Anterior Interosseous Nerve Syndrome
What is an Anterior Interosseous Nerve Syndrome?
Anterior interosseous nerve syndrome (AINS), also known as Kiloh-Nevin syndrome, is a rare neurological condition that affects the function of the anterior interosseous nerve (AIN). The AIN is a branch of the median nerve, which originates from the brachial plexus in the neck and supplies the muscles in the forearm.
AINS typically occurs as a result of compression or entrapment of the AIN along its course. The exact cause of compression can vary, but it is often due to traumatic injury, repetitive overuse, or anatomical anomalies. Some common causes include forearm fractures, muscle hypertrophy, and certain activities or occupations that involve repetitive wrist or forearm motions.
Anterior interosseous nerve syndrome is an alone palsy of these three muscles. It displays mainly as pain in the forearm attended repeatedly by a usual weakness of the index finger and thumb pincer motion. Many cases of anterior interosseous nerve syndrome will explore secondary to a few diseases like temporal neuritis, therefore nerve compression and trauma were the well-known causes as satisfactory. Different reasons should be presented as the causes of the disease.
Related Anatomy
To understand anterior interosseous nerve syndrome (AINS), it is helpful to have knowledge of the related anatomy. Here are some key anatomical structures involved:
- Brachial Plexus: It is a network of nerves that arises from the spinal cord in the neck. It gives rise to various nerves that innervate the upper extremity, including the median nerve.
- Median Nerve: The median nerve is a major nerve in the upper limb that originates from the brachial plexus. It runs down the arm, passes through the cubital fossa (elbow region), and enters the forearm. It provides motor and sensory innervation to several muscles and areas of the hand.
- Anterior Interosseous Nerve (AIN): The AIN is a branch of the median nerve that arises in the forearm, typically around the level of the elbow. It travels between the flexor digitorum superficialis and flexor digitorum profundus muscles and gives off branches to innervate specific muscles.
- Flexor Pollicis Longus: The flexor pollicis longus is a muscle located in the forearm. It originates from the radius bone and attaches to the thumb. It works as a flexing of the thumb.
- Flexor Digitorum Profundus: The flexor digitorum profundus is a muscle in the forearm that lies deep to the superficialis. It originates from the ulna bone and attaches to the distal phalanges of the index, middle, ring, and little fingers. It is responsible for flexing the distal interphalangeal joints of these fingers.
- Pronator Quadratus: The pronator quadratus is a square-shaped muscle in the forearm that runs from the distal portion of the ulna to the distal portion of the radius. It acts as a pronator, helping to rotate the forearm and hand medially.
These structures, particularly the anterior interosseous nerve and the muscles it innervates, play a crucial role in forearm and hand movements. Compression or entrapment of the AIN can lead to the development of anterior interosseous nerve syndrome and subsequent weakness or paralysis of the affected muscles.
Symptoms and Signs for the Anterior Interosseous Nerve Syndrome
Patients might feel badly localized, temporary pain in the wrist, where the sensory branch of the anterior interosseous nerve will generalize in the brain. The pain is sometimes directed into the cubital fossa and elbow pain has been noted as being a prior complaint.
Clinical signs of the anterior interosseous nerve syndrome
In a solid lesion of the anterior interosseous nerve, there would be just minor fatigue of the long flexor muscle of the thumb which includes the following muscles( Flexor pollicis longus), the deep flexor muscles of the index fingers and middle fingers (Flexor digitorum profundus one and two, and the pronator quadratus muscle).
later if the anterior interosseous nerve will no cutaneous roots to the skin, there should be no sensory deficiency present but there is a large sensory root to the proximal carpal bones, and temporary wrist pain might be experienced.
Causes of the Anterior interosseous nerve Syndrome
Injuries of the forearm with compression of the nerve from swelling are the most familiar cause: examples contain repeatedly related to hemorrhage into the deep musculature; dislocation of the elbow.
Direct trauma from a sharp injury such as a stab wound will be a probable cause of the anterior interosseous nerve syndrome.
