Shin Splint
What is a Shin Splint?
Shin splints, or medically termed medial tibial stress syndrome, refer to the pain along the inner side of the tibia the prominent bone in the lower front leg. This condition involves inflammation of the muscles, tendons, and bone tissue surrounding the tibia, often manifesting between the lower leg and ankle.
Shin splints transpire when the leg muscles and bones in the lower part of the leg excessively pull and jerk at their insertion on the tibia. This can result from repeated activity or heightened stress on the tibia, leading to inflammation characterised by redness, swelling, and pain.
This discomfort commonly arises after increased physical activity, such as running, engaging in sports, military training, and dancing, and in individuals with osteoporosis who face an elevated risk.
Overall, shin splints represent a prevalent overuse injury in the leg.
What are the causes of a shin splint?
The causes of shin splints are multifaceted and often stem from repeated overload injuries. Exercises like walking, jogging, and leaping can cause the shin bone to become inflamed, swollen, or irritated because of their constant and repetitive impact.
Shin splints evolve as a result of persistent stress on the shin bone, leading to the pulling and tugging of muscles and connective tissues in the lower leg. Individuals who initiate a new exercise regimen abruptly, accelerate their sports activities too quickly, or engage in exercise for weight loss may be susceptible to developing shin splints.
This condition commonly arises when muscles and tissues are overworked due to repeated activities. Sudden changes in physical activity, such as an increase in exercise frequency, duration, or intensity, can also contribute to the onset of shin splints.
Some characteristics increase the likelihood of shin splints: flat or unusually rigid arches in the feet, inappropriate or worn-out shoes, inadequate footwear, weak ankle, hip, or core muscles, obesity, excessively taut calf muscles, and nutritional deficiencies such as low levels of Vitamin D. Shin splints are more common in runners especially those who run on uneven terrain or suddenly increase the intensity of their routines dancers, military personnel who march or walk a lot, long-distance walkers, and people who have osteoporosis.
What are the symptoms of Shin Splint?
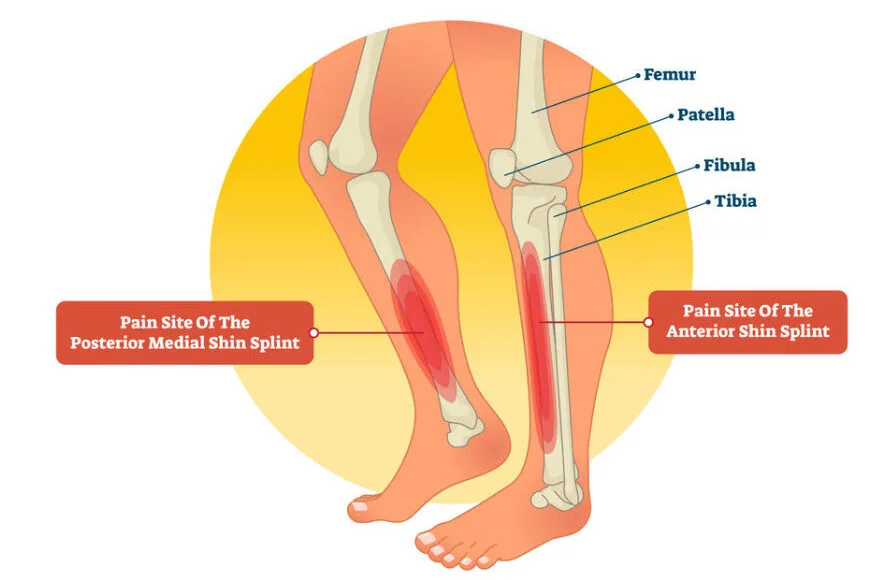
The primary indicator of shin splints is lower leg pain, ranging from mild to severe. The inner lower thigh or the front of the shin bone are the usual locations for this type of pain, which might start off as sporadic discomfort during action and develop into a chronic ache even after the activity has stopped.
This pain is often described as sharp, razor-like, or dull, accompanied by throbbing sensations in the front of the leg. It tends to intensify after physical activity, with the sore spot becoming more sensitive to touch.
Interestingly, the pain tends to diminish during periods of rest. Additionally, there may be mild to moderate swelling in the affected area.
Notably, women are more susceptible to progressing from shin splints to stress fractures, attributed to a higher incidence of diminished bone density and osteoporosis in this demographic.
