Total Hip Replacement
Introduction
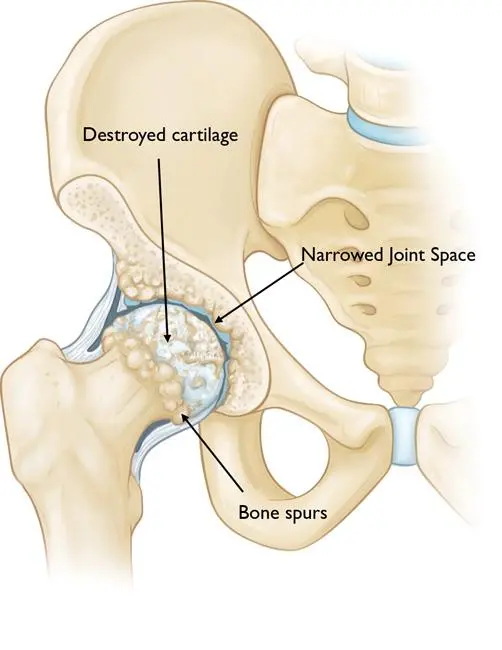
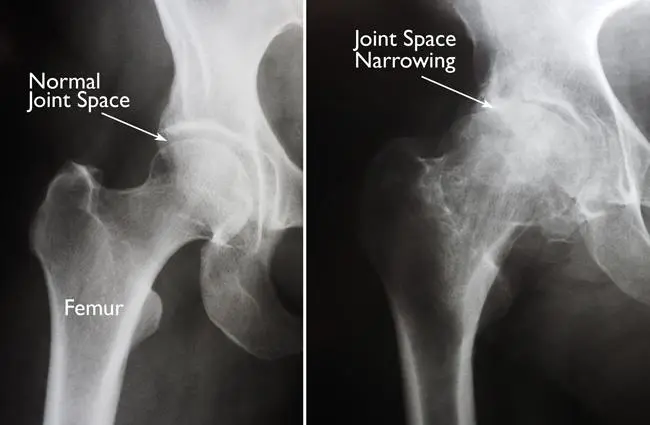
Total hip replacement, also known as total hip arthroplasty, is a surgical procedure in which a damaged or diseased hip joint is replaced with an artificial joint called a prosthesis. This procedure is typically performed to relieve pain and improve mobility in individuals who have severe hip joint damage due to conditions such as osteoarthritis, rheumatoid arthritis, avascular necrosis, or hip fractures.
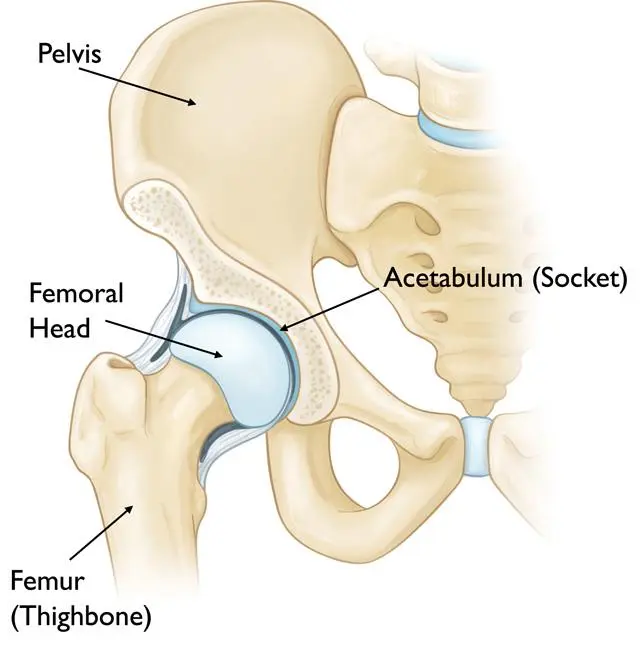
Anatomy of the Hip Joint:
Indications of Total Hip Replacement
Contraindications of Total Hip Replacement
Clinical Evaluation for THR
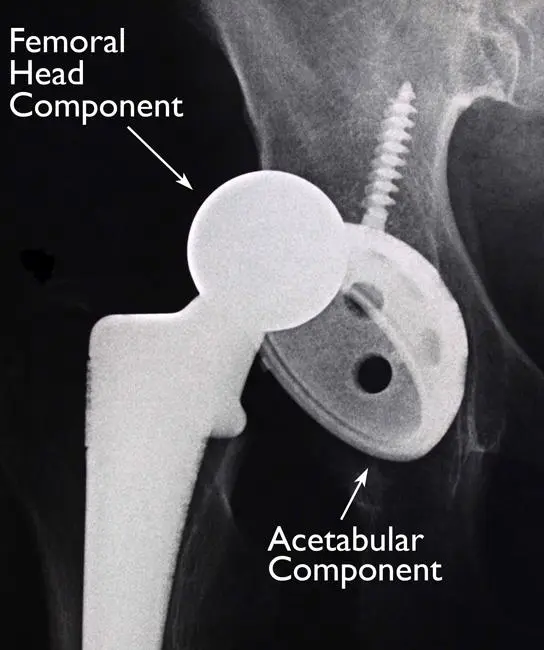
Which Prosthesis is used in Total Hip Replacement?

