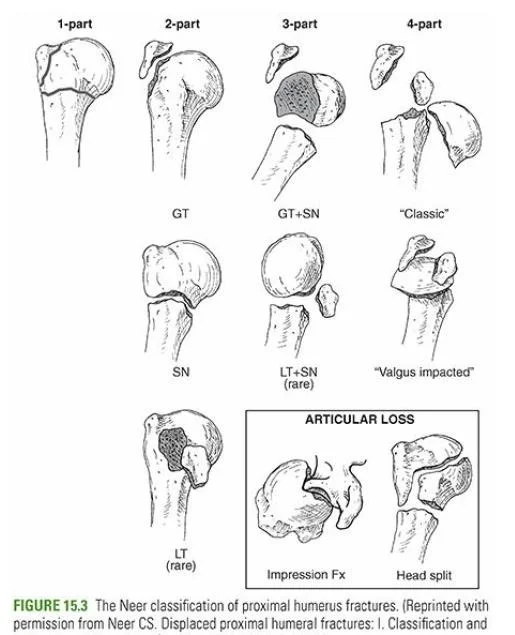
One-Part Fractures
A one-part proximal humerus fracture involves no bone displacement. Any one or more of the four parts can be fractured as long as the separation is less than 1cm and the angulation is less than 45 degrees.
For example, if the surgical neck and greater tuberosity fracture, it is still considered a one-part fracture as long as neither is displaced.
Approximately 75% of proximal humerus fractures are one-part fractures.
Two-Part Fractures
Two-part fractures occur when one part is displaced by more than one centimeter or rotated more than 45 degrees. Again, there could be multiple fractures in multiple parts, yet only one is displaced here.
Two-part fractures account for approximately 20% of all proximal humerus fractures.
Three-Part Fractures
Three-part proximal humerus fractures are those in which two parts are displaced. The surgical neck and one of the tuberosities (usually the greater tubercle) will almost certainly be displaced, while the other tuberosity will remain attached.
Three-part fractures account for approximately 5% of all proximal humerus fractures.
Four-Part Fractures
This is in which all four parts of the proximal humerus are fractured, with three of them displaced relative to the fourth. Four-part proximal humerus fractures are rare (less than one percent) but a serious injury that almost always requires surgery.
Valgus-Impacted Four-Part Fractures
This pattern was designated as a separate category in 2002. To accommodate the head, rotate it into a valgus position and push it down between the tuberosities. The articular surface is still in contact with the glenoid and does not move laterally.
AO/OTA Classification
The AO/OTA 2007 classification divides fractures into three categories based on their severity, articular/extraarticular, and unifocal/bifocal pattern.
- Type A is extraarticular and unifocal.
- Type B is extraarticular, bifocal
- Type C is articular
Fractures, Dislocations, and Articular Surface injuries
Dislocations were classified separately because they are more severe injuries with a higher risk of developing avascular necrosis and heterotopic ossification. Similarly, articular surface fractures were classified separately due to specific management considerations. There are two types: head-splitting fractures and impaction fractures.
Sign and Symptoms of Proximal Humerus Fracture
Proximal humerus fractures do not happen by chance; the injury can be associated with a specific event.
A proximal humerus fracture typically causes:
- Pain: The pain will be immediate, severe, and continuous. You will know you’ve accomplished it!
- Limited Movement: Any upper arm and shoulder movement will be very painful making movement very restricted.
- Swelling & Bruising: Within a few days of the injury, there will be major swelling and bruising in the upper arm, which may spread down to the hand.
- Crepitus: When moving the arm, you may hear or feel a grinding or grating sound. This occurs by broken fragments of bone rubbing together.
- Deformity: If there is a displaced fracture, the arm can appear deformed or “not look right”. When there is a fracture displacement, the deformity will be visible.
- Bleeding: occurs when the skin is punctured in an open fracture.
- Altered Sensation: Occasionally, the nerves surrounding the shoulder may be damaged during injury, resulting in affected sensations such as pins and needles or numbness beneath the fracture site. Just over half of all proximal humerus fractures are associated with nerve damage, but the axillary nerve is the most commonly affected.
Diagnosis
Physical Examination
Examination looks for signs of open fractures and inflammation, which can spread to the chest, arm, and forearm. Crepitus, also and pain are frequently present around the fracture site. Loss of deltoid contour lines suggests an associated shoulder dislocation, implying a more energetic mechanism. The examiner should determine whether any associated neurovascular injury exists.
