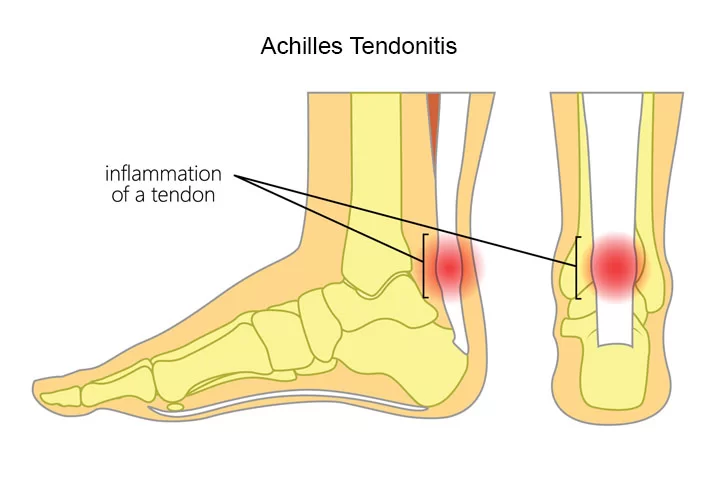
Achilles Tendinitis
What is an Achilles Tendinitis?
Achilles tendinitis is an overuse injury that causes inflammation, pain, and stiffness in the Achilles tendon, which connects the calf muscles to the heel bone.
It commonly affects runners, athletes, and individuals who suddenly increase their activity levels. It’s also typical for middle-aged people to solely participate in weekend activities like basketball or tennis.
Treatment typically includes rest, ice, stretching, strengthening exercises, and a gradual return to activity.

Symptoms:
After jogging or engaging in other sports, Achilles tendinitis pain usually begins as some aching in the back of the leg or above the heel. More intense pain episodes can happen after running, stair climbing, or extended running.
Additionally, you may feel stiff or painful, particularly in the morning, although this normally goes away with light exercise.
- Heel pain
- Ankle pain.
- Calf Tightness/Stiffness
- Tenderness in your tendon.
- Calf Muscle weakness.
- Swelling at the back side of the Ankle
You might experience further discomfort:
either after working out or the day after.
as you go uphill or upstairs.
beginning in the morning and getting better all day.
Achilles Tendinitis Types
The affected area of your tendon is defined by the two types of Achilles tendinitis:
Noninsertional Achilles tendinitis:
Your tendon’s main fibers begin to degrade, bulge, and thicken. Those who are more active are more likely to get this kind of Achilles tendinitis.
Insertional Achilles tendinitis:
The lower portion of your heel, where the tendon attaches or inserts into your heel bone, is affected. Even those who are not active can be impacted. However, long-distance runners and other individuals who overuse the tendon are most likely to be affected.
Causes of Achilles Tendinitis:
Achilles tendinitis is caused by repetitive or intense strain on the Achilles tendon, the band of tissue that connects your calf muscles to your heel bone. This tendon is used when you walk, run, jump, or push up on your toes.
The structure of the Achilles tendon weakens with age, which can make it more susceptible to injury — particularly in people who may participate in sports only on the weekends or who have suddenly increased the intensity of their running programs.
Risk factors:
A number of factors may increase your risk of Achilles tendinitis, including:
- Achilles tendinitis occurs most commonly in men.
- Age. Achilles tendinitis is more common as you age.
- Physical problems. A naturally flat arch in your foot can put more strain on the Achilles tendon. Obesity and tight calf muscles also can increase tendon strain.
- Training choices. Running in worn-out shoes can increase your risk of Achilles tendinitis. Tendon pain occurs more frequently in cold weather than in warm weather, and running on hilly terrain can also predispose you to Achilles injury.
- Medical conditions. People who have psoriasis or high blood pressure are at higher risk of developing Achilles tendinitis.
- Medications. Certain types of antibiotics, called fluoroquinolones, have been associated with higher rates of Achilles tendinitis.
Complications:
Achilles tendinitis can weaken the tendon, making it more vulnerable to a tear (rupture) — a painful injury that usually requires surgical repair.
Prevention:
While it may not be possible to prevent Achilles tendinitis, you can take measures to reduce your risk:
Increase your activity level gradually. If you’re just beginning an exercise regimen, start slowly and gradually increase the duration and intensity of the training.
Take it easy. Avoid activities that place excessive stress on your tendons, such as hill running. If you participate in a strenuous activity, warm up first by exercising at a slower pace. If you notice pain during a particular exercise, stop and rest.
Choose your shoes carefully. The shoes you wear while exercising should provide adequate cushioning for your heel and should have firm arch support to help reduce the tension in the Achilles tendon. Replace your worn-out shoes. If your shoes are in good condition but don’t support your feet, try arch supports in both shoes.
Stretch daily. Take the time to stretch your calf muscles and Achilles tendon in the morning, before exercise, and after exercise to maintain flexibility. This is especially important to avoid a recurrence of Achilles tendinitis.
Strengthen your calf muscles. Strong calf muscles enable the calf and Achilles tendons to better handle the stresses they encounter with activity and exercise.
Cross-train. Alternate high-impact activities, such as running and jumping, with low-impact activities, such as cycling and swimming.
Diagnosis of Achilles Tendinitis:
To find the origin of any pain, tenderness, or swelling, your doctor will apply light pressure to the affected area during the physical examination. Additionally, he or she will assess your foot and ankle’s reflexes, range of motion, alignment, and flexibility.
Imaging tests:

X-rays. Although soft tissues like tendons cannot be seen with X-rays, they can be used to rule out other illnesses that might be causing the same symptoms.
Ultrasound. The device visualizes soft tissues, such as tendons, using sound waves. Additionally, color-Doppler ultrasound can assess blood flow surrounding the Achilles tendon, and ultrasound can create real-time images of the tendon in action.
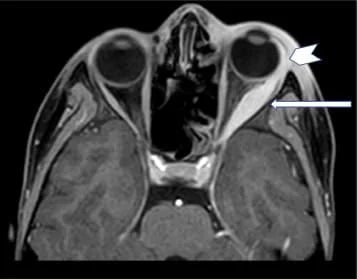
Magnetic resonance imaging (MRI). MRI equipment may create incredibly detailed images of the Achilles tendon by using radio waves and a powerful magnet.