Fibrous bands or Arcuate ligament might interrupt the median nerve as well as the anterior interosseous nerve, in which a patient must feel hand numbness as well as wrist pain. Very similar syndromes should be caused by more adjacent lesions
Anterior interosseous nerve trap or compression injury stays a challenging clinical diagnosis due to it being especially a motor nerve problem, and the anterior nerve interosseous syndrome is repeatedly misunderstood between the index finger and thumb tendon injury.
causes should be classified as either voluntary or traumatic.
the traumatic causes begin with forearm fractures such as supracondylar fractures, puncturing injuries
- cast fixation
- venipuncture: blood taken from a vein
- a complication of open reduction and internal fixation of fractures, etc.
- the most common voluntary causative factors should involve brachial plexus neuritis, compartment syndrome, and compression neuropathy.
The most common site of anterior interosseous nerve entrapment or compression is the tendinous boundary of the deep head of the pronator teres muscle. Other possible areas of the anterior interosseous nerve contain
- The proximal edge of the flexor digitorum superficialis arch ,the flexor digitorum superficialis arcade
- Gantzer’s muscle which involves the accessory head of the flexor policies longus muscle
- the flexor digitorum superficialis or flexor digitorum profundes accessory muscles
- Arterial thrombosis of the radial or ulnar artery has been involved
- Lacertus fibrous
Anterior interosseous nerve syndrome must be clinically distinguished from stenosing tenosynovitis or pathologies restricted to local pathology impacting the flexor tendons alone flexor tendon adhesion formation or partial versus complete flexor tendon rupture. The anterior interosseous nerve is actually typically squeezed by the fibrous bands that constantly initiate from the deep head of the brachialis fascia and the pronator teres, and this pressure should begin to raise with minor deviations.
Pathophysiology of the Anterior Interosseous Nerve Syndrome
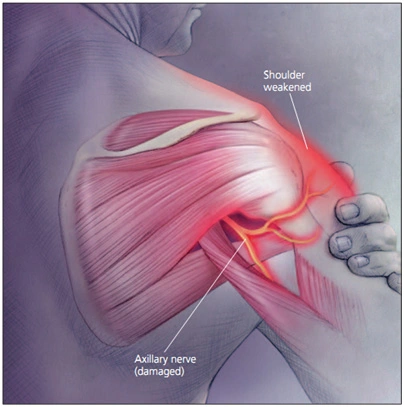
The exact pathophysiology should happen secondary to primary interruption, direct trauma, or in more fuzzy or incomplete clinical presentations, the condition displays following vial neuritis. In the latter, clinicians should have an elevated diagnostic doubt in patients presenting with motor loss following previous symptoms containing intense shoulder pain or recent viral illness/exposure
Diagnosis:
Diagnosis of AINS involves a thorough clinical examination, which may include assessing muscle strength, evaluating for any sensory changes, and performing specific tests to isolate the affected muscles. Electromyography (EMG) and nerve conduction studies may also be used to confirm the diagnosis and determine the extent of nerve damage.
Physical examination
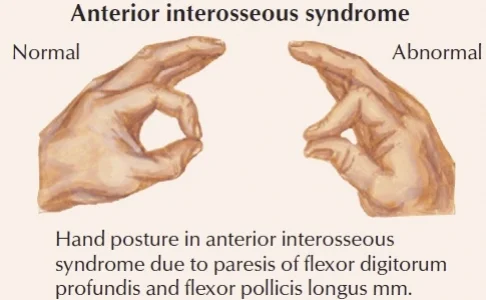
True anterior interosseous membrane syndrome presentation will present with motor deficits only. No sensory changes should be initiated. Most people feel weakly regional pain in the forearm side and cubital fossa. This pain is normally the first complaint of the people. There are no sensations present of numbness, tingling, or sensory deficiency. The patient’s chief complains of having difficulty fetching the distal phalanx of the thumb and index finger together.
