ABOVE KNEE AMPUTATION : Physiotherapy Management
INTRODUCTION of The above knee amputations :
The above knee amputations (AKA) involve removing the leg from the body by cutting through both the thigh tissue and femoral bone.
“This procedure may be necessary for a wide variety of reasons, such as trauma, infection, tumor, and vascular compromise”
There are several known physiologic and psychologic complications that are associated with this procedure. However, an interprofessional approach to caring for these patients may decrease the rate of these complications.
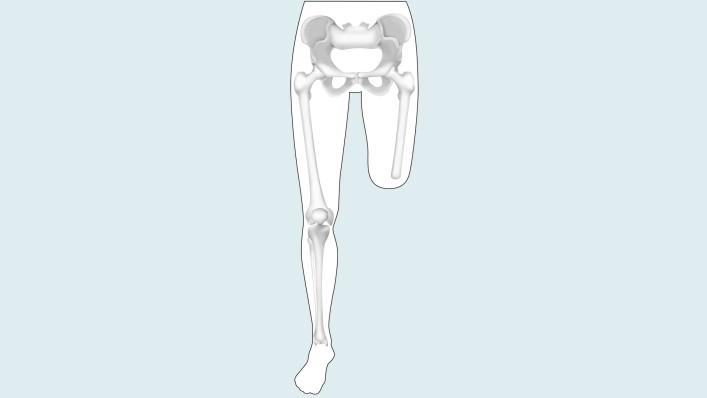
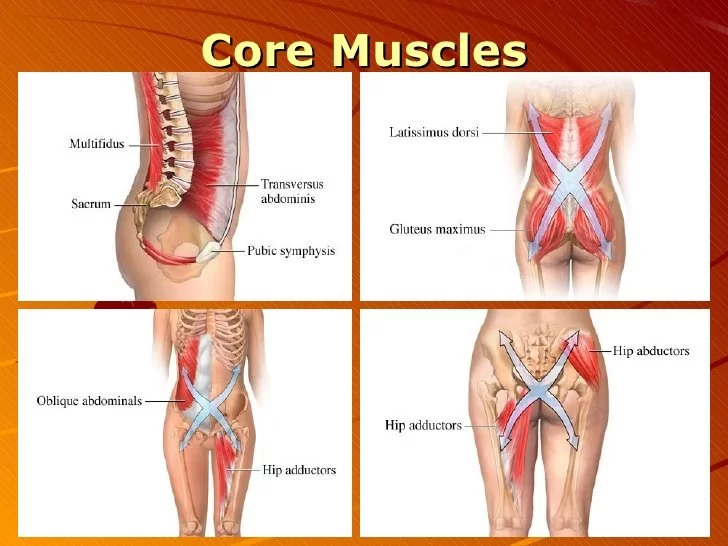
Anatomy :
The thigh divides into three compartments: anterior, posterior, and medial. These compartments surround the only bone in the thigh, the femur. The anterior compartment contains the vastus lateralis, vastus intermedius, vastus medius, rectus femoris, and genu articularis.
Branches of the femoral nerve lie within the anterior compartment and innervate the musculature. A cutaneous nerve, the saphenous, arises from the femoral nerve and innervates the medial skin of the thigh and leg.
The iliotibial band runs along the lateral border of the thigh, superficial to the vastus lateralis. The sartorius muscle is in the anterior portion of the thigh more proximally and in the medial portion more distally as it travels from the anterior superior iliac spine to its insertion on the anteromedial aspect of the proximal tibia as part of the pes anserinus.
The medial compartment of the thigh contains the adductor magnus, adductor longus, adductor brevis, and gracilis. These muscles receive their innervation from the obturator nerve, except for the adductor magnus, which also receives innervation from the sciatic nerve.
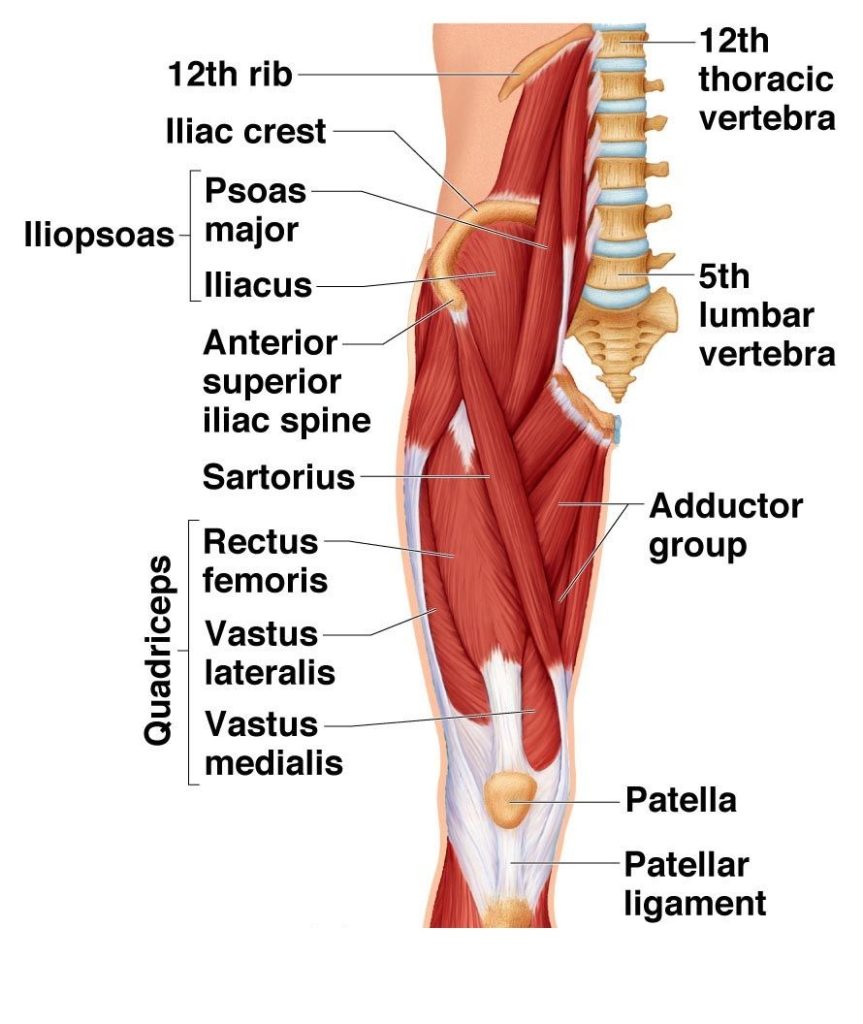
The medial compartment also contains the femoral artery and vein, which pass posteriorly after going through the adductor hiatus.
Proximally, the femoral artery divides into superficial and deep branches, with the deep branch providing blood flow to the muscles of the thigh and the femoral shaft.
The great saphenous vein runs superficially along the medial aspect of the thigh. The posterior compartment contains the long and short head of the biceps femoris, semitendinosus, semimembranosus, and sciatic nerve. Branches of the sciatic nerve innervate the musculature of the posterior compartment.
Indications For The above knee amputations :
- Can include trauma to the lower leg, which results in a non-viable leg at or near the level of the knee.
- soft tissue injury, limb ischemia and shock
- non-healing diabetic wounds
- necrotizing fasciitis,
- Vascular compromise, whether from injury or disease, which cannot be corrected, can also necessitate an AKA. Additionally, congenital disabilities that render a limb non-usable can indicate the need for this amputation.
Contraindications in The above knee amputations :
If the patient is not medically stable enough to survive the anesthesia and/or surgery. However, it merits consideration that the condition of the patient’s limb may be the cause of their medical instability.
Surgical Technique of the processor :
