Laminectomy
What is a Laminectomy?
Pressure on the spinal cord and nerve roots can bring pain and numbness or tingling in the arms and legs. In the lower reverse (lumbar region) pressure on the nerve roots can lead to affection walking and problems with bowel and bladder function. Laminectomy might be an option to help relieve pain.
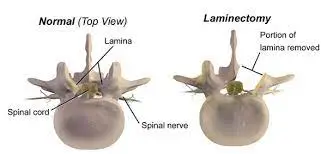
The lamina( described as “ bony bends ”) are bone pieces that stick out from the reverse of the spine. Their removal during surgical operation relieves pressure on nerve roots or the spinal cord, which can result in improvements in function and quality of life.
One of the most frequent treatments to widen the spinal canal is laminectomy. This is done in cases when the spinal canal has narrowed due to diverse disorders such as degenerative stenosis, fracture, primary and secondary spinal tumors, abscesses, and scarring. A successful clinical recovery and the avoidance of failed back surgery syndrome require the release of the central canal, the side recesses, and the neural foramina. The interprofessional units are pushed into service as this activity explains the laminectomy form in order to evaluate and enhance care for patients who have undergone this posterior spinal decompression operation.
It’s one of the most common spinal surgeries among cohorts further than 65 years of age. The classical laminectomy has a central, facet joint-sparing laminectomy. The spinous process and the lamella are removed limited indirectly to the medium part of hand joints. There was no benefit in conserving the midline structures. The central canal, the side recesses, and the neural foramina need to be decompressed for good clinical recovery and prevention of failed back surgery syndrome.
Currently, there are several ways to accomplish posterior spinal relaxation, similar to open or minimally invasive laminectomy, hemilaminectomy, laminotomies, and laminoplasty. decompression techniques are categorized as circular& direct; circular relaxation takes place without dural sac visualization. Instead, direct procedures involve those techniques of visualization of the dural sac during the surgery, the same as laminectomy.
One of the most frequent methods used by a spinal surgeon is either a laminectomy alone or one combined with a fusion.
Laminectomy is surgery that makes space by removing bone spurs & tissues associated with arthritis of the spine. It generally involves removing a small piece of the left part(lamella) of the small bones of the spine( vertebrae). Laminectomy expands the spinal canal to relieve pressure on the nerves or spinal cord. Laminectomy is frequently done as part of decompression surgery.
The pressure is most commonly generated by bony overgrowths within the spinal canal, which can occur in populations who have arthritis in their backbones. These overgrowths are occasionally called bone spurs. They are a side effect of growing for some people. Bone spurs can also be inherited.
This surgery is generally utilized only when other conservative treatment plans like physical remedies, drugs, or injections have been ineffective to relieve symptoms. This surgery might also be suggested if symptoms are more severe or getting much worsen.
What is the anatomy of the Spine?
Exact information on the posterior vertebral curvature and spine anatomy is imperative to understanding the principles of laminectomy.
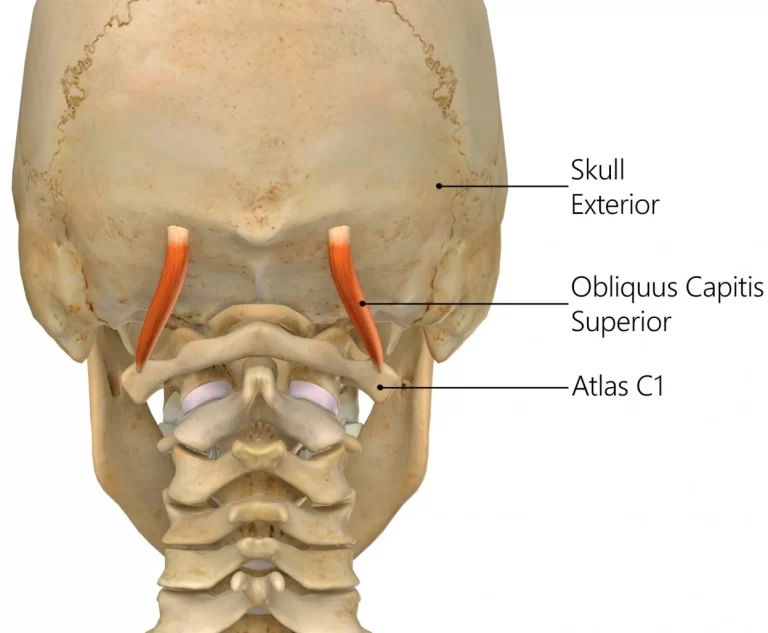
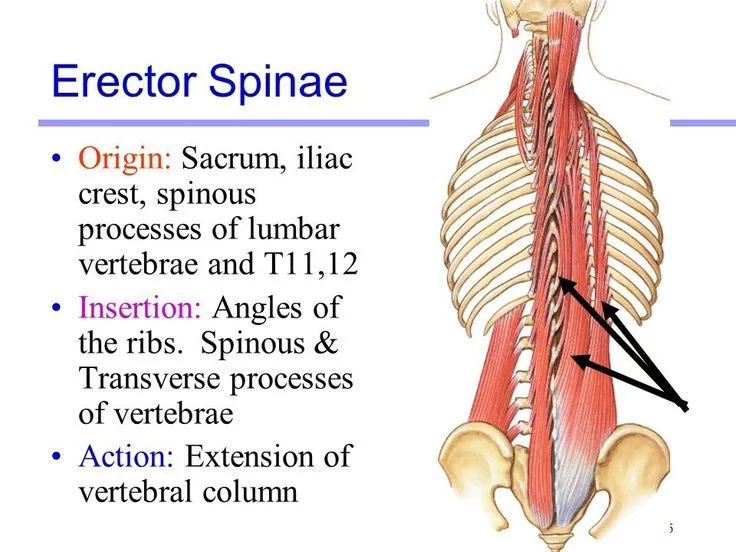