A thorough neurovascular examination should also be conducted. Examiners should keep a close eye out for associated nerve injury (typically a transient neuropraxia to the axillary nerve), especially in the presence of a fracture-dislocation pattern. Arterial compromise is much less prevalent and can occur even when there are intact distal pulses palpated on the exam due to extensive collateral blood flow.
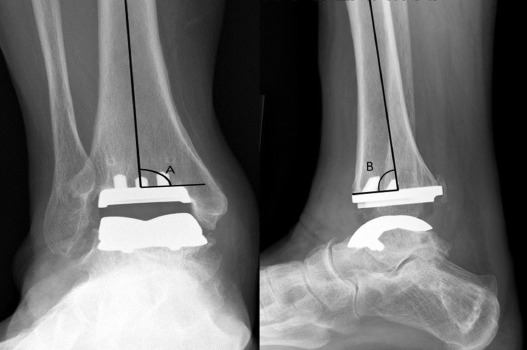
X-rays
Radiographic imaging is the most common baseline investigation for the diagnosis, classification, and management of PHFs. X-rays should contain:
- A true anteroposterior view.
- A transscapular Y view.
- An axillary lateral view.
The velpeau view can be used as a substitute depending on the patient’s ability to adjust to the axillary lateral radiographic position.
The velpeau view is performed in the patient’s arm held in internal rotation in a sling, and the film is taken superior to inferior while the patient leans backward into the beam field.
The west-point axillary view should also be considered.
The West Point X-ray technique involves placing the patient prone on an X-ray table. The affected shoulder is raised to the top of the table, and the cassette is placed in opposition to the superior aspect of the shoulder. The X-ray beam focuses on the axilla. The shoulder image is created by taking a tangential view of the anteroinferior rim of the glenoid rim.
Doppler Ultrasound
It can be used to evaluate the associated vascular injury and rotator cuff tears.
Computerized Tomography (CT)
It Can be utilized to evaluate complex fracture patterns, as well as quantify available bone stock and determine the extent and location of fracture union.
CT Angiography
It Can be used to accurately diagnose and guide the treatment of co-existing arterial injuries.
Magnetic resonance arthrography (MRI)
An additional imaging tool for evaluating periarticular soft tissue.
Angiography
A second imaging tool for evaluating vascular injuries.
Differential Diagnosis
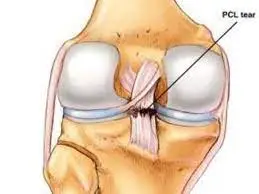
The evaluation should begin with a neurological and vascular examination of the affected extremity. Examine the entire limb for possible fractures. Concurrent fractures are particularly prevalent in high-energy injury mechanisms. The most common injuries associated with PHFs are axillary, suprascapular, or brachial plexus nerve injuries, axillary artery injuries, pneumothorax, haemothorax, and rotator cuff injuries.
Treatment of Proximal Humerus Fracture
A proximal humerus fracture is usually treated without surgery. Nearly 80% are undisplaced or minimally displaced, so non-operative treatment is acceptable.
Non-Surgical Treatment
Non-surgical treatment for a proximal humerus fracture involves:
Immobilization
A shoulder immobilizer is usually worn for the first several weeks after a proximal humerus fracture to help it heal in the right position.
A sling is modeled for the first few days or weeks after a proximal humerus fracture to stabilize the fracture and reduce swelling and pain.
The fracture must be completely immobilized for ten to fourteen days to allow the bones to knit back together and heal, so the sling must be worn at all times, day and night. After this, you can gradually decrease how much you wear the sling, and by around 12 weeks, you should no longer need it at all.
Usually, a shoulder immobilizer or sling and swath are used. They stabilize the elbow and forearm while counteracting the weight of the arm. The extra strap close to the body helps to immobilize the upper arm.
A collar and cuff sling is sometimes used to treat proximal humerus fractures. They provide less support, but allow the arm’s weight to provide gentle traction, which can help improve fracture alignment.
Medication
The physician will prescribe medicine to relieve pain and inflammation following a proximal humerus fracture, such as NSAIDs – non-steroidal anti-inflammatories like ibuprofen or naproxen. If you have an open fracture, you will be given antibiotics to help minimize the risk of infection.
Exercises
For the first few weeks following a proximal humerus fracture, the shoulder should be immobilized in a sling, but elbow, wrist, and hand exercises should be performed to prevent stiffness or weakness. You can usually do these with your arm out of the sling.
Exercises should be started immediately as possible and repeated at least four times per day. To avoid stiffness, move the elbow, wrist, and fingers through their full range of motion, and hand grips and balls are excellent tools for maintaining strength.