Patient placement is supine on the operating room table with the buttock of the surgical side elevated on a stack of blankets.
The operative leg gets prepped and draped in a sterile fashion. Planned skin incisions are marked. Some surgeons prefer anterior and posterior skin flaps for a fishmouth type closure with a slightly longer anterior flap, while others prefer medial and lateral flaps.
In a traumatic setting, flaps may be dictated by what tissue remains viable. An optional sterile tourniquet is then applied to reduce blood loss. Incisions are then made along the planned lines, and electrocautery is used to control bleeding.
Dissection is performed through the underlying fascia. Depending on the level of the amputation, muscle groups are identified and transected with electrocautery. Muscle groups should be transected approximately 1-2 inches longer than the planned bony cut to allow for musculature coverage of the bony end and myodesis.
Gentle traction is applied, and the nerves are sharply transected to reduce the risk of neuroma formation. A similar procedure is performed for any other nerves encountered, depending on the level of the amputation.
Which common Complications seen in The above knee amputations ?
Common complication are Muscle atrophy, surgical site wound infections, dehiscence and wounds from prosthetic wear.
Oedema
Stump oedema occurs as a result of trauma and the mishandling of tissues during surgery. After the amputation, there is an imbalance between fluid transfer across the capillary membranes and lymphatic reabsorption. This, in combination with reduced muscle tone and inactivity, can lead to stump oedema.
The complications that can arise from stump oedema include wound breakdown, pain, reduced mobility and difficulties with prosthetic fitting.
Wounds and Infection
Surgical site infection after amputation is common and as well as increasing patient morbidity, can have negative effects on healing, phantom pain and time to prosthetic fitting. Risk factors for a stump infection include diabetes mellitus, old age and smoking, which are all common denominators amongst the amputee population. The decision to insert a drain and use clips instead of sutures is also associated with increased infection risk.
- Tissue Necrosis
- Skin Blisters
- Sinuses and Osteomyelitis
- Pain
Post-Amputation Pain, Residual Limb Pain, Phantom Limb Sensation,Phantom Limb Pain
Treatment of major complication-
- Adequate post-op analgesia
- Patient education
- Limit oedema
- Prevent contractures
- Address musculoskeletal weakness and imbalances
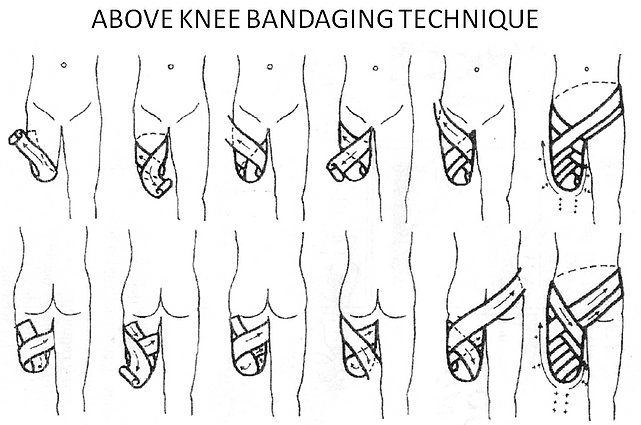
- Desensitisation – massage/bandaging
- Get patient moving, distraction helpsEarly prosthetic training
Clinical Significance
Above-the-knee amputations can have a significant clinical impact on the lives of patients. Many patients do not have the resources to obtain a prosthesis and may have to continue using a wheelchair following the procedure.
For those who do get a prosthesis, their mobility is significantly affected. One study showed that patients with a unilateral transfemoral amputation had a self-selected walking speed 8.6% slower than that of their non-amputee counterparts.
