Anterior Interbody Lumbar Fusion Surgery
Overview
Anterior lumbar interbody fusion (ALIF) is a surgery to treat disc problems in the low back.
Lumbar spine anatomy
The lower back (where most back pain happens) consists of the five vertebrae in the lumbar region and supports much of the weight of the upper body. The spaces between the vertebrae are maintained by intervertebral discs that act like shock absorbers through away the spinal column to cushion the bones as the body moves. Ligaments hold the vertebrae in place, and tendons attach a muscle to the spinal column. Thirty-one pairs of nerves are rooted in the spinal cord and they control body movements and transfer signals from the body to the brain.
- The spine extends from the skull to the coccyx and includes the cervical region, thoracic region, lumbar region, and sacral region. The lumbar spine consists of five moveable vertebrae (numbered L1 to L5). The lumbar vertebrae, as a group, create a lordotic curve.
- The intervertebral discs are responsible for mobility without sacrificing the supportive strength of the vertebral column. The intervertebral discs, along with the laminae, the pedicles, and the articular processes of adjacent vertebrae, create a space via which spinal nerves exit.
- The complex anatomy of the lumbar region is a remarkable combination of these strong vertebrae (with their numerous bony elements) linked by joint capsules, flexible ligaments/tendons, large muscles, and highly sensitive nerves. that also has a complicated innervation and vascular supply.
- The lumbar spine has the largest vertebrae bodies in the axial spine.
Components of vertebral bodies
- anterior vertebral body
posterior arch formed by
pedicles:- pedicles project posteriorly from the posterolateral corners of the vertebral bodies
lamina
- lamina project the posteromedially from the pedicles, join in the midline
- spinous process
- transverse process
mammillary processes
- separate ossification centers
- project posteriorly from the superior articular facet
pars interarticularis
- mass of bone between superior articular facets and inferior articular facets
site of spondylolysis
Articulations
- intervertebral disc: act as an articulation above and below.
- facet joint (zygapophyseal joint):- formed by superior and inferior articular processes that project from the junction of the pedicle and lamina.
- facet orientation:- facets become more coronal as you move inferior or downwards.
Vertebrae
Typical lumbar vertebrae have many features distinct from those typical of cervical vertebrae or thoracic vertebrae.
- Presence of a large vertebral body.
- A spinous process is thick and short, relative to the size of the vertebra, and projects perpendicularly from the body
- the articular facets are markedly vertical, with the superior facets directed posteromedially and medially
- Facets also have the special feature of a curved articular surface. This is one feature that changes lumbar vertebrae from thoracic vertebrae.
- add the mammillary process on the posterior aspect of a superior articular process.
- One lumbar vertebra may be considered atypical. L5 has a large body and transverse processes of whole vertebrae. The anterior aspect of the body has a greater or higher height compared to the posterior. This produces the lumbosacral angle between the lumbar region of the vertebrae and the sacrum.
Muscles of your lumbar spine
The lumbar muscles, along with the abdominal muscles, work to move the trunk and the lower back. The muscles and ligaments provide strength and stability to your lower back and allow you to bend forward, backward, and rotate. The muscles that attach to the lumbar spine include:
- Latissimus dorsi.
- Iliopsoas.
- Paraspinals.
Ligaments of the lumbar spine
Ligaments in the lumbar spine connect bone to bone to help to keep the lumbar spine stable, allow smooth motion of the spine and assist absorb the force of trauma. Lumbar spine ligaments include:
- Anterior longitudinal ligament.
- Posterior longitudinal ligament.
- Supraspinous ligament/interspinous ligament.
- Ligamentum flavum.
- Intertransverse ligament.
- Iliolumbar ligament.
Nerves of the lumbar spine
You have 5 pairs of lumbar spinal nerves, one that branches off from the right and left sides of L1 to L5. The nerves run down from the lower back and merge with other nerves to form a network of nerves that control pain signals and the movements of the lower limbs.
- The L1 spinal nerve provides sensation to your groin and genital area and helps move your hip muscles.
- L2, L3, and L4 spinal nerves provide sensation to the front part of your thigh and the inner side of your lower leg. These nerves also control hip muscle movements and knee muscle movements.
- The L5 spinal nerve provides sensation to the outer side of your lower leg, the upper part of your foot, and the space between your first and second toes. This nerve also controls hip movements, knee movements, foot movements, and toe movements.
- The sciatic nerve consists of the L4 and the L5 nerves plus other sacral nerves. Your sciatic nerve begins in the rear pelvis and runs down the back of the leg, ending in the foot.
Blood vessels of the lumbar spine
Branches of the large abdominal aorta supply blood and nutrients to the vertebrae, muscles, and ligaments of the lumbar region.
Functions of the Disc
A primary function of the disc is to join the vertebrae and permit movement between them. The Other functions are typical of the erect spine: a shock absorber, a load distributor, and a separator of the posterior facets to keep the size of the intervertebral foramen.
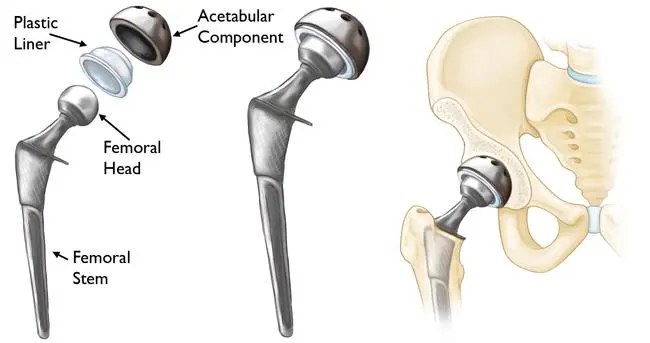
Anterior lumbar interbody fusion (ALIF) is a surgery to treat disc problems in the low back. Fusion closes together two or more bones to stop painful motion and correct those alignments. Through an incision in front of the belly, the disc is removed. A bone graft is placed in the space to restore the height and relieve nerve pinching. During the healing time, the bones fuse into one solid piece. An Anterior Lumbar Interbody Fusion (ALIF) surgery is a type of spinal fusion performed to stabilize a painful motion segment in a lower back, generally caused by lumbar degenerative disc disease and/or spondylolisthesis. The surgical approach is through the abdomen, to access the front–or the “anterior”–of the spine, where the disc is situated.
Anterior lumbar interbody fusion is a type of spinal fusion that utilizes an anterior (front – via the abdominal region) approach to fuse (mend) the lumbar spine bones together. Interbody fusion means an intervertebral disc is removed and replaced with a bone (or metal) spacer, in these cases using an anterior approach. The anterior technique is frequently favored when multiple spinal levels are being fused and multiple discs require to be removed. Anterior lumbar interbody fusion might be performed in conjunction with or without a posterior decompression (laminectomy) and/or instrumentation (use of metal screws/rods). The anterior ALIF approach is also ideal when only one spinal level is fused and posterior decompression and/or instrumentation are not needed. Though the anterior lumbar interbody fusion approach involves retracting (moving out of the way, temporarily) large blood vessels (aorta, vena cava) and the intestines, there is a wide exposure of the intervertebral disc without retraction of the spinal nerves and neurologic structures (and therefore, a reduced risk of neurologic injury). Anterior lumbar interbody fusion is commonly performed for a variety of painful spinal conditions, such as degenerative disc disease and spondylolisthesis, among others.
