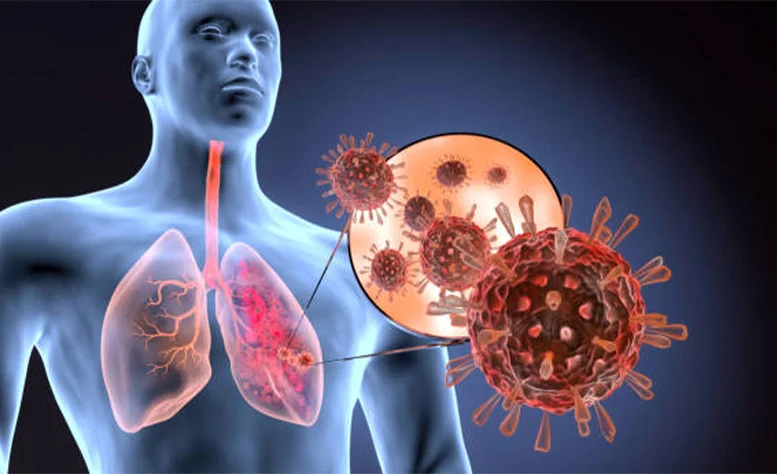
Acute Respiratory Distress Syndrome (ARDS)
What is Acute Respiratory Distress Syndrome?
Acute respiratory distress syndrome occurs when fluid builds up in the tiny, alveoli in your lungs. The fluid keeps your lungs from filling with little air, which means less oxygen reaches your bloodstream.
ARDS is a type of respiratory failure caused by the rapid onset of the spread of inflammation in the lungs.
Acute respiratory distress syndrome other name is respiratory distress syndrome, Adult respiratory distress syndrome, and shock.
Signs and symptoms of ARDS:
- Shortness of breath
- Fast breathing
- The low oxygen level of the blood
- Muscle fatigue
- General weakness
- Low blood pressure
- Hacking cough
- Fever
- Bluish skin coloration
- Chest pain
- Loss of speech
- Fast pulse rate
- Mental confusion
- discolored skin and nails
Complications of acute respiratory distress syndrome:
- Lungs: Barotrauma, Pulmonary embolism, Pulmonary fibrosis, Ventilator-associated pneumonia, Lung collapse, Lung fibrosis
- Gastrointestinal: Bleeding, Ulcer, dysmotility, pneumoperitoneum, bacterial translocation
- Neurological: Hypoxic brain damage
- Cardiac: Abnormal heart rhythms, Myocardial dysfunction
- Kidney: Acute kidney failure, Positive fluid balance
- Mechanical: Vascular injury, Pneumothorax
- Nutritional: Malnutrition, Electrolyte abnormalities
- Atelectasis: small air pockets within the lung
- Failure of multiple organs
- Pulmonary hypertension
- Blood clots
- Muscle weakness
- Post-traumatic stress disorder
- Anxiety
- Depression
Causes of acute respiratory distress syndrome:
- Pneumonia
- Aspiration
- Inhalational lung injury
- lung contusion
- Chest trauma
- Sepsis
- Shock
- Pancreatitis
- Trauma
- Cardiopulmonary bypass
- Burns
- Increased intracranial pressure
- Blood clots
- Pneumothorax
- Pulmonary fibrosis
- Drug overdose
- The coronavirus
Risk factors:
- After the age of 65 years
- Chronic lung disease
- Drinking alcohol
- Smoking cigarette
- Toxic shock
- Liver failure
Diagnosis:
- Blood test
- Chest X-ray
- CT scan
- Throat and nose swabs
- Electrocardiogram
- Echocardiogram
- Airway examination
Differential diagnosis:
- Cardiogenic edema
- Exacerbation of interstitial lung disease
- Acute interstitial pneumonia
- Diffuse alveolar hemorrhage
- Acute eosinophilic lung disease
- Organizing pneumonia
- Bilateral pneumonia
- Pulmonary vasculitis
- Cryptogenic organizing pneumonia
- Disseminated malignancy
Treatment of Acute Respiratory Distress Syndrome:
It is mostly treated in the ICU (intensive care unit) along with treatment of the underlying cause.
Mechanical ventilation:
Mechanical ventilation can be used by oxygen may be given through a fitted face mask or a cannula fitted over the nose.
Steps to minimize complications from acute respiratory distress syndrome are commonly used. These include:
- Sedation to manage pain.
- Breathing tests to determine when the patient is safe to remove the tube and ventilator.
- Blood thinners to prevent clots.
- Minimizing fluid buildup in the lungs.
- Minimizing stress ulcers in the stomach.
- Active mobility and physical therapy to prevent and increase muscle weakness.
Airway pressure release ventilation and Positive end-expiratory pressure can be used in mechanical ventilation.