Following ten to fourteen days, you should be able to begin gentle exercises to help the shoulder move. A physiotherapist will work with you to develop a rehabilitation plan. Pendulum exercises are the best place to begin when regaining mobility. These are exercises that use gravity to move the arm, preventing the muscles from pulling on the fracture site.
After about three weeks, you can begin active assisted exercises, which involve using your normal arm or a bar/stick to assist and move the broken arm. You may also be provided a pulley system to operate.
Following nine weeks, the fracture should have healed, and you can begin active mobility and gradually strengthening exercises, such as resistance band exercises, to regain rotator cuff strength.
Rehabilitation will continue until you have restored full movement, strength, and stability in your shoulder and elbow. You may have to continue exercising for up to a year to achieve this. After a proximal humerus fracture, not everyone regains their full range of motion, and some people continue to have difficulty lifting their arm above head height.
To gain your full range of motion, flexibility, and strength as possible, you must strictly adhere to the rehabilitation program and perform exercises daily. Failure to do so will result in reduced shoulder movement, which will likely impair function.
Your doctor will see you regularly and take x-rays of your shoulder to monitor its healing process. Everyone heals at a different rate, so listen to your doctor or physical therapist about when you can move on to the next stage of rehabilitation.
Surgical Treatment
About fifteen percent of proximal humerus fractures become displaced and need surgery. In the majority of situations, metalwork is used to re-align and repair bones. This is a temporary measure to hold things together while the bone heals; it is not intended to be a long-term support structure. If the metalwork becomes loose or causes problems, it can be removed later. If the bone fails to unite, additional surgery will be necessary.
There are several types of surgery for proximal humerus fractures, depending on the type of fracture and the individual’s functional requirements.
Closed Reduction
A closed reduction is a procedure used to correct a proximal humerus fracture while under anesthesia, avoiding the need for a shoulder incision.
This might be sufficient, but if the realignment turns out to be unstable, the surgeon might also use K-wires or percutaneous pins to secure the bone. To keep the fractures from moving, they are put at different angles through the skin and into the bone. Because there is a chance of infection and pin migration, buried pins may be used in place of slightly exposed pins or K-wires, which make them easier to remove once callus formation has started.
The most common procedure for treating two-part surgical neck fractures is a closed reduction.
ORIF (Open Reduction Internal Fixation)
Open reduction internal fixation, or ORIF for short, is the process of employing screws and a metal plate to treat a fracture.
Either the front or side of the shoulder is incised. The fracture is decreased (realigned) if there is any displacement. The fracture site is subsequently stabilized by the insertion of a metal plate, which is fastened above and below by surgical screws. After that, the incision is sealed with sutures or staples.
When a patient is younger and has two, three, or four component fractures, or when there is displacement of the larger tuberosity, an ORIF is typically performed.
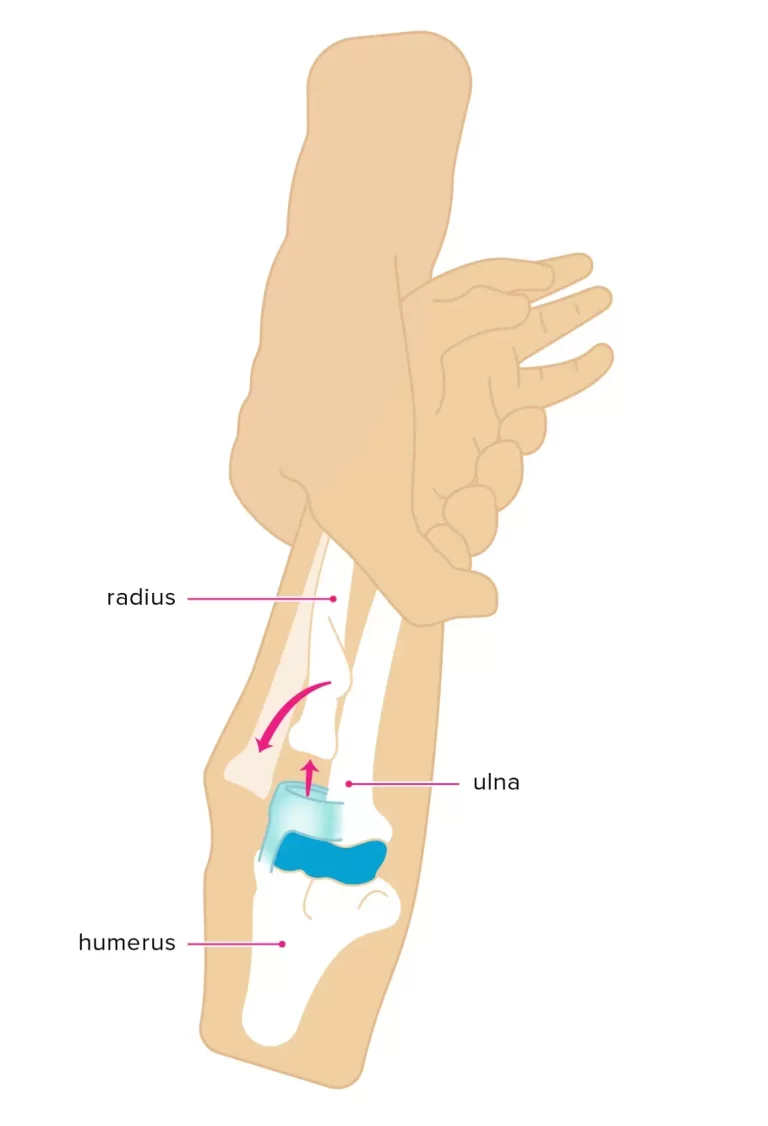
Intramedullary (IM) Nailing
A little anterolateral (front, side) incision through the skin and underlying soft tissues is created during intramedullary nailing. The medullary canal, a hollow in the middle of the humerus bone, is then used to insert a rod-shaped nail, which is secured in place with surgical screws. This stabilizes the fracture by splinting it from the inside out