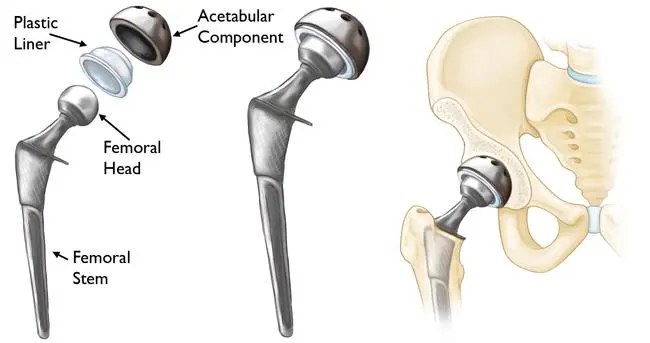
When accomplishing a total hip replacement the ball is extracted, the socket is reshaped, and the artificial implant is arranged in the bone. The implant may be kept in the bone by tightly wedging it in place/cementing it into position. The kind of fixation utilized relies on the bone health of individuals and the structure of the implant. Co-occurring total hip replacement methods have developed into press-fit femoral and acetabular elements, and many deviations exist. The primary elements are:
- Bearing surfaces are the surfaces that articulate in the prosthetic joint. The femoral head and the acetabular liner can be utilized in various mixtures. These will provide additional impressions on radiographs relying on the composition. Many possibilities are available for example Metal-on-polyethylene, Ceramic-on-polyethylene, Ceramic-on-ceramic, and Metal-on-metal.
- The femoral part or stem guides to the prosthesis which is injected into the femur. They can be defined by length, taper, and the sight of a coupling. Associated with the femoral element are the neck & head which in prostheses can be changed in size to build a steady hip joint.
- Prosthesis fixation femoral stem fixation can be either cemented/non-cemented (natural) fixation. Majority of fixation method: an increasing tendency towards cementless fixation.
Types of Total Hip Replacement
There are several kinds of total hip joint replacement, containing:
- Cemented hip replacement: This kind of hip replacement implicates utilizing unique bone cement to affix the synthetic joint parts to the remaining bone. A cemented hip replacement is generally utilized in more aged patients or those with more fragile bones.
- Uncemented hip replacement: In an uncemented hip replacement the synthetic joint parts are developed to affix straight to the bone without the usage of cement. This kind of hip replacement is usually utilized in younger patients or those with powerful bones.
- Hybrid hip replacement: A hybrid hip replacement implicates utilizing both cemented & uncemented elements in the same operation. For instance, the femoral part may be uncemented while the acetabular cup is cemented.
- Metal-on-polyethylene: In this kind of hip replacement, the ball segment of the synthetic joint is constructed of metal, and the socket element is constructed of polyethylene, a kind of plastic. This hip joint replacement is considerably normally operated.