Prone position:
This position of lung infiltrates in ARDS is non-uniform. Repositioning into the prone position improve oxygenation by relieving atelectasis and improving perfusion. If this is done early in the treatment of severe acute respiratory distress syndrome it confers a mortality benefit of 26% compared to supine ventilation.
Fluid management:
Several studies have shown that pulmonary function and outcome are better in people with acute respiratory distress syndrome who lost weight or whose pulmonary wedge pressure was lowered by diuresis or fluid restriction.
Medication:
- Corticosteroid
- Inhaled nitric oxide
- Alvelestat
- Medication to prevent the bleeding
- Medication to keep you calm and comfortable
Post-operative and rehabilitation care:
Tracheostomy and Percutaneous Endoscopic Gastrostomy:
Many patients with ARDS require a tracheostomy and a percutaneous feeding tube in the recovery phase. The tracheostomy facilitates application from the ventilator, making it easy to clear the secretions and more comfortable. The tracheostomy is usually done at two to three weeks, followed by a percutaneous feeding tube.
Nutritional Support:
Most patients with acute respiratory distress syndrome have difficulty eating and muscle wasting. These patients are either given parenteral feeding, depending on the condition of the gastrointestinal tract. Almost every type of nutritional supplement has been studied in patients with acute respiratory distress syndrome, but so far, none has proven to be the magic bullet.
Activity:
Since patients with acute respiratory distress syndrome are bed-bound, frequent position changes are highly recommended to prevent bedsores and deep venous thrombosis. In conscience patients, one can minimize the sedation and sit down in a chair.
Prognosis:
The overall prognosis of acute respiratory distress syndrome is poor, with mortality rates of approximately 40%. Exercise limitation, physical and psychological sequelae, decreased physical quality of life, and increased costs and use of health care services are important sequelae of acute respiratory distress syndrome.
Consultations:
Management of patients with acute respiratory distress syndrome requires a professional and interprofessional team of healthcare workers that includes:
- Pulmonologist
- Respiratory Therapist
- Intensivist
- Infectious disease
- Dietitian
Preventive measure:
If you have recently had ARDS, improve your recovery by:
- No smoking
- No drinking alcohol
Physiotherapy treatment of acute respiratory distress syndrome:
Mobilization and exercise:
- Acute effects
- Long-term effects
- Preventative effects
Body Positioning:
- Hemodynamic effects related to fluid shifts
Breathing Control Maneuvers:
- Coordinated breathing with activity and exercise
- Spontaneous euxinic hyperventilation
- Maximal tidal breaths and movement in three dimensions
- Sustained maximal inspiration
- Pursed lip breathing to end-tidal expiration
- Incentive spirometry
Coughing Maneuvers:
- Active and spontaneous cough with closed glottis
- Active Assist
- Eg, forced expiratory technique, huff
Relaxation and Energy Conservation Interventions:
- Relaxation procedures at rest and during activity
- Energy conservation
- Pain control interventions
ROM exercise:
- Active
- Assistive active
- Passive
Postural Drainage Positioning:
- Bronchopulmonary segmental drainage positions
Manual Techniques:
- Autogenic drainage
- Manual percussion
- Shaking and vibration
- Deep breathing exercises and coughing
Suctioning:
- Open suction system
- Closed suction system
- Tracheal tickle
- Installation with saline
- Use of manual inflation bag
Summary:
Acute respiratory distress syndrome occurs when fluid builds up in the tiny, alveoli in your lungs. The fluid keeps your lungs from filling with little air, which means less oxygen reaches your bloodstream. ARDS is a type of respiratory failure caused by the rapid onset of the spread of inflammation in the lungs. Acute respiratory distress syndrome other name is respiratory distress syndrome, Adult respiratory distress syndrome, and shock.
FAQ:
What is the best treatment for Acute respiratory distress syndrome?
The goal of treatment for acute respiratory distress syndrome is to improve oxygen levels and treat the underlying cause. oxygen therapy is the primary treatment for acute respiratory distress syndrome
What are the 4 signs of respiratory distress?
Shortness of breath.
Rapid breathing
Increase heart rate
Coughing produces phlegm.
Bluish skin
What are the three stages of Acute respiratory distress syndrome?
In acute respiratory distress syndrome, the injured lung is believed to go through three phases: exudative, proliferative, and fibrotic, but the course of each phase and the overall disease progression is variable.
What are the causes of Acute respiratory distress syndrome?
Sepsis may be the most common cause of acute respiratory distress syndrome that develops after severe trauma or burns.
How do you increase oxygen in Acute respiratory distress syndrome?
These strategies include recruitment, prone positioning, ventilation, inhaled nitric oxide, corticosteroid treatment, and even extracorporeal membrane oxygenation
What antibiotics are used for ARDS?
Piperacillin-tazobactam
Doxycycline
Macrolides
Cephalosporins






One Comment