The laminae belong to the posterior vertebral curvature, extended medially from the base of the spinous process to the junction between the superior and inferior facet joints, performing as a stabilization structure of the spine in alliance with the facet joint and also as a spinal cord and nerve root defensive layer. The laminae’s usual anatomy contains a superior & inferior border, an anterior exterior in contact with the medullary canal, & a posterior exterior that serves as erector spinae muscles attachment. The shape and consistency of the laminae vary according to the anatomical area. Laminar height tends to drop from C2 to C4 and then elevates towards a peak at T8. From T9 to L4 tends to drop in height & elevate in length having at L5 the smallest lumbar height; on the other hand, from cervical to lumbar, the laminae range decreases progressively over to the narrowest at the T4 level in the thoracic area and also increases steadily to reach the widest at L5 level.
Regarding consistency, it increases from the cervical to the lumbar regions.
A better understanding of the spine anatomy in different spinal regions might enhance surgery success and avoid induced complications similar to nerve root or spinal cord injury.
Why Is a Laminectomy Performed?
The main suggestion for laminectomy is the presence of spinal canal stenosis. According to Wiltse, spinal stenosis can also be categorized into central stenosis, side recess, foraminal and extraforaminal stenosis. Also, Lee et al. categorized the lateral region into three zones of nerve root contraction entrance zone( side recess), medial zone( foraminal region), and exit zone( extraforaminal region) in order to clarify anatomy and surgical plan. Laminectomy is especially useful for the treatment of central and side recess stenosis.
Spinal stenosis may be caused by
- the recoil of the discs of the spine and swelling of the bones
- and ligaments, which both do with growing
- arthritis of the spine, which is more common in aged grown-ups
- a congenital disfigurement, or disfigurement present at birth, similar to abnormal growth of the spine
- Paget’s complaint about the bones is a
- condition in which bones grow inaccurately
- achondroplasia, which is a type of dwarfism
- a tumor in the spine
- a traumatic injury
- a Disc prolapse or slipped disc
Central stenosis is the most ordinary, and the main symptom is neurogenic claudication, which includes pain, tingling, or cramping sensation in the lower extremity. On the other hand, side recess, foraminal, and extraforaminal stenosis may induce radiculopathy, cases with central stenosis may witness further symptoms in standing position and during walking, and pain is usually relieved by forward leaning or in a sitting position. In cases of central stenosis, straight leg raising, and femoral nerve stretching test are generally normal.
When symptoms derived from stenosis don’t respond to conservative treatment, surgical management similar to decompression with or without fusion is generally an account.
Fusion methods are needed when stenosis is associated with spinal instability, degenerative or isthmic spondylolisthesis, kyphosis, or scoliosis, as laminectomy alone may increase the threat of spinal instability in these conditions. still, in cases of low-grade degenerative spondylolisthesis, the research exhibits variable results regarding the threat of instability after laminectomy alone; some studies support fusion in cases of degenerative spondylolisthesis. On the other hand, Wang et al., in a recent meta-analysis, found no increased threat of instability after laminectomy, especially in cases without predominant symptoms of mechanical back pain and after minimally invasive procedures.