Another study showed a 49% increase in oxygen consumption during ambulation in patients with an above-the-knee amputation. Approximately 65% more energy expenditure is required to ambulate in above-the-knee amputees when compared to patients without an amputation.
PHYSIOTHERAPY TREATMENT
This number can be increased to 100% when the amputation is performed due to vascular compromise, as compared to trauma. This increased energy expenditure and decreased mobility may ultimately affect both the personal and professional lives of these patients.
Components
- Breathing exercises
- Active range of motion exercises
- Resistance exercises
- Passive range of motion exercises
- Bed mobility and transfers
- Positioning
- ADL
- Walking and wheelchair use
Goals
- Obtain maximum independence
- Prevent oedema
- Maintain joint ROM
- Prevent amyotrophy (muscle atrophy)
- Increase the muscular activation
- Prevent muscular weakness
- Prevent bronchopneumonia
- Control pain
- Sensory reeducation
- Support the client psychologically
- Prevent pressure sores
Prior to trans-femoral surgery
- Prescribe exercises for preoperative conditioning to improve your upper and lower extremity strength and flexibility
- Teach you how to walk with a walker or crutches
- Educate you about what to expect after the procedure
AFTER SURGERY:
Physical therapy will begin soon after surgery when your condition is stable and the doctor clears you for rehabilitation. A physical therapist will review your medical and surgical history, and visit you at your bedside. Your first 2 to 3 days of treatment may include:
- Gentle stretching and range-of-motion exercises
- Learning to roll in bed
- sit on the side of the bed
Prevention of Contractures in The above knee amputations :
A contracture is the development of soft-tissue tightness that limits joint motion.
Your physical therapist will help you maintain normal posture and range of motion at your hip. Your physical therapist will show you how to position your limb to avoid development of a contracture, and teach you stretching and positioning exercises to maintain normal range of motion
Compression to Address Swelling
Your physical therapist will help you maintain compression on your residual limb to protect it, reduce and control swelling, and help it heal.
- Use of rigid dressings / removable rigid dressings immediately post-operatively.
- Stump bandaging.
- Use of stump shrinkers.
- Compression therapy – pumps, elevation.
- Massage.
- Newer techniques involving use of silico
- ne or polyurethane sleeves / liners.
- Use of temporary or interim prostheses.
Pain Management:
- use of electrical stimulation and TENS (transcutaneous electrical nerve stimulation) for pain
- Performing manual therapy, including massage and joint manipulation to improve circulation and joint motion.
- stroking the skin with different types of touch to help reduce or eliminate the sensitivity reaction
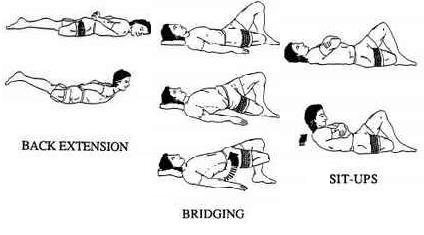
Strengthening Exercises
- Strengthening of all lower limb muscle of sound leg
- Strengthening of Hip Extension,Hip flexar,Hip abductar,Hip adductar of amputed leg
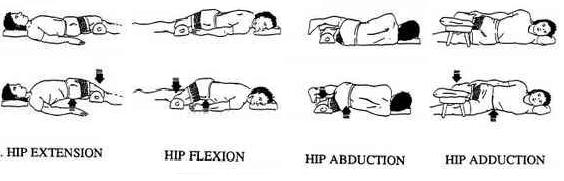
- back extensar
- bridging
- sit-up
prosthesis use and care