On a physical examination, the pinch grip test would turn in to positive; rather than forming the OK test sign, in the pinch grip the patient would grab the sheet in the middle of the index finger and an extended thumb. The patient might also complain of having difficulty beginning to make a fist or the incapability to button their shirts. The sensation should be limited during the examination
Evaluation of the anterior interosseous nerve syndrome
Electrodiagnostic studies should instrumental for anterior interosseous nerve syndrome of random etiology. Sensory nerve conduction of the median nerve must be quite normal as there should be no sensory supply to the anterior interosseous nerve. Electromyography should also show findings in the flexor pollicus longus muscle, the radial part of the flexor digitorum profundus muscle, and the pronator quadratus. These diagnostic methods should be beneficial in differentiating neurologic amyotrophy from compression neuropathy. Magnetic resonance imaging is also helpful in the assessment of anterior interosseous nerve syndrome patients.
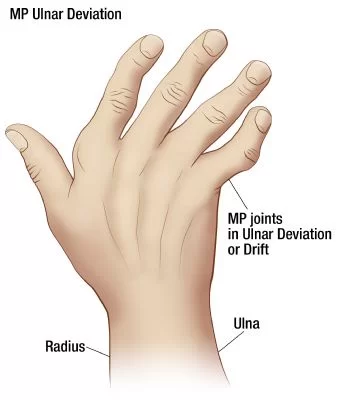
Sign of Benediction: When the therapist instructs the patient to make a fist, the patient would not be capable to flex the second and third fingers which indicate the hand of benediction. benediction is different from the Ulnar claw hand.
anterior interosseous nerve syndrome should be diagnosed by the Martin-Gruber anastomosis, which is present in up to twenty-five percent of people positive in these cases, the anterior interosseous nerve provides roots to the ulnar nerve, creating atypical motor supply patterns of the forearm and hand and thus canceling the specific clinical symptoms
Ericson’s Test
Ericson’s Test is a clinical strategy for estimating the power of the flexor digitorum profundus muscle and flexor policies longus muscles in anterior interosseous nerve syndrome, and other proximal entrapments of the median nerve.
In difference to the “OK sign,” Ericson’s test separates the action of the flexor digitorum profundus and flexor policies longus while destroying the donation of the tenodesis effect and further transformations that patients might utilize, normally unconsciously, to increase distal pincer strength. incapable to prevent compensatory wrist tendonitis should hide an underlying proximal median nerve weakness in a patient who should otherwise be forming a normal OK sign.
While facing the patient in what corresponds to an arm wrestling view, with elbows produced firmly on a level surface and preserved connecting the thorax, the examiner utilizes one hand to resist the patient’s wrist in a neutral position, surrounding which the patient twists his/her fingers. On the other hand, the examiner then tries to grab the peel’s backside tips of each particular finger against patient resistance. It is essential that movement of the upper extremity is limited to the distal interphalangeal joint, and that the metacarpophalangeal joint and proximal interphalangeal joints should be in full flexion and wrist neutral position or little flexed. If the distal finger flexors of the index and thumb should fatigue, the patient must be incapable of doing index phalanx and thumb motion, and Ericson’s test will be estimated positively for proximal median nerve weakness.
Ericson’s test is continually positive for front side median nerve weakness which anterior interosseous nerve syndrome must explore but as a one sub-category type in fact in the context of normal diagnosing, EMG, and nerve conduction studies, which underlines the clinical nature of the diagnosis. dependence on electrical diagnostic workup unfairly bans patients who would otherwise benefit from surgical decompression
- few signs which should indicate the anterior interosseous nerve syndrome
- OK/Kiloh-Nevin sign: incapable to execute
- Pinch paper in the middle of the thumb and index finger, then, resist the removal of paper: Incapable to executing OR
- Might balance by extending the interphalangeal joint of the thumb and distal interphalangeal joint of the index finger key pinch trick.