Anterior lumbar interbody fusion, often abbreviated ALIF, is the type of spine surgery performed to treat low back disorders including degenerative disc disease (DDD) and spondylolisthesis. degenerative disc disease and spondylolisthesis are examples of spinal problems that might compress spinal nerves and lead to instability. Compression or pinching of nerve structures may lead to low back, buttock, and leg sciatica pain. another neurologic symptom may include tingling, numbness, and weakness in one or both legs. The goal of an Anterior Lumbar Interbody Fusion procedure is to decompress the nerves, stabilize the lumbar spine, relieve symptoms, and not able the patient to return to regular activities of daily living.
Anterior Lumbar Interbody Fusion (ALIF) is a method used to fuse the lumbar spine, via an approach from the front of the spine through the abdomen. Anterior lumbar interbody fusion stands for:
Anterior = front(approach to the spine is from the front, through a small incision in the lower part of the abdomen). The surgical incision is made in the abdomen (for example, the stomach area) generally on the left or right side.
Lumbar = low back(one or more vertebrae of the lumbar spine is fused). The lumbar spine is one part of the spine. Those are five vertebral bodies in the low back; numbered L1 (top) through L5 (bottom). The disc levels are also abbreviated. For example, L3 and L4 refer to the intervertebral disc space between the third lumbar vertebral bodies and the fourth lumbar vertebral bodies (bones).
Interbody = between two vertebral bodies(fusion between two vertebral bodies where the disc usually would sit). The interbody space is the disc space.
Fusion = to join or combine(formation of bony bridge and stabilization of the spine)
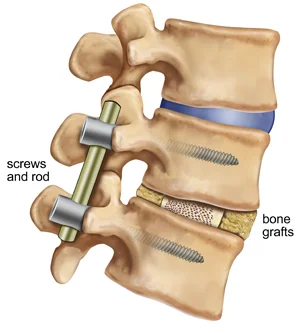
Bone graft is inserted into the space between the upper and lower vertebral bodies. Instrumentation (for example, screws, plates, cages, ) is implanted to immobilize (stabilize) the low back. The body’s natural healing processes lead to the new bone growing into and around the instrumentation resulting in a spinal fusion.
Not every patient with lumbar degenerative disc disease or spondylolisthesis needs spine surgery. Anterior lumbar interbody fusion, for the following reasons: non-operative treatment fails to ease symptoms, progressive worsening of neurologic symptoms or pain, spinal instability, and/or neurological problems. loss of function or movement, Numbness, and weakness are examples of neurologic dysfunction.
What is anterior lumbar spine fusion?
The doctor may recommend spinal fusion to repair damaged discs and realign bones leading to back pain or leg pain. There are many ways to reach the spine and perform a fusion. The surgeon will discuss the best approach for the unique problem.
During anterior fusion, the incision is made in the front of the belly. A spine surgeon and a vascular surgeon work as a group. The vascular surgeon clears a path to the spine, moving the side of the vessels to the legs. A spine surgeon removes the damaged disc or injured disc and fills the space between the bones with a spacer bone graft. The spacer restores the height between the bones, corrects the spinal curvature abnormality, and eases pinched nerves. The graft becomes a bridge between the 2 bones to promote fusion. In a few cases, the graft is strengthened with the screws and the metal plates.
As a body heals, new bone grows surrounding the graft. After three months to six months, the graft shall fuse the two vertebrae into one solid piece of bone. such as reinforced concrete, instrumentation and fusion work together. Depending on the symptoms, a one-level or multi-level fusion might be performed. A one-level fusion merges two bones while a two-level fusion merges three bones. Fusion would take away some flexibility in the spine, but most patients do not notice.
What is an ALIF (Anterior lumbar interbody fusion)?
An Anterior lumbar interbody fusion is a spinal operation where the spine is approached from the front rather than from the back. It is performed via the abdomen, generally with the assistance of a vascular surgeon to move the major blood vessels out of the way. A disc is removed and pressure on the nerves could be relieved. A large cage is then placed in the space where the disc was situated, and screws are inserted through the cage or a plate and into the spinal bones for extra stability.
Anterior lumbar interbody fusion (ALIF) is a spine surgery that involves approaching the spine from the front (or anterior) of the body to remove all or part of a herniated disc from in between two adjacent vertebrae (interbody) in the lower back (or lumbar spine), then fusing, or joining together, the vertebrae on either side of the remaining disc space using bone graft or bone graft substitute.
The graft material acts as a binding medium and also assists maintain normal disc height – as the body heals, the vertebral bone and bone graft finally grow together and stabilize the spine. Instrumentation, such as the rod, the screw, the plate, the cage, the hook, and the wire also might be used to create an “internal cast” to support the vertebral structure during the healing process.
Depending on the condition and your surgeon’s training, experience, and preferred methodology, an ALIF might be done alone or in conjunction with another spinal fusion approach. Please discuss the fusion approach options simply with the doctor, and rely on his or her judgment about which is most appropriate for your particular condition.
What conditions is Anterior lumbar interbody fusion used to treat?
- Anterior lumbar interbody fusion is used to treat a variety of conditions, You may be a candidate for Anterior lumbar interbody fusion if you have:
- Painful disc degeneration
- Spondylolisthesis
- Instability
- Spinal deformity or imbalance
- degenerative disc disease
- scoliosis or flat back syndrome
symptoms that have not enhanced with physical therapy or medication
You are not a candidate for Anterior lumbar interbody fusion if you have:
- problems that would prevent bone fusion
- significant prior abdominal surgery
- severe atherosclerosis of the aorta or an iliac vessel; peripheral vascular disease
- obesity (a weight loss plan is advised)
- severe osteoporosis
Fusion may help treat:
- Degenerative disc disease: the shrinkage and drying of discs with age. As the disc thins or herniates, the vertebrae bones rub and pinch a nerve.
- Spondylolisthesis: a forward slip of a vertebra out of its normal position. It could kink and compress the nerves, causing pain.
- Spinal stenosis: the narrowing of the nerve root canals and spinal canal. Enlarged facet joints and ligaments pinch the nerves leading to pain and numbness in the legs.
- Scoliosis: an abnormal curve of a spine caused by misalignment of the bones. In adults, this happens from aging discs, arthritis, or previous spine surgery.
What are the advantages of Anterior lumbar interbody fusion over other types of lumbar fusion?
Anterior lumbar interbody fusion is a very well-tolerated procedure and typically is associated with less pain and faster healing than spinal fusion surgery performed from the back of the spine. It allows the placement of a much larger cage than other types of spinal fusion, which provides more stability and has a higher chance of fusing solidly. It allows better correction of spinal deformity or imbalance, and this might be associated with better long-term outcomes in terms of pain, quality of life, and reduced chance of developing or creating problems at adjacent levels of the spine.
Anterior spine fusion has several advantages:
- A larger spacer device could be used, providing more support and a better chance of fusion.
- The path to the spine is from the front so there is less pain and disruption to a back muscle.
- Moving a forward-slipped L5 vertebra back into a normal position and restoring proper tilt (lordosis) is easier from the front.
- Anterior fusion allows the surgeon to avoid working surround the spinal nerves.
- The anterior lumbar interbody fusion is performed in a hospital setting. Patients commonly go home a day or two after surgery; recovery takes 6 to 12 weeks.