When there is an injury to the humeral shaft below as well as a two- or three-part proximal humerus fracture, intramedullary nails are typically utilized.
Shoulder replacement surgery
The fractured humeral head is removed during a shoulder hemiarthroplasty, often known as a partial shoulder replacement, and is replaced with a metal implant. The implant stem is placed into the medullary canal, which is the depression in the middle of the upper arm bone, and is either cemented firmly in place or held in place with a particular type of cement. After that, the ball is fastened to the stem’s top.
When alternative treatments have failed or the fracture is extremely complicated, a shoulder hemiarthroplasty is typically performed. A rotator cuff injury, a four-part fracture, an anatomical neck fracture, or a fracture dislocation could all be present. A hemiarthroplasty is typically the best course of action if the humeral head’s blood supply has been impaired and there is a significant risk of osteonecrosis or the death of the bone.
Total Shoulder Arthroplasty
When the entire shoulder joint is replaced, this procedure is known as a total shoulder arthroplasty. A metal implant is put in place of the humeral head, which is formed like a ball. The implant features a half-moon-shaped form with a stem that passes through the center of the humerus bone.
A plastic socket is positioned and secured in place with specific cement after the socket portion of the shoulder blade joint is shaved down.
If the proximal humerus fracture is accompanied by injury to the glenoid, the shoulder will be replaced. It’s possible that the glenoid was injured at the time of the incident or that the joint has severe arthritis (degeneration), in which case a partial shoulder replacement would not be appropriate.
For a complete shoulder arthroplasty, the rotator cuff must remain intact; otherwise, there is a significant chance that the prosthesis will become loose. Ninety-three percent of complete shoulder replacements have a minimum 10-year lifespan.
Reverse Shoulder Replacement
Reverse shoulder replacement surgery may be necessary if the proximal humerus fracture has caused injury to the rotator cuff, either by partial tearing or complete rupture. People with minimal functional needs over 70 years of age are the best candidates. The shoulder’s deltoid muscle has to be in optimal functioning condition.
The term “reverse shoulder replacement” refers to the placement of the implant’s ball portion on the shoulder blade and socket on the humerus, which is the opposite of how things are normally done! This may seem like an odd thing to accomplish, but it allows the deltoid muscle to compensate for the rotator cuff deficit, allowing for a wider range of motion in the shoulder than would otherwise be possible.
Physiotherapy Management
Whether surgery is performed or not, recovery and rehabilitation following a proximal humerus fracture follow essentially the same steps. Regaining mobility range is the most important phase of the healing process.
Phase-1 (0-3 Weeks)
Immobilization: a sling that must be worn all day and all night (except during activity, cleaning, and personal hygiene).
Exercises: range-of-motion and strengthening exercises for the elbow, wrist, and hand; pendulum exercises for the shoulder
Phase 2 (3-9 Weeks)
Once there is no displacement and the fracture begins to unite:
Exercises: Shoulder mobility exercises with active assistance that gradually decrease the level of support starting after around six weeks.
Function: Moderately functional use
Phase 3 (After 9 Weeks)
You can advance your exercises once the proximal humerus fracture heals and the bones begin to fuse.
You must perform a mix of the following:
Strengthening Exercises: begin with isometric strengthening and proceed to resistance training and arm mobility exercises.
Mobility Exercises: keep going until you reach your maximum strength and range.