Diagnosis of Shin Splint
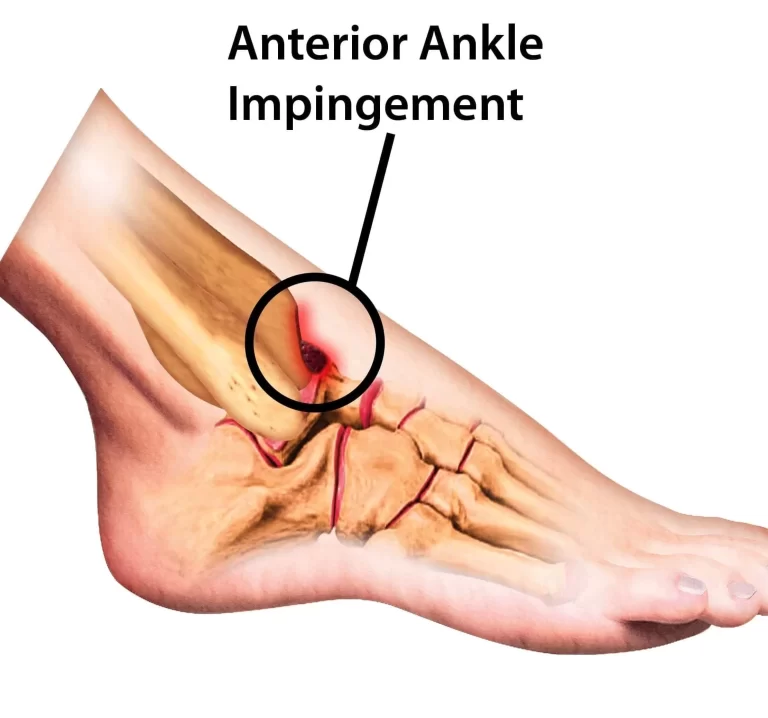
Shin splint diagnosis involves a comprehensive assessment conducted by doctors, encompassing a detailed patient history and physical examination. The doctor evaluates the patient’s gait, scrutinising the lower leg, ankle, and foot. This examination includes manipulating the ankle and foot, as well as assessing tenderness along the shin bone. Shin splints or a possible stress fracture can be diagnosed with the use of exercises like hopping or extended standing on the injured leg.
To exclude the possibility of a stress fracture, doctors employ various diagnostic methods, such as X-rays, bone scans, and MRIs (Magnetic Resonance Imaging). These imaging techniques not only help identify potential stress fractures but also reveal soft tissue injuries. Certain signs may be suggestive of stress fractures, such as increasing marrow involvement and periosteal oedema. In cases of shin splints, high-signal areas around the tibia are often visible on MRI scans.
During physical examination, the resurgence of pain with gentle or localised pressure over the tibia can provide valuable diagnostic clues. It’s generally observed that an examination involving more than 5 cm of the tibia yields more accurate results. Additionally, the presence of swelling, redness, or diminished pulses, along with shin splint symptoms, may suggest an alternative underlying cause.
Treatment of Shin Splint
Treatment for shin splints encompasses both nonsurgical and surgical approaches, tailored to the severity of the condition.
Nonsurgical Treatment:
Non-surgical treatment for shin splints involves the use of medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, aspirin, acetaminophen, and naproxen to alleviate pain and swelling.
Implementing the RICE method at home is an effective approach.
- Rest: Rest is the cornerstone for pain reduction, especially as shin splints often result from overuse. This entails several weeks of rest from activities that cause pain.
- It’s important not to over-rest; instead, avoid activities causing shin pain or putting excessive strain on your legs. Replace these with low-impact aerobic exercises like swimming, stationary cycling, walking, water walking, or using elliptical machines.
- Once pain has improved, decreased, or ceased, gradually reintegrate it into daily activities. For instance, if running on soft surfaces, start with shorter durations and distances, progressively increasing exercise time.
- Ice: Apply cold or ice packs for 15-20 minutes, 4–8 times a day, covered with a towel. Avoid direct skin contact.
- Compression: Utilise an elastic compression bandage on the calf muscle to prevent additional swelling and inflammation.
- Elevation: When icing shins, elevate the legs on a pillow or chair higher than the heart level to further reduce inflammation.
- Incorporate flexibility exercises: stretch lower leg muscles to alleviate tightness and reduce pain, involving various muscles in the leg.
Choose supportive shoes with good cushioning during daily activities to minimise stress on the shins.
Returning to exercise should occur only when pain-free for at least 2 weeks. Reintroduce activity at a lower intensity than before the injury, emphasizing a gradual increase.