Other important suggestions for laminectomy are primary or secondary tumors, infection( peridural abscesses), trauma( fractures that compromise the spinal canal), and stenosis associated with disfigurement.
The radiological armamentarium needed in the workup includes:
- CT criteria for central stenosis include anteroposterior girth(< 10 mm) and cross-sectional area(< 70 mm2) of the spinal canal.
- MRI – Gold standard imaging modality
- Dynamic flexion/ extension films to figure out instability & spondylolisthesis
- EMG- for distinguishing distal neuropathies
- PlanX-ray- hip and knee- confounding osteoarthritis
Indications for laminectomy include:
Central or side canal stenosis refractory to 12 weeks of the drug, physical remedy, and injections
Presence of uncontrollable pain or progressive neurological deficits
Presentation with cauda equina syndrome
still, surgery may be a choice, If medical treatments no longer work. Some medical management for pain might include:
- Changes in activity
- Medicines, similar to muscle relaxants, anti-inflammatory drugs, and pain relievers
- Spinal injections
- Physical rehabilitation, physical remedy, or both
- Occupational remedy
- Weight loss( if fat)
- Smoking cutoff
- Assistive devices, similar to mechanical back supports
Laminectomy is generally done for back or neck pain given after medical treatment. Or it is done when the pain is accompanied by symptoms of nerve damage, similar to numbness or weakness in the arms or legs.
Risk factors
The risks of spine surgery include:
- damage to a spinal nerve
- unsuccessful treatment, which can lead to pain that persists following surgery
- a return of back pain, particularly later spinal fusion
- an infection in the surgical place or vertebral bones
- Bowel or bladder problems (incontinence).
- Risks linked to the usage of general anesthesia
- a cerebrospinal fluid leak because of a tear of the dura mater, the membrane that presents around the spinal cord
The general risks of surgery include:
- a blood clot in the legs, which can cause a pulmonary embolism
- breathing difficulties
- an infection
- blood loss
- a heart attack
- a stroke
- a reaction to the medication
What are the Contraindications of a Laminectomy?
- Spondylolisthesis
- Scoliosis and
- Lateral listhesis
- Poor surgical candidates include:
Patients with multiple medical comorbidities are also not good candidates for surgery
Patients with depression-compromised walking and concurrent scoliosis
How to prepare the patient for the Surgery?
- The healthcare provider will explain the surgery to the patient and offer you the chance to ask any doubts that you might have about the process.
- You’ll be asked to sign an allowance form that gives your authorization to do the surgery. Read the form precisely and ask questions if a thing isn’t clear.
- In addition to a complete health history, your healthcare provider may do a physical test to make sure that you’re in good health before experiencing the procedure. You may have blood tests or other individual tests.
- Inform a healthcare provider if the patient is sensitive to or is allergic to any kind of drugs, latex, tape, & anesthesia drugs(original and general).
- Tell a healthcare provider about all prescribed and over-the-counter drugs and herbal supplements that you’re taking.
- Tell a healthcare provider if you have a history of bleeding diseases or if you’re taking any blood-thinning (anticoagulant)drugs, aspirin, or other drugs that influence blood clotting. You may be told to stop these drugs before the procedure.
- still, tell your healthcare provider, If you’re pregnant or suppose you could be.
- Follow any directions you’re presented for not eating or drinking before the surgery.
- You may get an opiate before the surgery to help you relax.
- You can meet a physical therapist before your surgery to talk about rehabilitation.
- Certain activities may be limited after your surgery. Arrange for someone to assist you for many days with the home activities and driving.
- Grounded on your health condition, your healthcare provider may have other instructions for you.
What happens during a laminectomy?
Equipment:
Standard radiolucent table with spinal frames and lathers pads
C- arm to localize position and minimize skin size gash
Laminectomy instrument set( bone cutting rongeurs, high- speed purr, Kerrison rongeurs, forceps, ball tip, angled spatula spreader, bayonet- shaped curettes, concave probes, tubular retractors, and dilators for MIS approaches)
Personnel:
One or two spinal surgeons, a registered OT nurse manpower, and anesthesiologists
Neuromonitoring is generally a recommendation in cervical or dorsal laminectomies and lumbar cases when there’s an accelerated threat of nerve injury
Preparation:
This surgery is done with the patient in the prone position on a support frame with leather pads for nipples & ASIS( anterior superior iliac crest spine), leaving the abdomen free, avoiding abdominal pressure decreases epidural venous pressure and, thus, surgical spot bleeding. The surgery generally takes around two hours but can take longer if it’s part of a more complex procedure or if numerous situations need to be addressed.