The anterior lumbar interbody fusion approach is just one of several approaches to spinal fusion. The primary benefit of using the Anterior lumbar interbody fusion approach is direct access to the front of the spinal column.
Relative to other fusion approaches, the advantages of choosing the Anterior lumbar interbody fusion approach include:
- Back muscles and nerves remain undisturbed
- The large spacer (spinal implant) might be used for improved stability of the fusion construct
- The bone graft is placed in compression opposite a large surface area of the endplates
- The natural curvature of the spine could be restored more efficiently and effectively
- There are specific disadvantages to the anterior approach as well. For eg, there is a risk of hernia after Anterior lumbar interbody fusion surgery. Whether a spine surgeon approaches the disc space from an anterior approach or/and one of the posterior approaches (PLIF or TLIF) is largely dependent on how comfortable the surgeon is with the anterior approach and operating surrounding the aorta and vena cava, which are large blood vessels attached to the heart.
- Most spine surgeons have not had a great deal of experience doing a procedure by themselves, and not all spine surgeons have access to a skilled vascular surgeon to help them with the approach. Therefore, a posterior approach for lumbar spine fusion surgery might be more practical for many surgeons.
Indications for Anterior Lumbar Interbody Fusion
The common indications for ALIF include:
- Severe lumbar (low back) pain or leg pain that is unresponsive to non-surgical treatment
- Degenerative disc disorder of the lumbar spine (pain due to damaged disc)
- Spondylolisthesis (slippage of one vertebra over another)
- Scoliosis (S-shaped curve of the spine)
- Fractures of the spine
- Tumors
- Spinal instability
What are the disadvantages of Anterior Lumbar Interbody Fusion?
A few patients may not be suitable for Anterior Lumbar Interbody Fusion – for eg, if they have had extensive abdominal surgery in the past, are quite overweight, or have unsuitable vascular anatomy.
What are the risks?
No surgery is without risks. In general complications of any surgery include bleeding, infection, blood clots (deep vein thrombosis), and reactions to anesthesia. The complications of ALIF surgery include infection, nerve damage, blood clots or blood loss, bowel and bladder problems, and any problem associated with anesthesia. The underlying risk of spinal fusion surgery is the failure of the fusion of vertebral bone and bone graft, which usually requires additional surgery.
What are the risks of surgery?
The risks are similar to other types of spinal fusion, including bleeding, infection, nerve damage, incontinence, paralysis, blood clots in the legs or lungs, stroke, and a very small risk of loss of the legs or death. Because the major blood vessels of an abdomen are nearby, there is a risk of major hemorrhage. In men, there is also a small risk of retrograde ejaculation- where a patient ejaculated into his bladder rather than outside. A hernia is also another potential complication.
Risks of Anterior Lumbar Interbody Fusion (ALIF)
Most Anterior Lumbar Interbody Fusion surgeries can be performed safely without any complications. However, like any surgical procedure, there are risks associated with both the anesthetic and the procedure itself.
Risks of Anaesthesia
Risks of anesthesia will be discussed with you by your anesthetist before surgery. You must inform us of your correct age and any past medical problems, as this can influence the risk of anesthesia. Risks include:
- Heart problems, such as arrhythmia or heart attack (AMI)
- Lung problems, such as blood clots or infection (pneumonia)
- Urinary tract infection
- Deep Venous Thrombosis (DVT)
- Eye or visual problems
- Pressure wounds
- Stroke
- Small risk of a significant life-threatening event
General Risks of Spine Surgery
However spine surgery is generally safe, but there are some risks whenever operations on the spine are performed. These include:
- Infection 1-2%
- Bleeding. This can happen at the time of surgery and may necessitate a blood transfusion. It can also happen a few times after surgery. Rarely another operation is required to drain the blood clot and stop the bleeding.
- Spine fluid leak (CSF leak)
- Small risk of significant neurological injury leading to paralysis
- Chronic pain
Specific Risks of Anterior Lumbar Interbody Fusion
The specific risks will be discussed in detail before your surgery but may include:
- Pain in the lower back
- Nerve injury causing pain, numbness, and weakness in the legs
- Nerve injury causing bowel or bladder problems
- Progressive deformity of the lumbar spine – spondylolisthesis or kyphosis
- Incomplete decompression of posterior pathology ( not able to reach the back of a spine)
- Persistent symptoms
- Recurrence of symptoms
- Adjacent segment disease – problems at the spinal levels next to a fused level
- Non-union – fusion not occurring
- Abdominal viscera Injury – bowel injury
- Vascular Injury – arterial or venous
- Ureteric injury
- Retrograde ejaculation
- Requirement for a second procedure from the back of the spine
Potential Risks and Complications with anterior lumbar interbody fusion Surgery
The principal risk of any spinal fusion surgery is that a solid fusion would not be obtained (nonunion). As with most spinal surgeries, an additional risk is a lack of or insufficient, pain relief for the patient. Risks and complications from an anterior lumbar interbody fusion (ALIF) approach tend to be relatively rare, reversible, and/or fleeting.
The majority of the known complications are related to the surgical approach from the front, which crosses or bypasses layers of the fat and the muscles, the internal organs, the nerves, and the blood vessels.
Constipation or Difficulty Eating After Surgery
Temporary constipation and/or dietary changes may happen during recovery in the days immediately following surgery. Around 3 days after Anterior Lumbar Interbody Fusion, patients might experience post-operative ileus, or constipation–a typical postoperative issue after abdominal surgery. This issue translates to not being able to eat solid food. This complication occurs in about 3% of Anterior Lumbar Interbody Fusion patients,1 but soon resolves on its own.
Infection or Incisional Hernia
The incision made when performing Anterior Lumbar Interbody Fusion surgery takes months of relative rest to heal fully. Without attentive care and rest, complications can happen. In about 2.6% of patients, the site of the incision could become infected or, rarely, develop a hernia.
An incisional hernia happens when the tissues of the abdominal lining begin to protrude outward and can be described as a lump or a bulge that might be more pronounced with activity. The standard treatment for the hernia is surgery to put the tissue back in place. An additional step to insert a surgical mesh might be required to prevent the tissue from protruding again.
Retrograde Ejaculation in Males
A risk unique to males is a condition called retrograde ejaculation. Approaching the L5 and S1 (lumbar segment 5 and sacral segment 1) disc space from the front creates this risk. The small nerves directly over the disc interspace control a valve that leads to ejaculation to be expelled during intercourse.
Dissection over the disc space may lead to the nerves stopping working, forcing the ejaculate to take the path of least resistance, which is up into the bladder. Retrograde ejaculation occurs in about 2% of cases and tends to resolve between 3 months to 4 years after surgery.
With retrograde ejaculation, the sensation of ejaculating is largely similar. Conception could become difficult, but this complication does not result in impotence because these nerves do not control erection. A surgeon might consider other approaches to spinal fusion surgery, such as PLIF, for younger male patients.
Bowel Obstruction or Abdominal Pain
Injury to the bowel or other bowel complications is infrequent, happening in as little as 0.25% of surgeries. During anterior lumbar interbody fusion surgery, the peritoneum (a large sack that holds the internal organs) might experience a rupture or abrasion, known as a serosal tear. Small serosal tears could be repaired during surgery, using absorbable or permanent stitches.