- how to put your new prosthesis on and take it off
- how to manage a good fit with the socket type you receive.
- help you to gradually build up tolerance for wearing your prosthesis for increasingly longer times, while protecting the skin integrity of your residual limb.
- You will continue to use a wheelchair for getting around, even after you get your permanent prosthesis, for the times when you are not wearing the limb.
Prosthetic training
it is a process that can last up to a full year. You will begin when the physician clears you for weight-bearing on the prosthesis. Your physical therapist will help you learn to stand, balance, and walk with the prosthetic limb
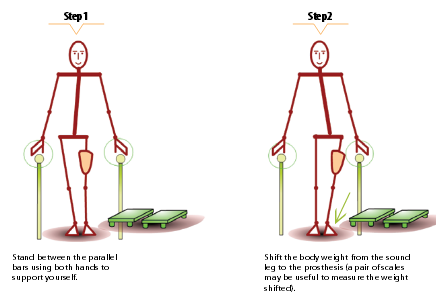
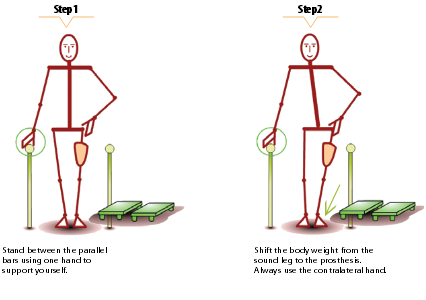
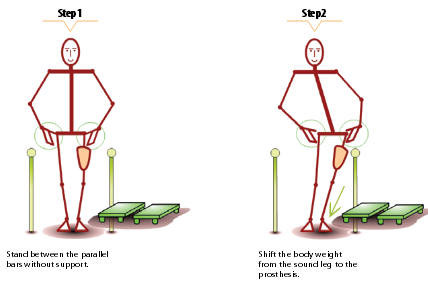
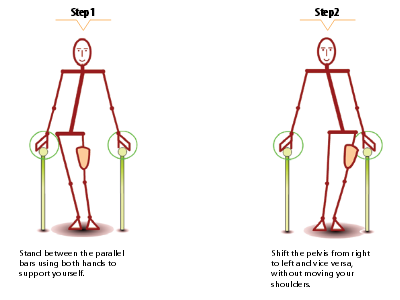
Exercises for Weight bearing and balance:
- Partial weight bearing (two-hand support)
- Partial weight bearing (one-hand support)
- Partial weight bearing (fingertip support)
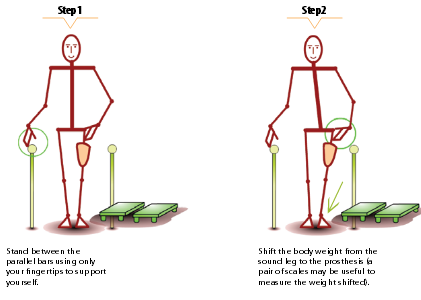
- Partial weight bearing (without support)
- Partial weight shift (two-hand support)
- Partial weight shift (one-hand support)