Arms are deposited at 90 degrees of abduction and flexion to avert axillary nerve injury.
Technique:
Laminectomy can be done through both a traditional open approach or with a minimally invasive technique.
The traditional open approach requires a posterior midline incision( 3 to 4 cm in length for a single position) and subperiosteal analysis along spinous processes to detach and retract paraspinal muscles from the spinous processes medially to the side laminar border avoiding damage to the hand joint. Spinous processes may be resected along with rearward lamellae to expose ligamentum flavum with bone slice rongeur or a purr, resection of ligamentum flavum is possible with Woodson elevator and spatula, and medium facetectomies can be performed to relax the side recess. The foraminal region can is accessible with Kerrison rongeurs. Use of a ball tip or angled inquiry help to assess foraminal size. Great care is necessary to avoid damage to the pars interarticularis and further than 50 of the hand joint to drop the threat of insecurity. The decompression approach is generally complete upon evidence of the dural sac, exiting, & descending nerve roots.
Minimally Invasive Surgical approaches contain laminectomy & microendoscopic laminectomy with tubular retractors. Contemporary literature supports these approaches performing in better preservation of posterior musculature, dropped intraoperative bleeding, & postoperative pain.
Indeed though MIS approaches may have some early resultant advantages over open procedures, the profitable value and cost-effectiveness of MIS bear further examination.
A recent methodical review compared conventional laminectomy with three different ways that avoid removing the spinous process( unilateral laminotomy, bilateral laminotomy, and resolve spinous process laminotomy). A depreciate postoperative back pain for bilateral laminotomy & split spinous laminotomy was set up; still, there were no noticeable clinically significant differences. Further, there was no disfiguration in terms of medical center length of stay, operative time, & complications of these methods compared to conventional laminectomy.
The salient surgical way in classical decompressive laminectomy can be epitomized as follows:
- Prone positioning
- The tummy should be made free of any overdue pressure
- Anatomical localization backed with fluoroscopy
- Superficial tissue and muscle anatomizing to reach the spinous process
- In some laminectomy procedures, subperiosteal lamella dissection does not extend past the tip of the transverse process or beyond the axis of facet joints.
- Spinous process disposal via large rongeur or Horsley bone blade
- disposal of the lamella via Leksell rongeur starting from theinter-laminar space
- disposal of thickened ligament flavum via Kerrison rongeur
- A high-speed drill to thin the lamella followed by its disposal via Kerrison can also be accepted
- Undercutting of medium facet and decompression of separate foramina
- Layered wound close after icing hemostasis and placement of a drain
What happens after a Laminectomy?
In the hospital:
After the surgery, a patient will be taken to the recovery room for observation. Once your blood pressure, palpitation, & breathing are stable and you’re alert, you’ll be taken to the hospital room. Laminectomy generally requires that you stay in the clinic for one or further days.
You’ll most likely begin getting out of bed and walking on the evening of your surgery. The pain will be controlled with drugs so that the patient can take part in the exercise. The patient might be given an exercise plan to follow both in the hospital & after discharge at home.
At home:
Once you’re at home, it’s important to keep the surgical incision region clean and dry. the healthcare provider will address you with specific bathing instructions. The surgical staples or stitches are taken off during a follow-up office visit.
Take a pain reliever for soreness as suggested by the healthcare provider. Aspirin or certain other pain remedies may increase the chance of bleeding. Be sure to take only recommended drugs. the healthcare provider might recommend a physical remedy after a laminectomy to enhance your strength and resilience.
While you’re getting back, you should…
- avoid aggressive exertion and heavy lifting
- be careful when climbing stairs
- gradually increase your conditioning, similar to walking
- schedule and go to all follow-up appointments
- While showering, you shouldn’t scrub over the incision point. Don’t apply any creams or creams near the incision. Avoid bathtubs, hot barrels, and swimming pools until your doctor says else. These can each increase your threat of infection.
Your doctor will give you specific instructions on how to take care of your abrasion.