Before starting exercise, ensure a thorough warm-up and stretching routine. Increase training intensity slowly, and if pain recurs, stop immediately. Use ice and rest for 1-2 days, then resume at a lower intensity, progressing more gradually than before.
Surgical Treatment:
Surgical intervention becomes a consideration for individuals with shin splints when conservative treatments prove ineffective, typically in severe cases. In such instances, a doctor may recommend surgery, known as a fasciotomy, to alleviate persistent pain.
During a fasciotomy, the surgeon makes small incisions in the fascia tissue surrounding the calf muscles, aiming to release tightness in the calf muscles. In certain cases, the surgical procedure may involve cauterising a ridge of the tibia.
Following surgery, it’s common to consult with a physiotherapy doctor or exercise physiologist who can oversee a safe recovery, especially for those leading highly active lives.
It’s worth noting that stress fractures, a related condition, are usually managed with a brace rather than surgical intervention.
Physiotherapy Treatment:
Physiotherapy treatment for shin splints involves a comprehensive approach focused on patient education and a graded loading exposure program to address functional gait and biomechanical overload factors.
- Acute Phase (0–3 days):
- Rest combined with medication, including NSAIDs and acetaminophen for pain relief.
- Cryotherapy with ice packs and the occasional use of analgesic gels for 10–20 minutes after exercise
- Isometric exercises and massages to reduce swelling
- Various physical therapy modalities, like ultrasound, soft tissue mobilisation, and electrical stimulation, may be employed.
- Subacute Phase (Day 4–Week 6):
- Modify training conditions by reducing running distance, intensity, and frequency by 50%.
- Advise patients to avoid high hills and uneven surfaces.
- Continue modalities to decrease inflammation.
- Introduce low-impact and cross-training exercises such as running on a hydro-gym machine, water running, and cycling.
- Gradually increase training intensity and duration, adding sport-specific activities and hill running as long as it is pain-free.
- Rehabilitation Exercises:
- Stretching: Involves seated shin stretch, soleus muscle stretch, gastrocnemius stretch, calf raises, & foam roll.
- Strengthening: Introduce a calf exercise programme to prevent muscle fatigue. Core, hip, and knee muscles can be strengthened to improve running mechanics and prevent lower-extremity overuse injuries.
- Proprioceptive Balance Training: Utilise one-legged stands or balance board activities to enhance neuromuscular education, increasing ankle joint efficiency and stabilising muscles to prevent re-injury.
- Consider orthotics for biomechanical foot problems, including custom-made options, casts, or pneumatic braces if necessary.
- Additional Therapies:
- manual therapy to control biomechanical abnormalities of the spine, sacroiliac joint, and other muscle imbalances.
- While acupuncture, ultrasound therapy injections, and shock-wave therapy exist, their efficiency is not universally proven.
- Taping or strapping may be employed if deemed necessary to restrict abnormal movement and prevent further damage.
- Return to Sport (Week 7):
- Gradually reintroduce running once the pain has decreased or resolved.
- Emphasise warm-up and joint stretching, initially avoiding uneven surfaces.
- Prioritise reestablishing distance before focusing on speed.
- Consider antipronation orthotics for individuals with MTSS or low dye taping.
- General Recommendations:
- Begin aerobic fitness with cross-training activities like sideboards, water running, and cycling.
- Emphasise flexibility and incorporate Theraband exercises.
- Choose proper shoes with good shock absorption, emphasising the importance of changing shoes every 250–500 miles to maintain optimal shock-absorbing capabilities.
Prevention for Shin Splint
Take proactive measures to prevent or minimise the risk of shin splints by incorporating the following strategies:
- Footwear: Wear Properly Fitted Athletic Shoes: Select shoes tailored to your specific sport, ensuring proper support. Recognise that shoes suitable for tennis may differ from those ideal for running.
- Consider Inserts for Arch Support: If you have high arches or flat feet, consider using inserts to provide additional arch support.
- Replace Shoes Regularly: For runners, replace shoes every 350 to 500 miles to maintain optimal support and shock absorption.
- Fitness Progression: Gradual Fitness Build-Up: Incrementally increases mileage or physical activity each week, avoiding sudden spikes. This gradual progression helps strengthen and loosen muscles, reducing the risk of tightness.
- Cross Training: Diversify Physical Activities: Incorporate cross-training with activities like swimming, biking, or yoga to vary movements and prevent monotony that may contribute to shin splints.
- Shock Absorption: Consider Shock-Absorbing Insoles: Explore the use of insoles designed to absorb shock, reducing the impact on the shins during exercise.