- Partial weight shift (without support)
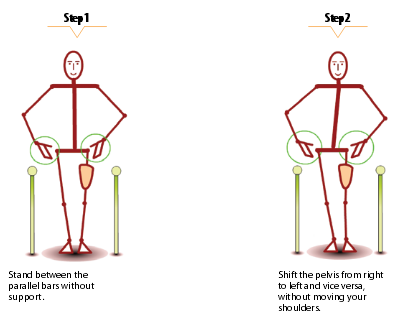
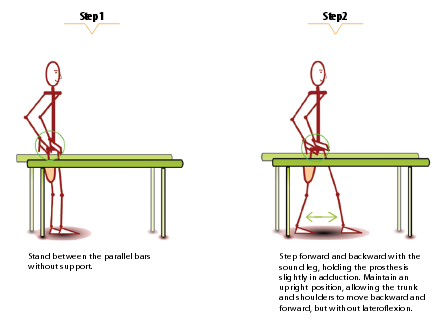
- Pelvic rotation

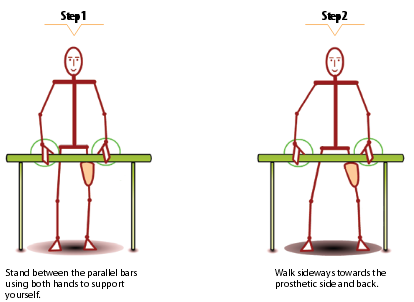
- Sideward walking (two-hand support)
- Full weight shift (two-hand support)