- Ceramic-on-polyethylene: Comparable to metal-on-polyethylene, the ball element of the synthetic joint is constructed of ceramic, and the socket element is constructed of polyethylene. Ceramic-on-polyethylene hip replacements may have more down wear rates analogized to metal-on-polyethylene hip replacements, but they may likewise be more breakable and inclined to fracture.
- Metal-on-metal: In a metal-on-metal hip replacement, both the ball & socket elements are constructed of metal. This kind of hip replacement is less familiar now because of worries about metal ions being radiated into the body and provoking damaging responses.
The choice of which kind of hip replacement to utilize will rely on several aspects, including age, bone quality, activity status, and any underlying medical illnesses. The orthopedic surgeon will recommend the best kind of hip replacement for the patient’s particular conditions.
Surgical Approaches for Total Hip Replacement
Any number of approaches can be utilized for the total hip replacement technique. The three considerable standard approaches are:
- Posterior approach: A most standard surgical approach for total hip replacement. A main benefit of this approach is the protection of the hip abductors. Accomplished with a patient lying on their side or side-lying position and a surgical incision assembled along the externals of the hip joint.
- Direct anterior approach: This surgical approach has been rising over the past decade. This process is executed with a patient lying on their back or supine lying position & a surgical incision is gathered getting down the front of the thigh between the tensor fascia lata (TFL) and sartorius on the external ending, and the gluteus medius and rectus femoris on the deep side. There are several conceivable benefits of the direct anterior approach. The two main majors are a low dislocation chance & earlier postoperative recuperation.
- Direct lateral (Hardinge) or anterolateral approach: Usually assumed to be a ratio between the anterior approach and posterior approach. The individual is arranged on their side, and the surgical incision is set straight down the externals of the hip joint. The benefits are the balance of delivering an adaptable incision that can be utilized to habilitate deformities and insert technical implants with more inferior dislocation rates underlying surgery than what is marked with posterior approaches. The disadvantage is superior gluteal nerve dissection may consequence in nerve damage, conducting to postoperative Trendelenburg gait, represented by compensatory activities to address hip abductor weakness.
Additionally
- Robotic Arm Assisted THR: Assists with total hip replacement operation, assisting in the accurate positioning of the implants which is connected with enhanced function and lifespan of the total hip replacement. Can be operated in all recent surgical techniques to the hip (AP, PA, and lateral).
- Minimally intrusive surgery is evolving and favored all around the world, because of the faster healing rates and decreased postoperative pain. Long-period follow-up and comparison analyses are still required in this domain.
Watch this 3-minute. video and comprehend the various approaches to total hip replacement operation and the benefits of each technique.
Preparing for Surgery
- Medical Evaluation: This step is necessary to ensure that you are in good enough health to undergo the surgery and successfully recover from it. In cases where patients have chronic medical conditions like heart disease, it is common for them to be evaluated by a specialist such as a cardiologist before the surgery.
- Tests: Several tests, including blood and urine samples, an electrocardiogram (EKG), and chest X-rays, may be necessary to aid in planning your surgery effectively.
- Preparing the Patient’s Skin: Your skin needs to be free from any infections or irritations before the surgery. If you have any such issues, it is important to inform your orthopedic surgeon, who will provide appropriate treatment to improve your skin condition before the surgery.
- Medications: Inform your orthopedic surgeon about any medications you are currently taking. Based on this information, they or your primary care doctor will advise you on which medications you should discontinue and which ones you can continue taking before the surgery.
- Weight Loss: If you are overweight, your doctor may recommend that you lose some weight before the surgery. This is done to reduce stress on your new hip and potentially decrease the risks associated with the surgery.
- Dental Evaluation: During infections after hip replacement surgery aren’t familiar, there is a chance of infection if bacteria penetrate your bloodstream. Since bacteria can enter the bloodstream while dental techniques, it is advisable to achieve any major dental work, for example, tooth extractions or periodontal therapies, before experiencing hip replacement surgery. Regular teeth cleaning should be delayed for several weeks after the surgery.
- Urinary Evaluation: Individuals with a recent history of urinary infections or frequent urinary issues should undergo a urological evaluation before the surgery.