Blood flow to the intestines might be limited if a blood clot (embolism) lodges into one of the supplying arteries. If this complication happens, a patient might experience abdominal pain that gets worse after a meal. Treatment options for interrupting blood flow to the bowel include blood thinning medications or/and surgery.
All treatment and outcome results are specific to the particular patient. Results may vary. Complications such as infection, nerve damage, blood clots, blood loss, and bowel, and bladder problems, along with complications associated with anesthesia, are a few of the potential risks of spinal surgery. A potential risk inherent to spinal fusion is the failure of the vertebral bone and graft to properly fuse, a condition that may need additional surgery.
Please consult the physician for a complete list of indications, warnings, precautions, adverse effects, clinical results, and other important medical information that pertains to the anterior lumbar interbody fusion procedure.
Deep Vein Thrombosis After anterior lumbar interbody fusion Surgery
The risk of deep vein thrombosis (DVT) happens in up to 14% of cases,3 and is higher in people who have been diagnosed with iliac vein compression syndrome, also known as May-Thurner syndrome. The syndrome concerns the compression of the left iliac vein, between the L5 vertebrae and the right iliac artery. About 22% of individuals are expected to have this anatomical compression,4 of which may or may not lead to deep vein thrombosis during one’s lifetime.
Blood Loss After anterior lumbar interbody fusion Surgery
Anterior lumbar interbody fusion is performed close to the large blood vessels that go to the legs, creating the risk of vascular problems, such as blood loss or/and injured blood vessels.
The total blood loss is measured by calculating the estimated volume of blood loss during surgery and the hemoglobin level of the blood after the surgery. The difference between the total blood loss and the estimated blood loss is named hidden blood loss, which makes up about 40% of the total blood loss in both anterior and posterior approaches to surgery. Hidden blood loss might contribute to prolonged hospitalization and recovery.
This potential risk of damage to veins or arteries is an uncommon complication in a hands of experienced vascular and spine surgeons.
Specific complications related to anterior lumbar interbody fusion include :
Injury to abdominal organs. Because the surgical path passes via or closer to the bladder and/or the ureter, kidneys, part of the colon, and other vital organs, there is a small but real risk of damage to these structures. If the bladder or colon is harmed, added surgery would be needed.
Injury to large blood vessels. At the L4 and L5 levels, two major arteries and veins branch into the legs. If nicked, significant bleeding can happen. This complication happens in about 3% of patients.
Retrograde ejaculation ensues when semen flows into the bladder instead of out via the penis. During orgasm, you might ejaculate with very small or no semen. Retrograde ejaculation is not harmful, but it can lead to male infertility. The risk of damage to the small nerves during anterior lumbar interbody fusion surgery is about 1%.
Vertebrae fail to fuse. Common reasons why bones do not fuse contain tobacco and alcohol use, osteoporosis, obesity, diabetes, and malnutrition. Nicotine is a toxin that interferes with bone-growing cells. If the fusion does not heal (pseudoarthrosis), another surgery might be required for repair.
Hardware fracture. Metal tacks that stabilize the spine might move or break before the bones are completely fused. Another surgery might be required to fix or replace them.
Bone graft migration and settling. In a few cases, the bone graft moves from its proper position between the vertebrae soon after surgery. This more often happens if hardware (plates and screws) is not used or if fusion was for many vertebral levels. Over time, the bone graft spacer can potentially sink into the bone (subsidence) and lessen the indirect decompression. If migration or subsidence happens, another surgery may be needed to correct the problem.
Adjacent segment disease. Fusion leads to the transfer of added stress and loads to the discs and bones above or/and below the fusion segment. The added wear and tear can ultimately degenerate the adjacent discs and lead to pain.
Nerve damage or persistent pain. many spine surgeries come with the risk of injury to the nerves or spinal cord. Damage can lead to numbness or even paralysis. The most common lead to persistent pain is nerve damage from the disc herniation itself. If the damage was permanent, the nerve could not respond to surgical decompression. Dislike memory foam, for example, the compressed nerve does not spring back. In such cases, spinal cord stimulation or another treatment may provide relief.
Restrictions
- Avoid bending/twisting the back.
- Don’t lift anything heavier than 5 pounds.
- No strenuous activity, including housework, yard work, and sex.
- Do not smoke, vape, dip, chew, or/and use nicotine products. It stops new bone growth and may cause your fusion to fail.
- Don’t drive until after the follow-up appointment.
- Don’t drink alcohol. It thins the blood and raises the risk of bleeding. Also, do not mix alcohol with pain medicines.
Incision Care
- Wash your hands before and after cleaning the incision to control infection.
- If Dermabond skin glue covers the incision, you might shower the day after surgery. Gently wash the area or part with soap and water each day. Do not rub or pick at the glue. Pat dry.
- If you have staples, steri-strips, or/and stitches, you may shower 2 days after surgery. Gently wash an area with soap and water every day. Pat dry.
- If there is drainage, cover an incision with a dry gauze dressing. If drainage soaks via two or more dressings in a day, call the office.
- Do not soak the incision in a bath, pool, or tub.
- Don’t apply lotion/ointment on the incision.
- Dress in clean clothes after each shower. Sleep with clean bed linens. No pets in the bed until the incision heals.
- A few clear, pinkish drainage from the incision is normal. And Watch for spreading redness, colored drainage, and separation.
- Staples, steri-strips, and stitches will be removed at the follow-up appointment.
- Apply an antibiotic cream or ointment, such as Aquaphor or Vaseline, to the incision site, and keep it covered with appropriate bandaging to prevent dirt, bacteria, and other irritants from entering the wound. A moist environment helps the cells to replicate and properly bond together to close up the incision faster.
Medications
- Take pain medicines as directed by your surgeon. Decrease the amount and frequency as your pain subsides. If you don’t require pain medicine, do not take it.
- Narcotics can also lead to constipation. Eat high-fiber foods and plenty of water. Laxatives and stool softeners such as Dulcolax, Senokot, Colace, and/or Milk of Magnesia are over-the-counter options.
- If painful constipation does not get better, call a doctor to discuss other medicine.
- Do not take anti-inflammatory pain relievers (Advil, Aleve) without the surgeon’s approval. They prevent new bone growth and may lead to fusion to fail.
- You may take acetaminophen (Tylenol).
Activity
- Ice your incision 3-4 times per day for 15-20 minutes to relieve pain and swelling.
- Do not sit or lie in one position longer than an hour unless you are sleeping. Stiffness leads to more pain.
- Get up and walk five to ten minutes every 3-4 hours. Gradually raise your walking time, as you are able.
- If you were given a brace, wear it at every time except when sleeping, showering, or icing the incision.
When to Call the Doctor
- Fever over 101.5° (unrelieved by Tylenol).
- Unrelieved nausea or pain.
- Unable to urinate six to eight hours after surgery despite having a full bladder.
- Signs of incision infection.
- Rash or itching at an incision (allergy to Dermabond skin glue).
- Swelling and tenderness in the calf of one leg (the sign of a blood clot).
- New onset of tingling, numbness, or weakness in the arms or/and legs.
- Dizziness, confusion, nausea, or excessive sleepiness.