- Cutaneous sensory testing Normal
- Muscle stretch reflex Normal
- Tinel’s test Negative
- Phalen’s Maneuver Negative
Differential diagnosis of the anterior interosseous nerve syndrome
it consists of a non-compressive neuropathy like brachial neuritis, which might simulate anterior interosseous nerve neuropathy. Flexor policies longus tendon rupture must also be probable among patients who have rheumatoid arthritis. To exclude the differential diagnosis, the wrist must be flexed passively by the therapist and extended to ensure that the individual will have an entire tenodesis influence Rheumatoid disease and gouty arthritis might be predisposing factors in anterior interosseous nerve syndrome.
Anterior interosseous nerve compression injury stays a competitive clinical diagnosis. It is hard because it is priorly a motor nerve and the syndrome should be repeatedly mistaken for a ligamentous finger injury. Differential diagnosis involves stenosing tenosynovitis, and flexor tendon adherence can cause very similar syndromes for the anterior interosseous nerve.
Treatment for Anterior Interosseous Nerve Syndrome
Treatment for AINS typically involves conservative measures, including activity modification, rest, and avoiding repetitive movements that exacerbate symptoms. Physical therapy and occupational therapy may be beneficial to improve muscle strength and function. In some cases, surgical intervention may be necessary if conservative treatments are ineffective or if there is evidence of severe nerve compression.
Nonoperative modalities
The widespread agreement for handling anterior interosseous nerve syndrome contains a period of rest, observation, and splinting of the elbow around ninety degrees of flexion or taking the position which should be most comfortable for the patient. The majority of patients would experience improvement between six to twelve weeks of activity modification.
Other modalities to regard contain nonsteroidal anti-inflammatory drugs and physical therapy modalities involving pain modalities and massage techniques if accepted
Surgical decompression
Surgical therapy consists of the investigation for neurolysis, and decompression behind several months of failed nonoperative modalities. The literature conveys seventy-five percent or greater positive effects following surgery, with more elevated rates noted in patients with an identifiable, clear space-occupying mass.
Unless a precise cause is determined, surgical intervention should normally be suggested just in preferred cases, and the choice will be concerned following at least three months of failed conservative treatment.
During median nerve surgical decompression, careful dissection should be essential to confirm the precise locations of compression. It is essential in the identification and discharge of compressing boundaries or fibrous bands.
Physiotherapy Treatment for the Anterior Interosseous Nerve Syndrome
Based on the reason for anterior interosseous nerve syndrome, the physiotherapy regime varies. In spontaneous anterior interosseous nerve syndrome, physiotherapy intervention recreates a crucial role as the real cause of palsy should be unknown. Since it is motor neuropathy, the goals of physiotherapy intervention should:
- to maintain muscle integrity.
- to decrease the over-sensitivity of the nerve.
- to prevent contractures.
- to accelerate the strength of particular muscles.
So to attain those goals the next intervention must be provided but it should be unforced and a follow-up assessment every month is a must.
- Nerve mobilization exercises of the upper extremity.
- Stretching exercise of the forearm
- therapeutic modalities like electrical stimulation, Transcutaneous Electrical Stimulation, or Neuromuscular Electrical Stimulation
- Soft tissue mobilization of forearm musculature.
- Strengthening exercises of hand and wrist.
Nerve mobilization exercises of the upper extremity
Median Nerve Glide
To glide the median nerve, a central nerve in the upper extremity:
- Stand up straight.
- Put the arm by the side with the palm facing upward.
- Gradually flex the wrist downward, stretching the front of the wrist and palm.
- Then, bend the head far from the outstretched arm. Be sure to preserve good posture and alignment of the shoulders as the person bend the wrist and neck.
- Hold the position for 2 seconds, then come back to the starting position with the wrist and head normal position.
- Repeat 10 to 15 times.
Ulnar Nerve Glide
To glide the ulnar nerve, a central nerve in the arm:
- Stand with the arm stretched out to the side, palm facing the floor.
- Gradually bend the elbow and wrist upward so that the palm of the hand moves towards the side of the face. the person should feel a mild jerk in the wrist, pinky, or elbow.