- Social Planning: Even though you will be capable to walk with the assistance of a cane, crutches, or a walker soon after the surgery, you may need help with tasks like cooking, shopping, bathing, and laundry for some weeks.
If you live alone, a social worker or a discharge planner at the hospital can assist you in making arrangements in advance to have someone support you at home. In some cases, a short stay in an extended care facility during the recovery period after the surgery may also be arranged.
Home Planning:
Making several modifications to your home can greatly enhance its navigability during your recovery from hip replacement surgery. Consider incorporating the following items to facilitate your daily activities:
- Sturdy safety bars or handrails securely fastened in your shower or bathtub
- Reliable handrails installed along all stairways
- A stable chair with a firm seat cushion (allowing your knees to be lower than your hips), a solid backrest, and two armrests to support your early recovery
- A raised toilet seat for added convenience
- A stable shower bench or chair for bathing comfortably
- A long-handled sponge and shower hose to aid in bathing
- Assistive tools such as a dressing stick, a sock aid, and a long-handled shoehorn facilitate putting on and removing shoes and socks without excessive bending of your new hip
- A reacher device that allows you to grab objects without straining your hips
- Firm pillows for your chairs, sofas, and car, promoting a seating position with your knees lower than your hips
- Ensure the removal of all loose carpets and electrical cords from areas where you walk into your home.
Medical management
The success of your surgery will greatly depend on how well you adhere to the instructions provided by your orthopedic surgeon for home care during the initial weeks following the surgery.
Pain Management:
Your doctor may prescribe medications to alleviate pain in the short term after surgery. Pain management drugs, involving opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and local anesthetics. A combination of these medications may be utilized to improve pain relief and minimize the need for opioids.
It’s important to note that while opioids can effectively relieve post-surgical pain, they are classified as narcotics and carry the risk of addiction. It is crucial to use opioids strictly as directed by your doctor and discontinue their usage once your pain begins to improve. If your pain does not show signs of improvement within a few days after surgery, consult your doctor.
Wound Care:
Your wound may be secured with stitches, staples, or an internal suture beneath the skin. The removal of stitches or staples usually takes place approximately two weeks after surgery.
Ensure that the wound remains dry until it has completely sealed and dried. You may continue to cover the wound with bandages to prevent irritation from clothing or support stockings.
Diet:
An upset appetite is expected for some weeks after surgery. A well-balanced diet, potentially supplemented with iron, is crucial for promoting proper tissue healing and restoring muscle strength. Remember to stay adequately hydrated by consuming plenty of fluids.
Activity:
Engaging in exercise is a vital aspect of home care, particularly during the initial weeks after surgery. You should gradually be able to resume most light daily activities within three to six weeks post-surgery. Some discomfort during activities and at night is normal during the recovery period.
Your activity routine should include:
- A gradual walking program, starting within your home and gradually progressing to outdoor walking, to enhance your mobility.
- Resumption of normal household activities like sitting, standing, and climbing stairs.
- Specific exercises aimed at restoring movement and strengthening your hip. While you may be able to perform these exercises independently, you might receive assistance from a physical therapist either at home or in a therapy center during the initial weeks after surgery.
Possible Complications of Surgery
The incidence of complications following hip replacement surgery is generally low. Serious complications, such as joint infection, are observed in less than 2% of patients, while major medical complications like heart attack or stroke occur even less frequently. However, the presence of pre-existing chronic illnesses may slightly elevate the risk of complications. Although rare, these complications, when they do arise, can potentially delay or limit full recovery.
Infection:
Infection can manifest as a superficial wound infection or a deep infection around the prosthetic joint. It may occur shortly after surgery or even years later. Minor wound infections are typically treated with antibiotics, while more severe or deep infections may necessitate additional surgery and removal of the prosthetic joint. It’s important to note that infections originating from any part of the body can spread to the joint replacement.