Recovery and prevention
Schedule a follow-up appointment with the surgeon for two weeks after surgery. Recovery time to daily activities is generally 6 to 12 weeks. X-rays may be taken after several weeks to verify that fusion is happening. The surgeon will decide when to release you back to work at the follow-up visit. Fusion takes time. Follow the “BLT” of spine surgery recovery by limiting the bending, lifting, and twisting for 2 to 3 months. Work modifications may be necessary.
The surgical decision
If you are a candidate for spinal fusion, the surgeon would explain the options. Consider all the risks and advantages as you make the decision. Fusion is performed only after another treatment has been explored. It will stop the motion in the painful area of the spine, allowing raised function and a return to a more normal lifestyle though one that may not be pain-free.
The surgeon would also explain the various types of bone grafts. This material is placed within the remaining disc space and acts as a kind of mortar between the bones as your body heals. All type has advantages and disadvantages.
- Autograft is your living bone. The marrow contains bone-growing proteins. It could be collected from drillings during the surgery or carried from the hip as an iliac crest bone graft. A harvested bone is about half an inch thick. The entire thickness of the bone is not removed, just the top half layer.
- Bone marrow aspirate(BMA) is the living bone marrow, collected with a syringe from the hip (iliac bone) or/and vertebra. It is relatively painless or/and pain-free compared to the iliac crest graft.
- The Allograft is a bone from an organ donor, collected and stored by the bone bank. A donor graft has no bone-growing cells.
- A cellular bone matrix is an allograft from an organ donor that contains bone-growing stem cells. A putty is shaped and added to grafts.
- BMP (bone morphogenetic protein) is a few times added to bone-graft material to stimulate bone growth naturally in the body.
Who performs the procedure?
A neurosurgeon or orthopedic surgeon, along with a vascular surgeon, performs (Anterior Lumbar Interbody Fusion) ALIF surgery. Many spine surgeons have specialized training or practice in minimally invasive surgery. Ask the surgeon about his or her training, particularly if your case is complex or you have had previous spinal surgery.
What do I need to do before surgery?
Before surgery, we will likely arrange for a few prehabilitation with one of our exercise physiologists or physical therapists. This is to get you into the best shape possible for the surgery. If persons are overweight, then you should do your best to shed any excess weight. If you smoke, then you should stop. If you take aspirin, warfarin, or other anticoagulants, then you should advise the team at Precision Brain Spine and Pain Centre so we could let you know when and how to stop these.
What happens before surgery?
In the office, you will sign consent forms and provide the medical history (allergies, medicines/vitamins, bleeding history, anesthesia reactions, previous surgeries). Inform the healthcare provider about all the medications (over-the-counter, prescription, herbal supplements) that you are taking. Presurgical tests (e.g., blood test, electrocardiogram) may require to be done several days before surgery. Consult the primary care physician about stopping certain medications and ensure you are cleared for surgery.
Continue taking the medications the surgeon recommends. Stop taking all non-steroidal anti-inflammatory medicines (ibuprofen, naproxen, etc.) and blood thinners (Coumadin, aspirin, Plavix, etc.) seven days before surgery.
You may be asked to wash the skin with Hibiclens (CHG) or Dial soap before surgery. It kills bacteria and decreases surgical site infections. Avoid getting CHG in the eyes, ears, nose, or genital areas or parts.
Stop smoking and drinking before surgery
The most important way to achieve a successful spine fusion is to stop tobacco use (cigarettes, vaping, cigars, pipes, chewing tobacco, and snuff/dip) before surgery.
Nicotine stops bone growth and decreases successful fusion. Smoking risk is serious: fusion fails in 40% of smokers compared with 8% of non-smokers. Smoking also reduces blood circulation, resulting in slower wound healing and increased risk of infection. Talk with the doctor about ways to help you quit smoking: nicotine replacements, medications (Chantix or Zyban), and tobacco counseling programs.
You should not drink alcohol one week before and two weeks after surgery to avoid bleeding problems.
Morning of surgery
- Don’t eat or drink after midnight before surgery (unless a hospital tells you otherwise). You might take permitted medicines with a small sip of water.
- Shower using antibacterial soap. Dress in freshly washed, and loose-fitting clothing.
- Wear flat-heeled shoes with closed backs.
- Remove the make-up, hairpins, contacts, body piercings, nail polish, etc.
- Leave all valuables and jewelry at the home.
- Bring a list of medications with dosages and the times of day generally taken.
- Bring a list of allergies to medication or/and foods.
- Arrive at the hospital 2 hours before the scheduled operation to complete the necessary paperwork and pre-procedure work-ups. An anesthesiologist would talk with you and explain the effects of anesthesia and its risks.
What happens during surgery?
This surgery commonly takes one to two hours, depending on how many spine levels are treated.
Anterior Lumbar Interbody Fusion (ALIF) is a major spinal fusion surgery performed through a patient’s abdominal cavity. The surgery is performed using large metal instruments with a tremendous force near major blood vessels, nerves, bladder, and intestines. The surgery is performed utilizing general anesthesia. A breathing tube (endotracheal tube) is placed and a patient breathes with the help of a ventilator during the surgery. Preoperative intravenous antibiotics are given.
An Anterior lumbar interbody fusion is a spinal operation where a spine is approached from the front relatively than from the back. It is performed through an abdomen, generally with the assistance of a vascular surgeon to move the major blood vessels out of the way. The disc is removed and pressure on the nerve can be relieved or eased. Depending on the location and extent of the surgery, you may experience some pain and discomfort but the pain can typically be controlled well with medications. After you go home, contact the doctor if you exhibit signs of infection, such as Redness, tenderness, or swelling. Wound drainage.
Step 1: prepare the patient and doctors
Patients will be positioned in the supine (lying on the back) position on the operating table and be given anesthesia., generally using a special, radiolucent operating table. The surgical region (abdominal area or region) is cleansed with a special cleaning solution. Once asleep, the belly is cleansed and prepped.
Sterile drapes are placed, and the surgical team wears sterile surgical attire such as gowns and gloves to maintain or keep a bacteria-free environment.
Step 2: make the incision
An x-ray fluoroscope or/and image guidance is used to plan an approach. The vascular surgeon makes a two to the three-inch incision in the belly at the specific disc level.
A three to eight cm (depending on the number of spinal levels to be fused) transverse or oblique incision is made just to the left of an umbilicus (belly button). An abdominal muscle is gently spread apart but is not cut. The peritoneal sacs (containing an intestine) are retracted (moved to the side) to the side, as are the large blood vessels. particular retractors are permitted to allow a surgeon to visualize the anterior (front part) aspect of the intervertebral discs. After the retractor is in place, an x-ray is used to establish that the proper spinal level(s) is identified.
Step 3: locate the damaged disc
A vascular surgeon gently clears a path between the abdominal cavity and the retroperitoneal space. The intestines are protected in a peritoneum sac, which is temporarily moved to the right side of the belly. The veins and arteries overlying the damaged discs are gently moved and held aside.
Step 4: remove the disc
Next, the spine surgeon removes the damaged disc. The number of discs removed depends on how many spine levels are affected or involved. The distractor instrument is inserted to open the collapsed disc space. Bone shavers prepare the fusion bed.
The intervertebral disc is then removed using special biting and grasping instruments such as pituitary rongeur, Kerrison rongeur, and curettes. Special distractor instruments are used to restore the normal height of a disc, as well as to determine the appropriate size spacer to be placed.
