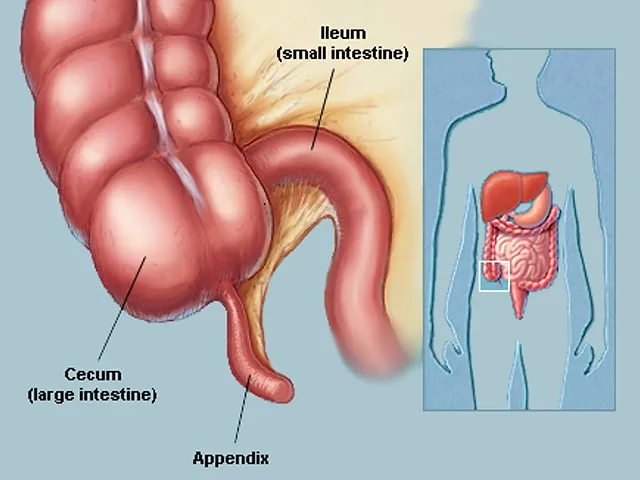
Appendicitis
An inflamed appendix is known as appendicitis. It may result in acute (sudden, severe) lower abdominal pain. Your appendix is a tiny, finger-sized tubular pouch that extends from the lower right end of your big intestine. Your large intestine can become blocked or infected by poop (feces), which can result in inflammation in your appendix. Your appendix swells due to inflammation, and as it swells, it has the potential to explode.
A medical emergency is a ruptured appendix. It disperses microorganisms throughout your abdominal cavity from your bowels. The spread of this infection (peritonitis) into your bloodstream can then result in potentially fatal consequences (sepsis). The conventional course of treatment for appendicitis is appendectomy because of this risk. You won’t miss having an appendix because it is not a necessary organ.
What is Appendicitis?
Appendix inflammation is referred to as appendicitis. The colon is located on the lower right side of the belly, commonly known as the abdomen, and the appendix is a finger-shaped pouch that protrudes from it.
Lower right belly pain is a symptom of appendicitis. However, for the majority of patients, the pain starts near the belly button and subsequently spreads. Appendicitis pain often intensifies and finally becomes severe as the inflammation worsens.
Although anyone can have appendicitis, people between the ages of 10 and 30 are the most likely to do so. Appendix removal surgery and antibiotics are typically used to treat appendicitis.
Appendix ectomy surgery must nearly always be performed as soon as is practical because it is a medical emergency. Thankfully, you can survive without it.
When your appendix becomes inflamed, usually as a result of a blockage, it can get infected and cause appendicitis. It may manifest as cramping or excruciating abdominal discomfort. Your appendix may rupture if appendicitis is not treated.
Appendicitis is the most common condition in the US that results in stomach pain and requires surgery. It affects up to 9% of Americans at some point in their lives.
A little pouch connected to the intestine, the appendix. It’s located in your lower right abdomen. Your appendix can develop bacteria if it is obstructed. Pus and oedema may grow as a result, putting pressure on your abdomen that hurts. Appendicitis can potentially stop blood flow.
Bacteria can enter your abdominal cavity if your appendix bursts, which can be dangerous and occasionally fatal.
Causes of Appendicitis
Infection or obstruction in the appendix are two potential causes of appendicitis. Although the precise aetiology of this is unknown, it is believed to be brought on by food or feces (poo) being lodged in the appendix. As a result, the appendix becomes obstructed, then swollen, inflamed, and finally infected.
Appendicitis is most likely caused by an obstruction in the lining of the appendix. An infection may result from this obstruction. The appendix subsequently becomes inflamed, bloated, and pus-filled as a result of the bacteria’s rapid growth. The appendix may rupture if immediate treatment is not received.
Appendicitis’ precise cause is frequently unknown. It is to specialists when a section of the appendix becomes occluded or clogged.