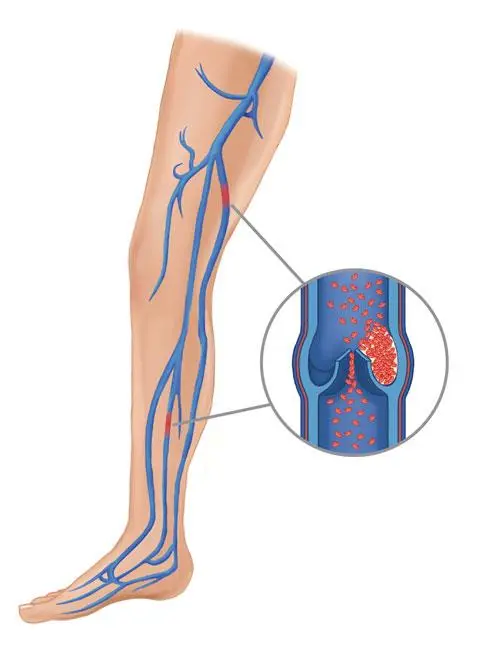
Blood Clots:
The formation of blood clots in the veins of the leg or pelvis is among the most common complications following hip replacement surgery. If these clots dislodge and travel to the lungs, they can become life-threatening. To mitigate the risk, orthopedic surgeons often prescribe preventive measures such as blood-thinning medications, support hoses, inflatable leg coverings, ankle pump exercises, and early mobilization.
Leg-Length Discrepancy:
Occasionally, patients may perceive a difference in leg length after hip replacement surgery, with one leg feeling longer or shorter than the other. Surgeons strive to achieve equal leg lengths, but slight adjustments may be made to enhance hip stability and biomechanics. In some cases, patients may find comfort in using a shoe lift following surgery.
Dislocation:
A dislocation in the hip joint happens when the ball of the hip joint comes out of the socket. The risk of dislocation is highest during the initial months of healing. While dislocation is uncommon, if it does occur, a closed reduction procedure is usually performed to put the ball back into place without requiring further surgery. However, recurrent dislocations may necessitate additional surgical intervention.
Loosening and Implant Wear:
Over time, the hip prosthesis may experience wear or looseness, primarily due to normal daily activities. This can also be influenced by osteolysis, a condition characterized by the thinning of bone tissue. If loosening becomes painful, revision surgery may be required to address the issue.
Other Complications:
In rare cases, nerve and blood vessel injuries, bleeding, fractures, and stiffness can occur following hip replacement surgery. A small percentage of patients may continue to experience pain even after the surgical procedure has been performed.
Avoiding Problems After Total Hip Replacement
Recognizing the Signs of a Blood Clot
It is crucial to carefully follow the instructions provided by your orthopedic surgeon to minimize the risk of developing blood clots during the initial weeks of recovery. You may be advised to continue taking blood-thinning medication as prescribed during your hospital stay. If you experience any of the following warning signs, it is important to notify your doctor immediately:
- Unrelated calf and leg pain not associated with the incision
- Tenderness or redness in the calf
- New or worsening swelling in the thigh, calf, ankle, or foot
Preventing Infection
Infections following hip replacement surgery can often be traced back to bacteria entering the bloodstream during dental procedures, urinary tract infections, or skin infections. Depending on your risk factors, you may need to take antibiotics prior to dental work, including routine cleanings, or before any surgical procedure that may introduce bacteria into the bloodstream. Your orthopedic surgeon will discuss with you whether preventive antibiotics are necessary.
If you notice any of the following signs, inform your doctor immediately, as they may indicate a possible infection at the site of your hip replacement:
- Persistent fever (temperature exceeding 100°F orally)
- Chills
- Increasing redness, tenderness, or swelling at the hip wound site
- Drainage from the hip wound
- Worsening hip pain during both activity and rest
Avoiding Falls
Taking precautions to prevent falls is essential during the initial weeks after surgery to protect your new hip and avoid the need for additional surgery. Staircases can be particularly risky until your hip strength and mobility improve. It is advisable to use assistive devices such as canes, crutches, walkers, or handrails, and to have assistance from someone until your balance, flexibility, and strength improve.
Your orthopedic surgeon and physical therapist will guide you in determining which assistive aids are necessary post-surgery and when they can be safely discontinued.
Other Precautions
To ensure proper recovery and minimize the risk of prosthesis dislocation, you may be instructed to take specific precautions while sitting, bending, or sleeping during the first six weeks after surgery. These precautions will vary depending on the surgical approach used by your surgeon for the hip replacement procedure.