Step 5: Prepare the disc space
The open disc space is measured, and The spacer size is selected. A trial spacer is slid into the empty disc spaces. The x-ray is taken to confirm that the depth, the placement, and the wedge angle create sufficient height and decompress the nerves.
A bone spacer (metal or plastic spacers may also be used) is then carefully put in the disc space. Fluoroscopic x-rays are taken to confirm that. When a good fit is made, the bone graft materials are prepared for the fusion. The mortar-like paste includes bone-growing proteins that are packed into the permanent bioplastic spacer cage.
Step 6. insert the bone graft
Guided by x-ray fluoroscopy, A permanent spacer graft is inserted into an empty disc space, pushing the two bones separated to restore normal disc height.
Step 7. insert plate and screws (optional)
The spacer graft might be held in place with screws or/and with a metal plate that is screwed into the front of the vertebrae. In a few cases, the patient might be turned over so that pedicle screws and rods can be inserted from the back. The hardware provides stability during fusion.
Step 8. close the incision
The instruments are removed and the peritoneum re-expands into its natural position or/and normal position. The abdominal muscles are closed with sutures. The skin incision is closed or near with skin glue (dermabond).
The wound area is commonly washed out with sterile water containing antibiotics. The deep fascial layers and subcutaneous layers are closed with a few strong sutures. The skin can generally be closed using special surgical glue, leaving a minimal scar and needing no bandage.
Cleaning an incision:- Gently clean it with soap and water to remove the crust. Do not scrub or soak a wound. Do not use rubbing alcohol, hydrogen peroxide, or/and iodine, which can harm the tissue and slow wound healing. Air-dry the incision or pat it dry with a clean, fresh towel before reapplying the dressing.
The total surgery time is approximately two to three hours, depending on the number of spinal levels involved.
What happens immediately after surgery?
It is usual to feel some pain after surgery, particularly at the incision site. Pain medications are generally given to assist in the control of the pain. While tingling sensations or numbness is common, and should decrease over time, they should be reported to the neurosurgeon. Most patients are up and moving around within more hours of surgery. This is encouraged to maintain circulation normal and avoid blood clot formation in the legs. You would be able to drink after around 24 hours, depending on how quickly the bowels start contracting and when you start passing wind. The CT scan will be performed the next day to check the position of the screws and cage.
You will be discharged home when you are comfortable, generally after a short period of inpatient rehabilitation. You would awaken in the postoperative recovery area. The blood pressure, heart rate, and respiration would be monitored. Any pain will be addressed. Once awake, you can start a gentle movement (sitting in the chair, walking). Patients generally go home the next day. Be sure to have a few at home to help you for the first 24 to 48 hours.
What do I need to tell my surgeon about after the operation?
You should notify your neurosurgeon and should also see your GP if you experience any of the following after discharge from a hospital:
- Increasing leg pain, weakness, or numbness
- Worsening back pain
- Problems passing urine or controlling the bladder or the bowels
- Problems with your walking or balance
- Fever
- Swelling, redness, raised temperature, or suspected infection of the wound
- Leakage of fluid from the wound
- Pain or swelling in your calf muscles (ie. below your knees)
- Chest pain or shortness of breath
- Any other concerns
Why Do I Need This Procedure?
There are many reasons the surgeon may recommend spinal fusion. This procedure is commonly used to treat.
- One or more fractured (broken) vertebrae
- Spondylolisthesis (slippage of one vertebral bone over another vertebral bone)
- Abnormal curvatures of the spine,( such as kyphosis or/and scoliosis )
- Protruding or degenerated discs (the cartilaginous “cushions” in between vertebrates)
- Instability of the spine (an abnormal or excessive motion between two or more vertebrae)
- Patients with low back and/or leg pain due to degenerative disc disease(DDD), spondylolysis/spondylolisthesis, scoliosis, or other spinal instability that have not responded to non-surgical treatment measures (rest, physical therapy, or medications) might be suitable candidates for anterior lumbar interbody fusion.
Patients without an excessive amount of spinal instability or/and slippage, and who have little to no spinal stenosis or nerve compression in the back of the spine, are generally the best candidates for an anterior lumbar interbody fusion alone. Although, anterior lumbar interbody fusion as a stand-alone technique is generally not recommended for people whose bones have become very soft due to osteoporosis, or in patients with instability or arthritis.
A surgeon will consider several factors before recommending an anterior lumbar interbody fusion, including the condition to be treated, your age, health and lifestyle, and the anticipated level of activity following surgery. Please discuss this treatment option thoroughly with the spinal care provider.
How Long Will It Take Me To Recover?
The recovery period for a spinal fusion procedure such as an anterior lumbar interbody fusion would vary, depending on the procedure and the body’s ability to heal and firmly fuse the vertebrae. One advantage of an anterior lumbar interbody fusion is that the back muscles and nerves are undisturbed.
Patients typically stay in the hospital for many days, longer if necessary for more extensive surgery. This might also include time in a rehabilitation unit. the surgeon will prescribe pain medication as required and may recommend a brace and follow-up physical therapy.
The length of time you would be off work will depend on many factors: The particular procedure and the physician’s approach to the spine, the size of the incision, and whether or not they experienced any significant tissue damage or complications. another consideration is the type of work the plan is to return to. generally, you can expect to be on medical leave for 3 to 6 weeks; Although many innovations and advancements have been developed in the last few years that allow for improved fusion rates, shorter hospital stays, and an additional active and rapid recovery period.
Work closely with the spinal surgeon to determine the appropriate recovery protocol for you, and follow his or/and her instructions to optimize the healing process.
Post-Operative Care
Mainly patients are generally able to go home 3-4 days after surgery. Patients will usually stay longer, approximately four to seven days, if a posterior spinal surgery is also performed. Before patients go the home, the occupational therapists and the physical therapists work with the patients and instruct them on proper techniques for getting in and out of the bed and walking independently. Patients are instructed to stop bending at the waist, lifting more than five pounds, and twisting in the early postoperative period (first 2-4 weeks) to avoid a strain injury. Patients can slowly begin to bend, twist, and lift after four to six weeks as the pain subsides and the back muscles get stronger.
Sit with both feet flat on the ground (you may require to use a low stool). The hips should be just higher than your knees, and you should have equal weight through both hips. With the hips at the back of the chair, the front of the seat should not place pressure on the backs of the knees or calves.
Just like sleeping on the back, sleeping on the side helps decrease pain and pressure. Try to alternate between sleeping on the left side and right side to distribute the pressure and benefit the spine’s alignment. Right after surgery, you can also place a pillow under or in between the knees.
While it might seem easy to climb stairs a few days after surgery, this motion can put undue stress on the spine and slow down your recovery. You can go upstairs in a couple of weeks following surgery, but it is best to limit stairs to once or twice a day in the first few weeks.
You should tell your employer you would be out of work for approximately eight to twelve weeks but may be able to return earlier than that. Walking is the best exercise you can do for the first six weeks after surgery. You should begin out slowly and work up to walking 30 minutes at least twice a day.
Brace
Patients are generally not needed to wear a back brace after surgery. Occasionally, a few patients may be issued a soft or rigid lumbar corset that can provide more lumbar support in the postoperative period, if necessary.