- Hold the position for 2 seconds, and then gradually release the position.
- Repeat 10 to 15 times.
Radial Nerve Glide
To glide the radial nerve, a primary nerve in the upper extremity:
- Stand with the arm downward at the person’s side close to the hip, palm facing backward.
- Flex the wrist and then gradually drag the shoulder backside into extension.
- While maintaining this position, bend the neck away from the person’s arm.
- Maintain the position for 2 seconds, and then gradually release.
- Repeat 10 to 15 times.
Stretching exercise of the forearm
the muscles are divided into an anterior compartment (flexors) and a posterior compartment (extensors), with the flexors bearing roughly twice the bulk and strength rather than the extensors.
Anterior (Flexors) Compartment
- Superficial (first) Layer contains of Pronator Teres,palmaris longus,flexor carpi ulnaris,
- The intermediate (second) Layer contains flexor digitorum superficialis,
- The deep (third) Layer contains flexor digitorum profundus, flexor policies longus, pronator quadratus
Posterior (Extensors) Compartment
superficial layer
- extensor carpi radialis longus
- extensor carpi radialis brevis
- extensor carpi ulnaris
- brachioradialis
- anconeus
intermediate layers
- extensor digitorum
- extensor digitiminimi
deep layer
- abductor policis longus
- extensor policis longus
- extensor policis brevis
- extensor indicis
- supinator
Benefits Of Forearm Stretches
Stretching assists preserve the flexibility of the flexors and extensors which should be significant in stopping overuse injuries such as tenosynovitis and tendinitis.
Extensor Stretch

- Lift one arm outside with the elbow straight.
- Use the other hand to grab the arm at the side of the thumb and bend the wrist downward.
- Hold the stretch for 20-30 seconds.
another method

- Put the arms at chest height with the elbows bent and the back of the hands together.
- With the back of individual hands touching each other, extend the wrists till a mild stretch should be felt on top of the forearm and wrists.
- Preserve the stretch for 20-30 seconds.
flexor stretch
- Hold the palm of one hand with the other hand, while maintaining the elbow straight on the affected arm.
- Drag the hand backward slightly to feel a stretch in the forearm.
- Hold the stretch for 20-30 seconds.
another method

- Put the fingers and palms of the hands together.
- Lower the hands and extend the elbows separated as far as the person can while maintaining the palms together until the person feels a stretch.
- Preserve the stretch for 20-30 seconds.
- Relax the hands.
- When executed stretching perfectly, the stretching exercise generates the wrists to turn backside until the person feels a stretch across the palms, wrists, and internal forearms.
Pronator Stretch

- Bend one elbow next to the body and position the other hand on the back of the hand.
- With help from the other hand, rotate the forearm to obtain the palm of the hand facing the ceiling until the person feels a stretch in the forearm.
- maintain the pronator stretching for 20-30 seconds.
- Maintain the position and relax.
Supinator Stretch

- Bend one elbow and position it next to the body.
- Maintain the palm facing downward on the stretched arm.
- Position the other hand beyond the wrist.
- Rotate the wrist slightly to turn the wrists upwards until the person feels a stretch in the forearm.
- Hold the supinator stretch for 20-30 seconds.
- Maintain the position and relax. and then repeat.
Soft tissue mobilization of the forearm musculature
Purposes of Soft Tissue Mobilization:
- Break down or diminish adhesions
- Enhance range of motion
- Extend muscles and tendons
- Lower swelling and edema
- Lowering pain
- Reform functionality
Sustained force: give thrust directly on the restricted tissue and holding
Unlocking circle: give thrust on the restricted tissue in rotating clockwise and counterclockwise rotating motions
Direct oscillations: gradually forcing on the restricted tissue
Perpendicular mobilization: forcing on the myofascial tissue at right angles
Parallel mobilization: thrusting along the stitching of muscles
Perpendicular pluck: gradually forcing along the muscle border, followed by rubber on top of the muscle
Deep Friction massage: forcing across the grain of the muscles, tendons, and ligaments
Being capable to execute soft tissue mobilization approaches demands a considerable portion of exercise in human anatomy and physiology and understanding how using the tissues will affect physical function. Physical therapists specialize in the evaluation, assessment, and treatment of motion function disorders. Soft tissue manipulation is just one of the treatment options to help patients complete their functional goals.