There are many reasons why your appendix could get obstructed, including:
- Intestinal worms, swollen lymphoid follicles, and an accumulation of tough stool
- Tumors from traumatic injury
- Numerous medical problems can cause abdominal pain. For information on more possible causes of pain in your lower right abdomen.
Anyone can get appendicitis. However, some people are more susceptible to this illness than others.
Why does appendicitis occur?
Your appendix is prone to clogging and infection due to its size and position. Numerous bacteria live in your large intestine; if too many of them wind up in your appendix, they overgrow and result in an infection. Sometimes an infection precedes appendicitis, and other times the disease develops afterwards. Your appendix’s swelling might narrow or seal the entrance, trapping additional bacteria inside.
The following are typical reasons for obstruction, inflammation, oedema, and infection in your appendix:
- Appendix stones are hardened stools: Fecaliths, appendicoliths, or appendix stones are hard, calcified faecal deposits that can become lodged in the opening of your appendix. In addition to carrying bacteria, they can trap bacteria that were previously present in your appendix.
- Hyperplasia of the lymph nodes: By creating and releasing white blood cells into your tissues, the lymphatic system, a component of your immune system, aids in the battle against infections. Even if the initial infection was elsewhere in your body, this can cause the lymphoid tissue in your appendix to expand. Your appendix’s enlarged tissue may restrict it and cause an infection there.
- Colitis: Your appendix may become inflamed if you have an infection or inflammatory bowel disease. It’s possible for the infection to spread or for the inflammation to irritate it.
In addition, the following things could prevent your appendix from opening:
- Cystic fibrosis
- Parasites
- Tumours.
Acute appendicitis appears to be brought on by a major obstruction of the appendix. When this obstruction happens, the appendix swells and fills with mucus. The appendix’s lumen and walls are under greater pressure as a result of this ongoing mucus generation. The small veins get occluded and thrombosed as a result of the increased pressure, and the lymphatic flow becomes stagnant. Rarely does spontaneous recovery take place at this point. The appendix becomes ischemic and finally necrotic as the blood artery obstruction worsens. Pus occurs inside and around the appendix (suppuration) as germs start to escape through the decaying walls. The end result is appendiceal rupture, or a “burst appendix,” which causes peritonitis and, in rare instances, sepsis and death. These incidents are to blame for the gradually worsening stomach pain and other often-present symptoms.
Bezoars, foreign things, trauma, lymphadenitis, and, most frequently, appendicoliths or fecaliths, which are calcified faecal deposits, are among the causes. Obstructing fecaliths are more common in industrialized countries than in poor countries, which has drawn attention to their prevalence in appendicitis patients. Additionally, severe appendicitis is frequently accompanied by an appendiceal fecalith. People with acute appendicitis have fewer bowel movements per week in comparison to healthy controls, which may be due to faecal stasis and arrest.
It was believed that a right-sided faecal retention reservoir in the colon and a protracted transit time were responsible for the development of a fecalith in the appendix. An extended transit time wasn’t noticed in further trials, though. In groups where appendicitis itself was uncommon or non-existent, such as certain African communities, diverticular disease and adenomatous polyps were historically unknown, and colon cancer was extremely uncommon. Studies have linked growing rates of appendicitis and the other colonic disorders described above in these populations to a shift to a Western diet reduced in fibre.
Additionally, it has been demonstrated that cancer of the colon and rectum often precedes acute appendicitis. Studies show that a low-fibre diet contributes to the pathophysiology of appendicitis. The right-sided fecal reservoir’s prevalence plus the fact that dietary fiber speeds up transit time explains this low intake of dietary fiber.
Risk Factors:
Appendicitis risk factors include:
- Age: Although it can happen at any age, appendicitis most frequently affects adolescents and people in their 20s.
- Sex: Appendicitis is more likely to affect men than women.
- Family background: Appendicitis runs in families, therefore those with a history are more vulnerable to getting it.
Symptoms of Appendicitis
What early indications of appendicitis are there?