Wound Care
The wound area or part can be left open to the air. No bandages are needed. That area shall be kept clean and dry. Unless advised otherwise, the sutures will be dissolvable and not require to be removed. You must keep the wound dry for one week following the surgery. You will be provided with waterproof dressings. You can shower with this dressing on and then replace it following a shower, or when it is soiled. It is important not to have any restrictive clothing which is tight to surround the wound or rub on the wound. Any increasing wound pain or swelling, or any evidence of redness, heat, discharge, fluid leakage, wound breakdown, or signs of infection, should be urgently reported to the local doctor. After seven days, you can get a wound wet. It is best not to scrub or rub a wound in a shower. After two weeks, you can swim and get the wound completely immersed in water. You should keep the wound dry for three weeks after the surgery- showering is fine as long as you use a waterproof dressing. After three weeks, you could take a bath and start hydrotherapy. the staples should be removed twelve days postoperatively, and we would give you instructions about how this should be done and who to have them removed by.
Shower/Bath
Patients can shower immediately after surgery but should keep the incision area covered with a bandage and/or tape, and try to avoid the water from water hitting directly over the surgical area. After the shower, patients should remove a bandage, and dry off the surgical area or part. Patients should not take a bath until the wound has fully healed, which is typically around 2 weeks after surgery.
Driving
Patients may begin driving when the pain has decreased to a mild level, which usually is between seven to fourteen days after surgery. Patients should not drive while taking pain medicine (narcotics). When driving for the first time after surgery, patients should make it a short drive only and have somebody come with them, in case the pain flares up and they need help driving back home. After patients feel comfortable with a short drive, they can start driving longer distances alone.
Return to Work and Sports
Patients may return to light work duties as early as two-three weeks after the surgery, depending on when the surgical pain has subsided. Patients may back to moderate-level work and light recreational sports as early as 3 months after surgery if the surgical pain has subsided and the back strength has returned appropriately with the physical therapy. Patients who have undergone a fusion at only one level might return to heavy lifting and sports activities when the surgical pain has subsided and the back strength has returned appropriately with physical therapy. Patients who have undergone fusion at two or more levels are commonly recommended to avoid heavy lifting, laborious work, and impact sports.
Doctor’s Visits and Follow-Up
Patients will return for a follow-up visit to see a doctor approximately 12 to 14 days after surgery. The incision would be inspected. There are no sutures to be removed from an anterior wound. Medications will be refilled if necessary. Patients will commonly return to see Doctore every four to six weeks thereafter, and an x-ray will be taken to confirm the fusion area is stable and healing appropriately. At 8-12 weeks after surgery, patients will be given a prescription to start physical therapy for gentle back exercises.
What else happens after discharge?
You will require to take it easy for 8 weeks but should walk for at least an hour every day. You should avoid sitting for more than 15 to 20 minutes continuously during this time. At 6 to 8 weeks you will likely be able to return to work on “light duties” and to drive a motor vehicle on short trips. This, and the step-wise progression in the physical activities, will be determined on an individual basis. Bear in mind that the amount of time it takes to back to normal activities is different for every patient. Discomfort should decrease a little each day. Increases in energy and activity are signs that the post-operative recovery is progressing well. Maintaining a positive attitude, a healthy and well-balanced diet, and ensuring plenty of rest are excellent ways to speed up recovery.
Signs of infection such as swelling, redness or discharge from an incision, and fever should be brought to a surgeon’s attention immediately. You will be reviewed after 6 to 8 weeks by your neurosurgeon. Until then, you should not lift objects weighing more than 2kg-3kg, and should not engage in bending or twisting movements. The results of fusion surgery are not as good in patients who smoke or are very overweight or obese. It is therefore important that you give up smoking permanently before the surgery and try to lose as much weight as possible. You should continue wearing the TED stockings for a couple of weeks after surgery.
What do I need to do after I go home?
We will give you specific instructions. In general, walking for at least an hour in total every day soon after the surgery is enabled. You may need a short period (of around a week) of inpatient rehabilitation, but this is not always essential. Your pain medications will be gradually decreased. Outpatient rehabilitation with our exercise physiologists and physical therapists is also often recommended.
Results and Outcome Studies
The results of anterior lumbar interbody fusion surgery in the treatment of symptomatic spondylolisthesis and degenerative disc disease are commonly excellent. Numerous research studies in medical journals demonstrate greater than 87-97% good or excellent results from anterior lumbar interbody fusion surgery. mainly patients are noted to have a significant improvement in their back pain and return to many, if not all, of their normal daily and recreational activities.
Track the surgeon’s home care instruction or pedagogy for 2 weeks after surgery or until the follow-up appointment. In general, you can expect:
- Post-Operative Care and Instructions Following ALIF(anterior lumbar interbody fusion) Spinal Fusion
- Postoperative Care for Anterior Spinal Fusion – ALIF(anterior lumbar interbody fusion)
- The following information is provided to assist and maximize recovery following your anterior spinal fusion surgery (ALIF).
What are the results?
Anterior lumbar fusion avoids incisions of the back muscles, has a short operating time and poses a few serious difficulties. With its tiniest trauma to the spine and nearby tissues, patients repeatedly return to daily activities within 6 weeks. Each patient’s consequence and recovery counters based on his or her health and lifestyle. Keep a positive attitude and perform your physical therapy as required.
The anterior lumbar interbody fusion surgery reduces painful pinched nerves by indirect decompression. By increasing the height of the disc space, more room is created for the nerves to move voluntarily in the canals. The surgeon does not see or touch the spinal nerves with tools. By comparison, in a TLIF or PLIF surgery, the nerves are relaxed under direct vision.
Conducting a successful spinal fusion goes, depending on the method used, your available health, and whether you smoke.
Treatment & Benefits
anterior lumbar interbody fusion (ALIF) is commonly performed for a variety of painful spinal disorders, such as spondylolisthesis and degenerative disc disease, among others. Fusing provides a high degree of stability for the spine and a large surface area for bone fusion to happen. Approaching both sides of the spine frequently allows for a more aggressive reduction for patients who have a deformity in the lower back (e.g. isthmic spondylolisthesis). A few spine surgeons feel that if stabilization is achieved both through an anterior and a posterior approach, patients can be mobilized earlier in the postoperative period. Studies have shown that fusing both sides of a spine in the lower back does lead to a very high fusion rate (greater than 95% of these cases will achieve a solid fusion).
Recovery of Anterior Lumbar Interbody Fusion
The post-surgical hospitalization includes a rehabilitation program. If needed, a surgeon may prescribe pain medications or a brace and follow-up physical therapy upon discharge.
The recovery period after anterior lumbar interbody fusion surgery depends on the body’s healing capacity. The success of surgery depends on different factors such as age, spinal condition, overall health status, and activity level of the individual. A period of rest or inactivity depends on a few factors such as the type of surgical procedure and the approach used to access your spine, the size of an incision, and the presence of any complications.
Back to work or normal activity depends on the type of work or activity the plan is to perform. typically, three to six weeks is the ideal time for healing. With advanced and innovative techniques, it is now possible to achieve improved fusion rates, shorter hospital stays with an active and rapid recovery period. Strictly adhere to the postoperative instructions suggested by the spine surgeon to promote healing and decrease the possibility of postoperative complications.
What are the outcomes of anterior lumbar interbody fusion?
In well-selected patients, the outcomes are typically quite good. 70-80% of patients should obtain a good outcome.