physical exercise and modalities like cryo massage, neural mobilization, transcutaneous electrical nerve stimulation, and the strain-counter strain approach four times a week for two weeks in a patient who had anterior interosseous nerve syndrome because of an active stimulus point in the center of the anterior forearm. strain-counter strain is elaborate as an indirect myofascial approach that is explored to treat bodily dysfunctions of the neuro-musculoskeletal system. After the myofascial intervention, the patient has revealed an improved pinch grip strength of eight pounds, an inactive trigger point verified via palpation, and improved handwriting.
Prognosis
The prognosis is generally good, and most cases don’t need surgical treatment. If conservative treatment fails further three months, surgery might be suggested in select cases.
It is very essential to utilize result instruments to see the prediction and also to define the goal of the patient following anterior interosseous nerve syndrome. There are various results in managing hand dexterity and even a simple manual muscle test should be utilized as an outcome measure.
Enhancing Healthcare Team Outcomes
Even though anterior interosseous nerve syndrome is very rare, the clinical fear concern appears in the presence of the radial flexor digitorum profundus and weak flexor pollicis longus muscles. The utilization of electrodiagnostic studies, associated with MRI and balance assists in the diagnosis of the anterior interosseous syndrome and helps to determine the possible etiology.
Anterior interosseous nerve syndrome’s optimal treatment should not be verified. It is suggested that surgical interventions be proposed only to those patients who should not reveal any clinical improvement during the first few months or to those with confirmed cases of compression neuropathy. Careful dissection should be required during median nerve surgical decompression to select sites of compression. It is crucial in the identification and clearance of any further compressing boundaries or fibrous bands.
An interprofessional method of treatment is excellent. This system contains primary care providers who face the disease first and electrophysiologists who handle the nerve and muscle studies. It also contains orthopedic surgeons who obey the course of treatment, pharmacists who provide the medication required, and physical therapists who conduct the rehabilitation. Other healthcare team personnel like the nursing staff should also help in the conformed care of the patient. These teams would obtain result in the best outcomes.
If you suspect you may have anterior interosseous nerve syndrome or are experiencing symptoms similar to those described, it is important to consult with a healthcare professional for a proper evaluation and diagnosis. They will be able to provide you with appropriate guidance and develop a suitable treatment plan based on your specific situation.
FAQs
Where does the anterior interosseous nerve get compressed?
The most common site of anterior interosseous nerve syndrome entrapment/compression is the tendinous boundary of the deep head of the pronator teres muscle. Other potential sites involve: The proximal boundary of the flexor digitorum superficialis arch (the FDS arcade), Gantzer’s muscle accessory head of the FPL muscle
What is the special test that is utilized to ensure an anterior interosseous nerve syndrome?
Ericson’s Test is a clinical trick for assessing the strength of the flexor digitorum profundas and flexor policies longus muscles in anterior interosseous nerve syndrome, and other proximal entrapments of the median nerve.
How is anterior interosseous nerve syndrome treated?
The general concurrence for handling anterior interosseous nerve syndrome includes a period of rest, observation, and splinting of the elbow near 90 degrees of flexion or the position of most comfort for the patient. The majority of patients will experience progress between six and twelve weeks of activity modification.
How much glide is executed for evaluation for anterior interosseous nerve syndrome?
radial, median, and ulnar glide executed for evaluation for anterior interosseous nerve syndrome
which medicine is used for anterior interosseous nerve syndrome?
a nonsteroidal anti-inflammatory drug commonly used to relieve pain for a temporary base



3 Comments