Abdominal discomfort typically starts in the center of your abdomen, close to your belly button. For several hours, it could hover or come and go. Later, as the pain worsens, nausea and vomiting start to appear. After a few hours, the nausea goes away and the discomfort moves to the lower right area of your abdomen, where your appendix is located. The discomfort intensifies and concentrates more.
You can experience mild stomach discomfort in the early stages of appendicitis, which gradually spreads to your lower right abdominal quadrant. This pain is persistent:
- Starts out quickly
- It worsens when you cough or move
- It is terrible and distinct from previous abdominal pain you have had, and it wakes you up from sleep. It gets worse after a few hours.
These are some other signs of appendicitis:
- Reduced appetite
- Indigestion
- Nausea
- Vomiting
- Stomach bloating
- A minor fever
Less frequently, you encounter gastrointestinal issues like:
- Diarrhea
- Constipation
- The need to go for bowel movements
- Inability to exhale
What other signs and symptoms might there be of appendicitis?
In some people, further symptoms could appear. These may consist of:
- Fever: An average of 40% of people get a fever. This indicates that your immune system is ramping up. It might also indicate a rise in inflammation or the spread of an illness.
- Malaise: Perhaps all you notice is that you feel generally ill. You can feel tired or unmotivated and want to stay in bed, just as when you’re sick.
- Bloated belly: Your stomach could feel bloated or appear enlarged. This is typically an indication of old age and can mean your appendix has burst.
- Urine symptoms: You might experience more frequent or urgent urges to urinate. This may occur if appendicitis aggravates bladder-related nerves.
- Intestinal paralysis: Your bowels may momentarily stop moving if your body diverts blood flow from them to your appendix. Constipation can cause some people to feel as though they are unable to pass gas. You may feel as though having a bowel movement will make your symptoms go away.
- Diarrhea. Some people may have more frequent bowel movements and hyperactive bowels. This could be a result of your appendix’s inflammation irritating the end of your colon next to it.
Depending on the patient’s age and the location of the appendix, the pain’s location may change. Due to the pregnancy’s elevated appendix, pain may appear to originate in the upper abdomen.
Unfortunately, only around 50% of those who have appendicitis present with the traditional set of symptoms. Children, older adults, and pregnant women may less frequently exhibit the usual symptoms.
Diagnosis:
Your symptoms and medical background will be discussed with you if your doctor thinks you may have appendicitis. They will then do a physical examination to look for any edema or rigidity in the lower right portion of your abdomen as well as any soreness. There is also a chance of using a digital rectal exam.
Your doctor may prescribe one or more tests to look for symptoms of appendicitis or rule out other possible explanations of your symptoms, depending on the findings of your physical examination.
Particularly in young children, appendicitis can be challenging to diagnose. Even in adults, it can be challenging to distinguish between appendicitis and other abdominal conditions. To determine the most likely diagnosis, your doctor may track the course of your ailment over time.
Your doctor may occasionally use tests including an ultrasound, a CT scan, and blood work to diagnose appendicitis. In some circumstances, even if they are unsure whether the appendix is inflamed, your doctor may recommend an operation to inspect it.
Appendicitis cannot be diagnosed with a single test. Your doctor may make the diagnosis of appendicitis if no other reasons for your symptoms can be found.
Blood test
Your doctor could request a full blood count (CBC) in order to look for indicators of illness. They will take a sample of your blood and send it to a lab for analysis in order to perform this test.
A bacterial infection frequently occurs in conjunction with appendicitis. Similar symptoms to appendicitis can also be caused by infections in the urinary tract or other abdominal organs.
In order to rule out other causes of abdominal inflammation, such as an autoimmune disorder or another chronic ailment, your doctor may also request a C-reactive protein test.
Urine test:
Your doctor may do a urinalysis to rule out kidney stones or an infection of the urinary tract as probable causes of your symptoms. Testing of urine is another term for it.