Your surgeon and physical therapist will provide detailed instructions and guidance tailored to your individual needs.
Physiotherapy Management
Discuss Hip precautions before surgery.

- The posterior approach avoids hip flexion beyond 90 degrees, excessive medial rotation, and adduction outside the midline of the body.
- The anterolateral approach avoids hip extension, excessive lateral rotation, and adduction further the midline of the body.
- The anterior approach avoids hip bridging, extension, excessive lateral rotation, and adduction further the midline of the body.
Pre-operative physiotherapy management
One-on-one preoperative physiotherapy session protocol is useful for decreasing the number of postoperative physiotherapy visits and time for readiness to release from physiotherapy. It plays a crucial part in enhancing the preoperative grade of life (individuals can wait many months for surgery and undergo additional degeneration in the health-affiliated quality of life while prolonged waits).
Pre-operative assessment and treatment session
Useful to make a patient-specific treatment plan to follow post-operative, taking examination into consideration eg the patient’s desire to uptake golf.
Benefits: reduced time of visit, reduced nervousness levels, enhanced self-confidence, establish a relationship of faith between the physiotherapist & patient.
A combination of verbal explanations and written pamphlets is the best method for health education. Essential to comprise this into the pre-operative physiotherapy management of patients previous to total hip replacement surgery.
Pre-operative Assessment
- Subjective history
- Range of motion
- Muscle power
- Circulation
- Mobility and function
Pre-operative Treatment
- Education and advice: Patient information pamphlet, Protection, and contraindications, Restoration procedure, Goals & expectations, Functional/ADL modifications, and Security principles.
- Encourage them to stop smoking if applicable
- Discharge planning
- Teach: Bed activities, Sift in and out of bed (within protection)
- Gait re-education with mobility assistive device (crutches vs walkers)
- Stair climbing
Post-operative physiotherapy management
Commencing rehabilitation on the day of surgery has been found to have several benefits, including reduced hospital stay, decreased pain, and improved functionality.
- The primary objective of post-operative rehabilitation is to address the patient’s functional requirements, such as initiating mobilization and enhancing mobility, strength, flexibility, and pain reduction. Initially, assistance may be provided, but the ultimate goal is to maximize the patient’s functional capabilities before discharge.
- Due to the pre-existing condition leading to the surgery, patients may exhibit muscle atrophy and weakness, particularly in the gluteus medius and quadriceps muscles. This loss of strength often results in decreased independence among the elderly.
- While surgery corrects joint issues, the pre-existing muscle weakness persists and necessitates post-operative rehabilitation. Research indicates that hip abductor weakness following surgery is a significant risk factor for joint instability and prosthetic loosening. Regardless, patients can accomplish significant modifications via targeted strength exercise programs obeying total hip replacement. The inclusion of Motor Imagery training as an adjunct therapy has shown positive results, enhancing both specific and general adaptations related to patients’ physical capabilities in conjunction with routine physical therapy.
Currently, there is no universally adopted standard protocol for hip replacement rehabilitation, as certain aspects of the rehabilitation process vary among surgeons. For instance, some enhanced recovery after surgery protocols involves mobilizing patients within the first six hours after surgery, while others may delay mobilization until day 1 or 2 post-surgery. Accelerated rehabilitation programs and early mobilization have demonstrated benefits in terms of boosting patients’ confidence in post-operative mobility and daily activities, as well as facilitating earlier discharge.
Evidence
Physiotherapy plays a crucial role in enhancing strength, and gait speed, and preventing complications like subluxation and thromboembolic disease after total hip replacement. It promotes mobility, provides education on exercises and precautions during hospitalization and post-discharge, and maximizes overall function. An improved function is associated with a higher likelihood of early discharge, leading to reduced overall healthcare costs.
Engaging in bed activities obeying a total hip replacement is necessary as it assists decrease edema, improves cardiac function, and enhances range of motion (ROM) and muscular strength.