Recovery
Following a proximal humerus fracture, the following outcomes are typical:
- 1 Week: being able to type and write
- 6-12 Weeks: for the bone to have completely healed and to be free of the requirement for your sling.
- 3 Months: to be able to hang laundry on the line and reach up to grab items from a closet
- 3-6 Months: to resume lifting without any limitations
- 6-12 Months: to be fully functional again if there’s a chance that shoulder-arm mobility will always be somewhat limited
According to research, smoking (or consuming nicotine-containing products) can raise the risk of non-union by approximately six times and delay the healing of bones. Because nicotine reduces blood vessel size by around 25%, the bone receives less oxygen and nutrients needed for repair, which can significantly slow down the healing process.
Complications
The following are the most typical complications of a proximal humerus fracture:
- Decreased Shoulder Function: After a proximal humerus fracture, full strength and mobility may never be regained, especially in older individuals or those who don’t adhere to their training regimen. It normally takes up to a year following an injury or surgery to notice improvement.
- Frozen Shoulder: This can seriously restrict shoulder movement when the shoulder joint capsule grows and tightens. This usually occurs after a prolonged period of shoulder immobilization. Early initiation of an exercise regimen lowers the chance of adhesive capsulitis, often known as frozen shoulder. The section on the frozen shoulder has a wealth of further information regarding the causes, treatments, and recovery.
- Avascular Necrosis: Avascular necrosis, sometimes known as osteonecrosis, can arise from a proximal humerus fracture, which disrupts the blood supply to the humeral head. This is the period of decreased blood supply-induced bone cell death. Pain and limited mobility are the results of the humeral head gradually collapsing. Vessels that emerge from the armpit area and head upward, branching off the axillary artery, supply blood to the humeral head. The most common fractures to obstruct blood flow and result in avascular necrosis are anatomical neck fractures and four component fractures.
- Shoulder Arthritis: Early onset shoulder arthritis was more likely to occur in cases of shoulder joint damage.
- Surgical Risks: Risks associated with surgery include infection, nerve damage, poor bone healing, issues with wound healing, and prosthesis loosening.
Prevention
- Wear your seatbelt at all times.
- Wear the appropriate safety gear when participating in all sports and activities.
- It is important to always utilize the proper tools or equipment when reaching for anything at home. Never stand on counters, tables, or chairs.
- Adapt to a diet and exercise regimen that will support the health of your bones.
- If you have a family history of osteoporosis or are older than 50, discuss getting a bone density test with your healthcare provider.
- If you have difficulty walking or are more prone to falling, use a cane or walker.
FAQs
Is a proximal humerus fracture serious?
Unfortunately, proximal humerus fractures are frequently serious injuries, particularly when the bone’s alignment has shifted significantly. Changes in shoulder function are not uncommon, and people who suffer these injuries frequently do not recover their full strength or joint mobility.
Which location does proximal humerus fracture occur most frequently?
The surgical neck, located distal to the tuberosities, is the most common site for humerus fractures, particularly in the elderly. PHF-relevant deforming forces include pectoralis major, which displaces the humeral shaft anterior/medial.
What nerve is damaged in a humerus fracture?
The radial nerve is most likely to be damaged in humerus fractures with lateral displacement of the distal fracture segment because it is attached to the bone and cannot withstand the forces applied to it as a result of the movement.
Can a proximal humerus fracture heal without surgery?
Most proximal humerus fractures can be treated without surgery as long as the bone fragments are not displaced.
How long does a proximal humerus fracture take to heal?
Proximal fractures occur when the bone breaks near the shoulder joint. These fractures typically take 6 to 12 weeks to heal.
REFERENCES
- Professional, C. C. M. (n.d.). Humerus Fracture. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22990-humerus-fracture
- Triplet, J. (n.d.). Proximal Humerus Fractures – Trauma – Orthobullets. https://www.orthobullets.com/trauma/1015/proximal-humerus-fractures
- Humerus Fracture (Upper Arm Fracture). (2021, August 8). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/humerus-fracture-upper-arm-fracture
- Proximal Humerus Fractures. (n.d.). Physiopedia. https://www.physio-pedia.com/Proximal_Humerus_Fractures
- Pencle, F. (2023, August 4). Proximal Humerus Fracture. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470346/
- Proximal Humerus Fracture: Causes, Treatment & Recovery. (n.d.). Shoulder-Pain-Explained.com. https://www.shoulder-pain-explained.com/proximal-humerus-fracture.html
- Cluett, J. (2022, October 18). Proximal Humerus Fractures. Verywell Health. https://www.verywellhealth.com/proximal-humerus-fracture-2548596