Test for pregnancy
Appendicitis and ectopic pregnancy can be confused. Instead of the uterus, it occurs when a fertilized egg implants itself in a fallopian tube. There may be a medical emergency as a result of this.
A pregnancy test could be done if your doctor thinks you might have an ectopic pregnancy. They will take a sample of your blood or urine to do the test. The site of the implanted fertilized egg may also be identified via transvaginal ultrasonography.
Examining the pelvis
If you were born a girl, your symptoms could be caused by ovarian cysts, pelvic inflammatory disease, or another condition affecting your reproductive system.
A pelvic exam may be performed by your doctor to examine your reproductive system.
During this examination, they will visually inspect your cervix, vulva, and vagina.
They will also examine your uterus and ovaries in person. They could collect a tissue sample for examination.
Abdominal imaging examinations
Your doctor could advise an abdominal scan to check for appendix inflammation. This can help in the search for symptoms of an abscess, inflammation, or other appendix problems.
It can also assist medical professionals in determining further probable reasons of your symptoms, such as:
- Abdominal infection
- Inflammatory bowel disease
- Fecal impaction
One or more imaging tests from the list below may be prescribed by your doctor:
- abdominal sonography
- stomach X-ray
- abdomen-contrast MRI
- abdomen-focused MRI
- abdominal sonography
In some circumstances, you might have to refrain from eating for a while prior to your test. Your doctor can provide you with information on how to prepare for it.
Chest imaging tests
Additionally, symptoms of appendicitis can also be caused by pneumonia in the lower right lobe of your lungs.
Your doctor will probably request a chest X-ray if they suspect you have pneumonia. To get precise photos of your lungs, they could also need an ultrasound or a CT scan.
A CT scan produces more accurate images of your organs than an ultrasound. However, because a CT scan exposes the patient to radiation, it is typically only advised as a last resort following an ultrasound and an MRI.
A developing fetus may be harmed by CT scans. In the event that you are of childbearing age, your doctor will initially suggest a pregnancy test.
Complications:
If you experience constipation and suspect you may have appendicitis, avoid using laxatives or an enema. These operations have the risk of rupturing your appendix.
Because appendicitis can swiftly result in extremely significant consequences, medical professionals treat it as an emergency. Although it’s not usually the case, complications can develop in phases. Stages of complications include:
- Necrosis and ischemia: Your appendix becomes severely swollen, cutting off the blood supply (ischemia), which worsens the inflammation and eventually starts the tissue’s decomposition (necrosis).
- Gangrene/perforation: The onset of necrosis might cause the infection to spread. When your appendix ruptures or tears (perforation), it may spread swiftly or slowly depending on whether you have internal gangrene.
- Abscess/phlegm: The infection may initially only affect your appendix. Your appendix may develop a pus-filled abscess on the outside. The appendix can also form a phlegmon, which is a mass that surrounds it. Although they can rupture, these tumours confine the infection.
- Peritonettitis and infection dissemination: Infection can spread to other organs and even your bloodstream (septicemia) when it enters your peritoneal cavity (peritonitis). The potentially lethal conditions of sepsis and septic shock can result from an infection in your bloodstream.
Treatment of Appendicitis
Since appendicitis is treated in the emergency room, it is seen as an emergency. Surgery and medicine are both part of the usual course of treatment, though occasionally medication alone may be sufficient.
Medical treatment:
Antibiotics are almost universally required for appendicitis. Appendicitis frequently results in an infection, even if you don’t already have one. Antibiotics are also a common preoperative preventative measure.
Your doctor may decide to wait and see whether your condition gets better on its own if you have an extremely early and mild case of appendicitis. If you have risk factors that make surgery less safe for you, you may prefer this technique. However, doctors don’t usually advise it because appendicitis can recur if your appendix isn’t removed.
For pain relief, you might also require medication. This can be administered by IV. If you’re undergoing surgery, general anesthesia will be administered so that you won’t be awake or cognizant during the process.