Early weight-bearing and physical activity offer benefits for bone tissue quality, prosthesis fixation, and reducing the risk of early loosening. The level of activity should be tailored to each patient, with clinical reasoning guiding any necessary adaptations. It’s important to note that certain specific sports movements may pose a higher risk of injury for inexperienced individuals, and these should be incorporated later in the rehabilitation process under the supervision of a physiotherapist.
In the absence of complications, the following protocol is suggested. However, it is crucial to consider the surgeon’s preferences and any other factors that may impact adherence to the protocol. Adaptations should be made as necessary.
Day 1 Post-Surgery
Education and Advice:
- Providing education on muscle relaxation techniques.
- Reviewing precautions and contraindications, assuming the patient had a pre-operative session with the physiotherapist. Otherwise, comprehensive education will be provided as mentioned in the pre-operative section.
Bed Exercises:
- Performing circulation drills to improve blood flow.
- Engaging in upper limb exercises to stimulate cardiac function.
- Maintaining range of motion in the non-operated leg to ensure controlled mobilization of the operated hip.
- Performing isometric quadriceps exercises (progressing to concentric VMO) and gluteal contractions.
- Assisting with active-assisted (progressing to active) heel slides, and hip abduction/adduction.
- Promoting bed mobilization using unilateral bridging on the unaffected leg.
- Helping the patient in sifting in and out of bed.
- Helping the patient with getting on and off a chair with arm support.
- Assisting the patient in sit-to-stand exercises using a mobility assistive device, preferably a walking frame or rollator, for increased support.
- Re-educating the patient’s gait with the use of a mobility assistive device as tolerated, taking into consideration the weight-bearing status determined by the surgeon.
- Encouraging the patient to sit out in a chair for a maximum of one hour.
- Providing guidance on proper positioning when transferring back to bed.
Day 2 Post-Surgery
- Bed exercises, as previously described, should be progressed by increasing the number of repetitions and reducing the level of assistance provided to the patient.
- Gradually increase the distance mobilized during exercises and/or encourage the patient to rely less on mobility assistive devices.
- If necessary, incorporate balance exercises into the rehabilitation program to improve stability and coordination.
- Include sitting in a chair as part of the rehabilitation process, gradually increasing the duration of time spent sitting.
Day 3 Post-Surgery
- Bed exercises should be continued, progressing the number of repetitions and reducing the level of assistance provided to the patient.
- Gradually increase the distance mobilized during exercises and consider the use of mobility assistive devices as needed.
- Incorporate stair climbing into the rehabilitation program, aiming for at least three flights of stairs or as per the requirements of the patient’s home.
- Continue working on sitting in a chair, gradually increasing the duration of time spent in a seated position.
- Ensure a thorough revision of precautions, contraindications, and functional adaptations to ensure the patient’s safety and progress.
- Prescribe a progressive resistive strengthening home exercise program for a period of six weeks, including exercises such as stationary cycling, while ensuring that the patient adheres to the necessary precautions, especially in the case of posterior approach surgery.
After three days, if the patient meets the discharge criteria, they are typically discharged home. The physiotherapist and nurse provide assistance in transferring the patient to the car while maintaining hip precautions. It is important to note that the majority of patients may lack certain abilities or skills during the early stages of recovery.
Discharge Home Criteria:
- Achieving independent ambulation with the assistance of an appropriate mobility device.
- Attaining the ability to perform transfers independently, without requiring assistance.
- Developing independence in activities of daily living (ADLs), such as grooming, dressing, and bathing, without relying on external help.
- Practicing stair climbing with supervision to ensure safety and proper technique.
- Arranging suitable home assistance, whether it be from a spouse, family members, or visiting nurses, to provide additional support during the recovery period.
Home Planning
To enhance home navigation during the recovery period, several modifications can be implemented. The following items are beneficial for daily activities:
- Properly installed safety bars or handrails in the shower or bath area.
- Sturdy handrails along all stairways.
- A steady chair specially developed for earlier healing, provided with a firm seat pillow that permits the knees to stay lower than the hips. Additionally, the chair should have a strong backrest and two armrests.
- A raised toilet seat facilitates easier and safer use of the toilet.
- A stable shower bench or chair for comfortable bathing.