- Full weight shift (without support)

- Heel strike (with or without support)

- Balance board

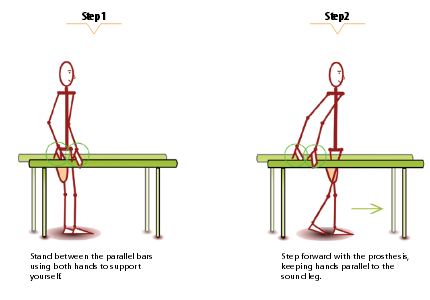
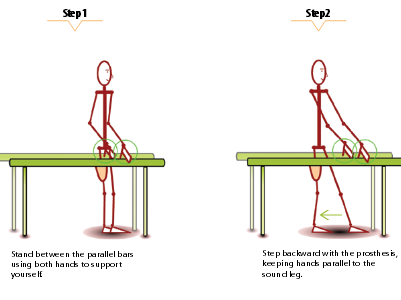
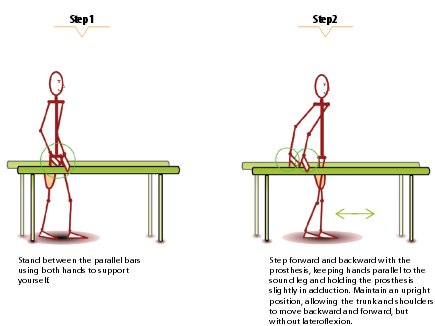
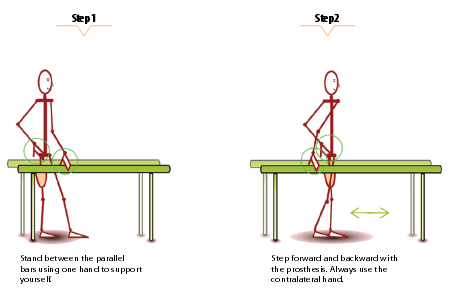
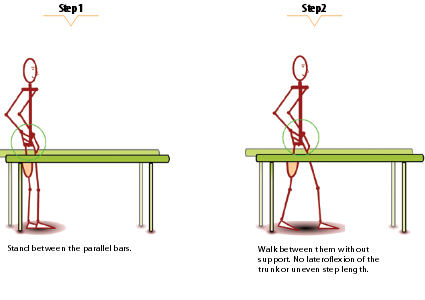
gait training:
- Sound-leg step forward (two-hand support)
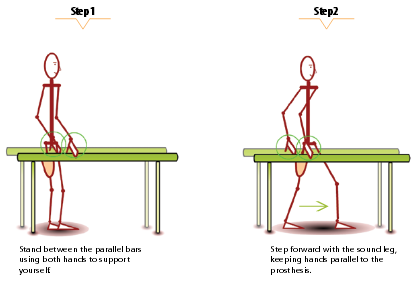
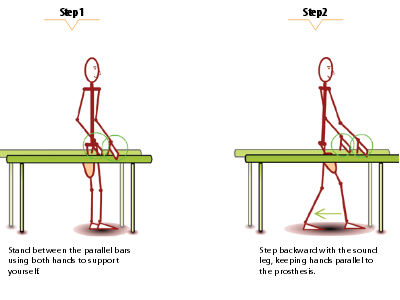
- Sound-leg step backward (two-hand support)
- Sound-leg step through (two-hand support)

- Sound-leg step through (one-hand support)

- Sound-leg step through (without support)
- Prosthetic-leg step forward (two-hand support)
- Prosthetic-leg step backward (two-hand support)
- Prosthetic-leg step through (two-hand support)
- Prosthetic-leg step forward (one-hand support)
- Prosthetic-leg step through (without support)

- Walking between the parallel bars (one-hand support)

- Walking between the parallel bars (without support)
Walking on an uneven surface

Going up and down a slope

Climbing a staircase – Climb a staircase starting with the sound leg. Follow with the prosthesis.
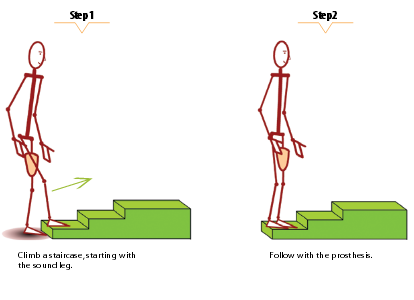
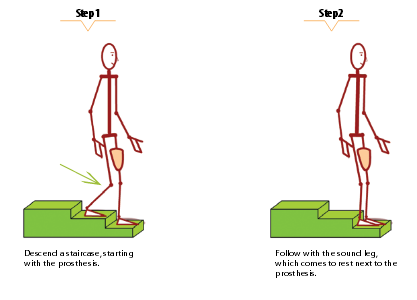
Descending a staircase – starting with the prosthesis Follow with the sound leg which comes to rest next to the prosthesis