Surgical treatment:
Surgery to remove the appendix is typically part of the therapy for appendicitis. You might be given antibiotics before surgery to treat an infection.
Having the appendix surgically removed
Appendix removal surgery is known as an appendectomy. An abdominal incision between two and four inches long can be used to perform an appendectomy as open surgery. It is known as a laparotomy. The procedure can also be achieved through a few tiny abdominal incisions. This type of surgery is referred to as laparoscopic. The surgeon inserts specialized instruments and a camera into your abdomen to remove your appendix during a laparoscopic appendectomy.
Laparoscopic surgery generally allows for a quicker recovery with less pain and scarring. It might be better for fat people and older adults.
Laparoscopic surgery is not appropriate for everyone, though. If your appendix has ruptured and the infection has moved outside of the appendix, or if you have an abscess, you might require an open appendectomy. Your surgeon can thoroughly clean the abdominal cavity during an open appendectomy.
After your appendectomy, plan to stay in the hospital for 1 to 2 days.
Removing an infection prior to appendix surgery
The abscess may be drained if your appendix bursts and an abscess develops around it. A catheter is inserted into the abscess via your skin to drain it. Once the infection has been under control for a few weeks, an appendectomy can be done.
Antibiotics may be taken alone if your appendicitis is not severe and does not require surgery. The likelihood of appendicitis returning is increased if the appendix is not removed.
Outlook:
The outlook is favorable with early detection and treatment. The majority of people fully and swiftly recover. Your recovery could take longer if you have complex appendicitis. If the infection has moved outside of your appendix, you may require additional treatments. 40% of cases of appendicitis that are treated alone with antibiotics recur. Untreated appendicitis has a mortality rate of more than 50%.
Your prognosis and length of recovery from appendicitis will depend on a number of variables, including:
- Your general health,
- Whether you experience complications after surgery or appendicitis,
- The particular treatments you receive
If your appendix is removed via laparoscopic surgery, you might be able to leave the hospital that day or the following morning.
If you undergo open surgery, you’ll probably require additional recovery time in the hospital. Compared to laparoscopic surgery, open surgery is more intrusive and often requires more aftercare.
Before you leave the hospital, your healthcare professional might instruct you on how to care for the regions where you had incisions. They could suggest using painkillers or antibiotics to help with your recovery.
They can also suggest that you alter your diet, stay away from physically demanding activities, or change other aspects of your normal routine while you recover.
You might need a few weeks to fully recover from your appendicitis and surgery. If problems occur, your healing process can take longer.
FAQs
What are the first signs of appendicitis?
An abdominal soreness that may come and go is the typical initial sign of appendicitis. Your lower right side, where the appendix is typically located, starts to experience discomfort within a few hours, and it quickly worsens and becomes constant. Walking, coughing, or applying pressure to this area may exacerbate the pain.
How do issues with the appendix begin?
Appendicitis is most likely caused by an obstruction in the lining of the appendix. An infection may result from this obstruction. The appendix subsequently becomes inflamed, bloated, and pus-filled as a result of the bacteria’s rapid growth. The appendix may rupture if immediate treatment is not received.
How does the pain in your appendix feel?
A sudden, severe pain that begins on the right side of your lower abdomen is the telltale sign of appendicitis. Additionally, it could begin close to your belly button and progress lower to your right. When you cough, sneeze, or move, the discomfort may at first feel like a cramp and may get worse.
What are the five phases of appendicitis?
The different stages of appendicitis are early, suppurative, gangrenous, perforated, phlegmonous, spontaneously resolving, recurrent, and chronic.
What are the four symptoms and indicators of appendicitis?
If you experience any of the following appendicitis signs or symptoms, get medical help right away:
You are experiencing a lower right quadrant abdominal ache.
The ache in my abdomen is growing worse.
stomach ache along with nausea and/or fever.
Sensitivity to touch and soreness in the abdomen.



One Comment