- Useful tools such as a long-handled sponge and shower hose to assist with bathing.
- Helpful aids like a dressing stick, sock aid, and long-handled shoehorn to aid in dressing and footwear.
- A reacher tool that enables the user to grasp objects without excessive bending of the hips.
- Firm pillows for chairs, sofas, and cars, provide proper support and allow individuals to maintain a position where their knees are lower than their hips.
- Ensuring the removal of all loose carpets and electrical cords from the areas where individuals walk within the home to prevent tripping hazards.
Watch a 7-minute video that demonstrates post-operative exercises after a total hip replacement surgery for 1 to 4 weeks.
6 Weeks Post Surgery
- Patients are normally followed up by an orthopedic surgeon
- The orthopedic surgeon decides if the patient is allowed the following activities such as:
- Full range of motion at the hip
- Full weight bearing without mobility assistive device
- Driving
After 6 Weeks
- Gain of initial ROM, stabilization, and proprioception
- Endurance
- Flexibility
- Balance
- Speed, precision, neurological coordination
- Functional exercises
Return to sport
Low-impact exercises are preferred
- Golf: handicap shows minimal change after THA, handicap shows an increase after TKA.
- High-effect activities raise correction rates in patients less than 55 years aged.
Outcome Measures
- Harris Hip Score
- Oxford Hip Score (OHS)
- 6-Minute Walking Test
- Timed Get Up & Go Test
- SF-36
- Fear Avoidance Belief Score
- Hip Disability & Osteoarthritis Outcome Score (HOOS)
- International Hip Outcome Tool
- Ibadan Knee/Hip Osteoarthritis Outcome Measure
Team Work
Total hip arthroplasty (THA) stands as one of the most dependable, consistent, effective, and economically viable procedures in the field of orthopedics. Its successful execution necessitates seamless coordination among different healthcare providers, including nurses, physical therapists, advanced practitioners, medical physicians, and orthopedic surgeons.
Collaboration among clinicians, such as the surgeon, nurse practitioner, and physician assistant, is vital in offering comprehensive education to patients and their families regarding the procedure, anticipated concerns, and postoperative care instructions. This interdisciplinary approach ensures that patients receive thorough guidance and support throughout their treatment journey.
FAQ
Is hip replacement surgery for you?
The judgment to have a hip replacement operation should be a suitable one produced by a person, his relative, his primary care physician, & orthopedic surgeon. The procedure of completing this conclusion generally starts with a referral by your physician to an orthopedic surgeon for an initial estimate.
When THR is recommended?
There are several causes why a doctor may instruct hip replacement surgery. Individuals who aid from hip replacement surgery frequently have:
Hip distress that restricts day-to-day actions, like walking/bending.
The hip ache persists during resting either day or night.
Immobility in the hip restricts the capability to move or raise the leg.
Impaired pain relief from anti-inflammatory drugs, physiotherapy, and walking aids.
Who are the candidates for THR?
There are no definite age/weight limitations for total hip replacements (THR).
Suggestions for operation are established on the pain and disability of persons, not age. Most individuals who experience total hip replacement are 50 to 80 years old, but orthopedic surgeons estimate patients separately. Total hip replacements have been executed successfully for all generations, from the youthful teenager with adolescent arthritis to the geriatric patient with degenerative arthritis.
How much is the recovery time for a total hip replacement?
On moderate, hip replacement healing can take about 2-4 weeks, but everyone’s recovery is different. It relies on some aspects, involving how engaged a person was before their surgery, their age, diet, preexisting illnesses, and other health and lifestyle elements.
Which hip replacement is best?
The most acceptable hip replacement procedure out there is via the anterior approach. The anterior purpose is from the front of the hip. Most of the country typically goes from the posterior approach. The posterior approach works but the risk of post-operative dislocations are more elevated than the anterior approach.
Can a person live a normal life after hip replacement?
Around three months after the hip replacement (THR) operation most things will return to normal and the ache diminish for most individuals. Individuals must examine for signs and symptoms of complications and continue being careful about how they drive their hips. After 6 to 12 months, the healing is believed done.



8 Comments