- Stretching: Pre-exercise Stretching: Prioritise stretching muscles before exercising to facilitate warm-ups and enhance flexibility.
By following these preventive measures, individuals can significantly reduce the likelihood of developing shin splints and promote overall lower leg health.
Conclusion
Shin splints are typically a temporary condition that can be alleviated through the RICE method (rest, ice, compression, and elevation of the leg), adjusting exercise routines, and wearing supportive footwear. If persistent, a prolonged duration of shin splints might necessitate examination for underlying issues like stress fractures. To prevent recurrence, evaluating factors such as diet, footwear, exercise habits, and flexibility becomes crucial.
For those experiencing prolonged shin-splint discomfort, testing for potential stress fractures or other contributing factors may be advisable. Effective treatment often involves a combination of rest, medication, and physical therapy encompassing pain modalities, targeted exercises, and stretching. In most cases, shin splints resolve within three to four weeks with adequate rest and recovery.
It’s noteworthy that timely intervention is crucial for optimal recovery, especially since stress fractures may require a more extended healing period. Therefore, early and comprehensive management of shin splints is essential to minimize the risk of complications and facilitate a prompt return to regular physical activities.
FAQ
How do you fix shin splints?
Steer clear of activities that make you swell, hurt, or feel uncomfortable, but don’t stop exercising altogether. Try low-impact activities like swimming, cycling, or water running while you’re recuperating. Frozen. For several days, apply ice packs to the injured shin four to eight times a day for 15 to 20 minutes at a time.
What causes shin splints?
Overuse of the muscles and bone tissue in your lower legs might result in shin splints. One possible cause for this could be an abrupt increase in the volume or intensity of exercise. the overpronation of the ankle joint, which occurs as the running foot strikes the ground.
Are shin splints OK?
Usually, jogging or other high-impact activities cause them. Shin splints, also known as medial tibial stress syndrome (MTSS), are a temporary condition that goes away with rest.
Do shin splints heal naturally?
One particularly prevalent overuse condition is shin splints. Most people recover from shin splints with rest and ice, and no long-term health issues arise. On the other hand, shin splints can progress to a tibial stress fracture if they are not addressed.
Do shin splints go away?
After taking a break from sports and other activities, the majority of people with shin splints heal. Shin splints often go away in three to four weeks, when your legs have had time to heal. After their legs heal, most people are able to start an exercise regimen again.
Are shin splints serious?
One particularly prevalent overuse condition is shin splints. Most people recover from shin splints with rest and ice, and no long-term health issues arise. On the other hand, shin splints can progress to a tibial stress fracture if they are not addressed.
What deficiency causes shin pain?
Tibial bone soreness and pain are linked to vitamin D insufficiency.
Should you walk with shin splints?
Although shin splints are often not a major condition, if you don’t take care of them, they can make it difficult to walk or perform daily tasks. Shin splints can be lessened in severity and frequency with the use of rest, ice, supportive footwear, and low-impact exercises.
How long do shin splints last?
Shin splints often go away in three to four weeks, when your legs have had time to heal. After their legs heal, most people are able to start an exercise regimen again. It is preferable to treat shin splints as soon as possible because recovery from a stress fracture takes longer.
Should you massage shin splints?
A common complaint regarding shin splints is that they go away but then come back when the workout regimen is resumed. This is frequently caused by tight or unhealthy calf muscles in particular. A massage is a particularly useful tool for relieving knots and tension in this particular muscle region.
Can I lift weights with shin splints?
Dr. Simmons states that, as shin splints are an overuse issue, the best course of treatment is to reduce further stress on the affected area, which typically entails taking time off from jogging. You can stretch, foam roll, cross-train, and strength train during this time.
Reference
- Shin Splints – OrthoInfo – AAOS. orthoinfo.aaos.org/en/diseases–conditions/shin-splints. Accessed 13 Nov. 2023.
- Professional, Cleveland Clinic Medical. “Shin Splints.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/17467-shin-splints. Accessed 13 Nov. 2023.
- “Shin Splints – Symptoms and Causes – Mayo Clinic.” Mayo Clinic, 16 Oct. 2021, www.mayoclinic.org/diseases-conditions/shin-splints/symptoms-causes/syc-20354105.
- Sankhla, Dr. Nirma. “Shin Splint – Cause, Symptoms, Diagnosis, Treatment.” Samarpan Physiotherapy Clinic, 19 Dec. 2022, samarpanphysioclinic.com/shin-splint.




2 Comments