Treatment of Achilles Tendinitis:
Initially, your doctor will suggest nonsurgical treatment. If you’ve been experiencing symptoms for a few months, it can take several months for the pain to subside.
The RICE method is one nonsurgical treatment for Achilles tendinitis:
- Rest: Give up any activities that cause your tendon to become stressed. Change to low-impact exercises that won’t strain your Achilles tendon, like swimming.
- Ice: As needed throughout the day, apply ice on your tendon for up to 20 minutes.
- Compression: Use surgical tape or an athletic wrap to provide pressure on your tendon.
- Elevation: Place your foot on cushions over your heart while lying down to minimize swelling.
Self-care techniques typically work effectively for tendinitis. However, your doctor may recommend alternative treatments if your symptoms are severe or ongoing.
Medical Treatment:
If over-the-counter pain medications — such as ibuprofen (Advil, Motrin IB, others) or naproxen (Aleve) — aren’t enough, your doctor might prescribe stronger medications to reduce inflammation and relieve pain.
Physiotherapy treatment:
Physiotherapy is the use of mechanical or physical methods, including heat or exercise, to treat a disease or condition. These treatments are given by a physiotherapist. Additionally, he or she will offer recovery support, education, and instruction.
For an Achilles tendon injury, the following treatments are often used:
- Stretching and flexibility exercises. These are key to helping your tendon heal without shortening and causing long-term pain.
- Strengthening exercises. They will help you regain the strength you might have lost while the tendon was healing. And they will help protect you from another injury.
- Ultrasound heat therapy. It improves blood circulation, which may aid the healing process.
- Deep massage. It helps you increase flexibility and blood circulation in the lower leg. It can also help prevent further injury.

A special type of strengthening called “eccentric” strengthening, involving a slow let down of weight after raising it has been found to be especially helpful for persistent Achilles problems.
Orthotic devices. A shoe insert or wedge that slightly elevates your heel can relieve strain on the tendon and provide a cushion that lessens the amount of force exerted on your Achilles tendon.

Surgery:
If several months of more conservative treatments don’t work or if the tendon has torn, your doctor may suggest surgery to repair your Achilles tendon.
When to consult a physician
Contact your physician if you have chronic Achilles tendon pain. If the pain or weakness is severe, get medical help right away. Your Achilles tendon can be damaged, or ruptured.
Epidemiology
In athletes, the cumulative lifetime injury incidence for the Achilles tendon is about 24 percent. The frequency of running-related injuries ranges from 11% to 85%, or 2.5 to 59 injuries for every 1,000 hours of running. According to one study’s findings, 1–2% of competitive adolescent players have Achilles tendinopathy.
According to a different survey, 9% of recreation athletes sustain injuries. A lifetime injury incidence of 2.35 per 1000 is closely linked to participation in sports. In older males, this incidence rises. The majority of Achilles tendinopathy ruptures occur in males, with a male-to-female ratio of 3.5:1, while the total incidence rate is 2.1 per 100,000 person-years.
Prognosis
The prognosis for Achilles tendinopathy is improved by early and proper therapy. Achilles tendinosis of insertion (TAI) is often treated with surgery, which has a success rate of more than 80%. According to a study by Stenson et al., the likelihood of nonoperative therapeutic failure increases with the number of risk variables.
A 55% risk of conservative therapy failure was associated with higher visual analog scale scores, limited ankle range of motion, previous corticosteroid injections, and Achilles tendon enthesophytes. These risk factors can therefore assist surgeons in determining when surgical intervention is required in the appropriate clinical setting.
A retrospective investigation by Sanalla and colleagues found that bone-tendon autografts were a dependable method for Achilles tendon strengthening with a low risk of complications.
Conclusion
Achilles tendinopathy is a complex disease that can have a big effect on people, athletes, and non-athletes alike, by making it harder for them to exercise and do other physical activities. Conservative or physical therapy is usually the first line of treatment for Achilles tendinopathy. In order to improve patient outcomes when treating cases of Achilles tendinopathy, an interdisciplinary healthcare team may be required.
FAQs
Can Achilles tendonitis heal itself?
Achilles tendonitis is not self-healing. Resting the injury, applying ice, and using other nonsurgical Achilles tendonitis treatments can help it heal.
Is Achilles tendonitis serious?
Under your doctor’s guidance, the majority of Achilles tendinitis instances can be resolved with rather easy at-home care. Self-care techniques are typically required to stop reoccurring episodes. Tendon tears, or ruptures, may result from more severe forms of Achilles tendinitis and may need to be repaired surgically.
How can I heal my Achilles tendon naturally?
Rest, Ice, Compression, and Elevation
By keeping your foot stationary, a walking boot may help your Achilles tendon repair. Immobilization for two or three weeks following a diagnosis of Achilles tendinitis may be advised by doctors. Crutches can assist in removing foot weight.
How to sleep with Achilles tendonitis?
Compressive elastic bandages or wraps can assist lessen tendon mobility and swelling. To lessen swelling, elevate the affected foot above your heart. At night, sleep with your injured foot up.
References
- Pabón, M. a. M., & Naqvi, U. (2023, August 17). Achilles tendinopathy. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK538149/




8 Comments