What are the implications of surgery?
Mainly patients are admitted on the same day as their surgery; Although, a few patients are admitted the day before. Patients admitted the day before surgery have those who: reside in country regions, interstate, or overseas; have complex medical conditions or who take warfarin; need further investigations before their surgery; are first on an operating list for a day. You would be given instructions about when to stop drinking and eating before admission.
You will be in the hospital for between two and four days after the surgery. You will be given instructions about any physical restrictions that would apply following surgery, and these are summarised later in this section. More X-rays of your back will be taken during surgery to make sure that the correct spinal level is being fused, and also to optimize the positioning of the cage and screws. You must inform us if you are pregnant or think you could be pregnant, as X-rays may be harmful to the unborn child. There is significant variability between patients in terms of the outcome of surgery, as well as the time taken to recover. You would be given instructions about physical restrictions, as well as your back to work and resumption of recreational activities. You should not drive the motor vehicle or operate heavy machinery until instructed to do so by a neurosurgeon. You should not sign or witness legal documents until reviewed by your GP post-operatively, as the anesthetic can few times temporarily muddle your thinking.
Recurrences of pain are common. The key to preventing recurrence is prevention:
- Proper lifting techniques
- Good body mechanics and posture during standing, sitting, moving, and sleeping
- Appropriate exercise program
- An ergonomic work area
- Healthy weight and lean body mass
- The positive attitude and relaxation techniques (e.g., stress management)
- A healthy diet of whole, unprocessed foods
- No smoking
Other anterior lumbar interbody fusion Considerations
In general, the principal risk of this type of spine surgery is that a solid fusion will not be obtained (nonunion) and further surgery to re-fuse the spine may be required. Fusion rates for an anterior lumbar interbody fusion are generally as high as 90% to 95%.
Nonunion rates are higher for patients who:
- Have had prior lower back surgery
- Smoke or are obese
- Have multiple-level fusion surgery
- Have been treated with radiation for cancer
- Not all patients who have a nonunion will require to have another fusion procedure. As long as the joint is stable and the patient’s symptoms are good, more back surgery is not necessary.
DISCLAIMER:
This article is intended or purposeful for your general informational purposes only and does not address particular circumstances. it is not a substitute for professional advice(or guidance) or help( or assistance) and should not be relied on to make decisions of any kind. A few or any actions you take upon the information presented in this article are strictly at your own risk and responsibility.
FAQs
What Should I Expect from Surgery?
Patients might notice an improvement in a few or all symptoms and pain from surgery may diminish between two to four weeks after surgery. However, recovery time varies between patients. It is the surgeon’s goal for the patient to back to normal activities as soon as possible. A positive attitude, reasonable expectations, and compliance with post-surgery instructions all assist to contribute to a satisfactory outcome.
What to expect after Anterior lumbar interbody fusion?
After surgery, you can expect the back to feel stiff and sore. You may have trouble sitting or standing in one position for a very long and may require pain medicine in the weeks after the surgery. It may take four to six weeks to get back to doing simple activities, such as light housework.
How soon can you walk after Anterior lumbar interbody fusion surgery?
Most people are up and walking immediately following anterior lumbar interbody fusion surgery. Although, you should still expect to generally stay overnight in the surgery center. More complex cases sometimes need a longer hospital stay
How is an Anterior lumbar interbody fusion done?
An Anterior lumbar interbody fusion is a spinal operation where a spine is approached from the front relatively than from the back. It is performed through an abdomen, generally with the assistance of a vascular surgeon to move the major blood vessels out of the way. The disc is removed and pressure on the nerve can be relieved or eased.
Is lumbar fusion surgery painful?
Depending on the location and extent of the surgery, you may experience some pain and discomfort but the pain can typically be controlled well with medications. After you go home, contact the doctor if you exhibit signs of infection, such as Redness, tenderness, or swelling. Wound drainage.
How long do you wear a back brace after Anterior lumbar interbody fusion surgery?
You would require to wear a brace at all times when you are up, for 3 months following surgery. You might remove the brace for brief periods to shower and attend to personal hygiene but remember to maintain your back in a neutral position and avoid any bending.
Can you climb stairs after Anterior lumbar interbody fusion surgery?
While it might seem easy to climb stairs a few days after surgery, this motion can put undue stress on the spine and slow down your recovery. You can go upstairs in a couple of weeks following surgery, but it is best to limit stairs to once or twice a day in the first few weeks.
How do you sit after Anterior lumbar interbody fusion surgery?
Sit with both feet flat on the ground (you may require to use a low stool). The hips should be just higher than your knees, and you should have equal weight through both hips. With the hips at the back of the chair, the front of the seat should not place pressure on the backs of the knees or calves.
How do you sleep after Anterior lumbar interbody fusion surgery?
Just like sleeping on the back, sleeping on the side helps decrease pain and pressure. Try to alternate between sleeping on the left side and right side to distribute the pressure and benefit the spine’s alignment. Right after surgery, you can also place a pillow under or in between the knees.
How long does nerve pain last after Anterior lumbar interbody fusion surgery?
A few times this is a temporary condition as the nerve root or roots take time to heal. This can take days to weeks. If the pain is still there after three months, it is unlikely to improve on its own.
What can you not do after Anterior lumbar interbody fusion surgery?
Change the positions often and avoid just lying, standing, or sitting for long periods during the day. If you do any activity or exercise that increases your pain, stop it immediately.
Is an Anterior Lumbar Interbody Fusion considered major surgery?
Anterior Lumbar Interbody Fusion (ALIF) is a major spinal fusion surgery performed through a patient’s abdominal cavity. The surgery is performed using large metal instruments with a tremendous force near major blood vessels, nerves, bladder, and intestines.
How long does leg pain last after Anterior lumbar interbody fusion surgery?
You would feel the initial post-operative soreness for at least a few weeks after surgery and that is commonly how long it can take to return to desk/office-type work. More physical work might require up to six weeks of recovery to feel up to that level of activity.
How long will I require a walker after spinal fusion?
You will require an assistive device such as a walker or cane for the first week; although, you should strive to limit the use of this device after the first two to three weeks when you are on a stable floor.
How long is bed rest after spinal fusion?
You should tell your employer you would be out of work for approximately eight to twelve weeks but may be able to return earlier than that. Walking is the best exercise you can do for the first six weeks after surgery. You should begin out slowly and work up to walking 30 minutes at least twice a day.
Should I stay in bed after spinal fusion?
You don’t require to fear being bedridden for weeks after spinal surgery since it’s of the utmost importance to your post-surgical recovery to get up very soon. Movement is crucial to proper healing after spinal surgery, so you can expect to get out of bed the same day or the very next day after surgery.
Which activities can you not do after spinal fusion?
Activity Precautions
No matter what type of back surgery you are undergoing, and no matter how well-controlled the pain is, it’s vital that you avoid bending, lifting, and twisting. Bending from a waist, lifting more than 10 pounds, and twisting your torso all put undue pressure on the vulnerable spine.
How do you care for an incision?
Cleaning an incision
Gently clean it with soap and water to remove the crust. Do not scrub or soak a wound. Do not use rubbing alcohol, hydrogen peroxide, or/and iodine, which can harm the tissue and slow wound healing. Air-dry the incision or pat it dry with a clean, fresh towel before reapplying the dressing.