Ask the healthcare provider about any of the following happens:
- Fever
- reddishness, swelling, bleeding, or other drainages from the incision point
- Increased pain around the incision point
- draining, heat, or reddishness at the incision point
- tenderness or swelling in the legs
- difficulty breathing
- chest pain
- Numbness in your legs, back, or buttocks
- Difficulty in urinating or loss of control of a bladder or bowel
Do not drive until you were told by the healthcare provider. Do not bend over to pick up objects or arch your back. The healthcare provider might tell you to limit other activities.
The healthcare provider might give you other instructions after the procedure, depending on your individual situation.
Depending on the measure of lifting, walking, and sitting your job involves, you may be suitable to return to work within a countable week. still, your recovery time will be longer, If you also have a spinal fusion.
What are the complications of a Laminectomy?
Instability: Damage to the pars interarticularis is a threat. Damage to more than half of facets on bilateral or whole facets on one side intraoperatively command fusion surgery. Since L1- 3 has a narrow surgical corridor for decompression, preservation of pars is of ultimate significance at these degrees.
Bony Re-growth
Kyphosis: because of disturbance of posterior tension banding function of posterior Osseo- ligamentous complex.
Spinal epidural hematoma: most threat at the L2/ 3 situation.
Dural tear: The prevalence is 3.1 to 13 and8.1 to17.4 for primary and modification surgery, independently. It increases the threat of surgical location infections, postoperative deficits, and distraction. The area is the lower surgical zone near the nerve root, followed by the dorsal sac. former surgery and elderly age began to be threat variables. The dural closure approach doesn’t impact modification surgery rates or complications. Primary repair followed by bed rest is supported. minimum access surgeries have minimum dead space, reducing the threat of pseudo meningocele and CSF fistula.
Mortality: prevalence of 0.5 to 2.3 %
What is the result of a Laminectomy?
Most patients report notable improvement in their symptoms after laminectomy, particularly relief in pain that radiates to the leg or arm. But this benefit might lessen over time with some forms of arthritis. Laminectomy is less likely to better pain in the back itself.
In most known conditions of lumbar & thoracic laminectomies, patients tend to recover slowly, with recurring pain or spinal stenosis persisting for up to 18 months following the procedure. In the opinion of a World Health Organization census (WHO) in 2001, most patients who went through a lumbar laminectomy surgery recovered in daily activities within one year of their operation.
Back surgery can decrease pressure on the spine, but it is not an aid-all for spinal stenosis. There might be considerable pain immediately after the surgery, and pain might persist on a longer-term basis. For some patients, recovery can take weeks or months and might need long-term occupational and physical therapy. Surgery does not stop the degenerative process & features may reappear within several years.
Patients who also have a spinal fusion are more likely to have spinal complications in the future.
What is the physiotherapy treatment of a Laminectomy?
Pre-Operative Exercises of a Laminectomy
Instruction in bed mobility, transfers, and body mechanics instruction with ADLs
Instruction in beginning home exercise program
- Ankle pumps
- Gluteal sets
- Quadriceps sets
- Hamstring sets
- Heel slides
- Long and short curvature LE extension
- Transverse Abdominis isometric contractions
- Breathing relaxation exercises
target on regional muscle systems longus colli before primary carriers similar to SCM, & PCM. Original muscles are shorter in length and near to the axis or rotation while the global muscles have no direct attachment to the spine.
Avoid preloading the spine with overhead arm movements too beforehand in recovery. The no pain no gain theorem generally doesn’t apply to the spine
Focus on low-burden-high repetitions to enhance endurance rather than high-burden low repetition for strength.
Focus on pain relief with a Neck Disability Index of 50, with scores of 3050 concentrating on diminishing pain, muscle reeducation, gradational strengthening, and flexibility and enriching cardiovascular endurance, with scores lower than 30 concentrating on work simulation and progressive strengthening.
Post-Operative Cervical laminectomy
Phase I- Immediate post Surgical Phase of 06 weeks
- avert excessive starting movement or stress on tissues.
- Diaphragmatic breathing
- Relaxation exercises
- Upper extremity extension isometric exercises
- Multilevel fusions have hard collars for 6 weeks; one-level fusions wear a collar as required for a week or two
Phase II- 6- 9 weeks and 2- 3 times per week
- Grade- 1 or grade- 2 joint mobilizations for pain modulation
- Cervical Range of motion exercises.
- Cervical Isometric exercises.
- Cervical flexibility exercises Decrease stress on the cervical spine and make it simple to maintain a neutral spine. ( upper trapezius, levator scapula, pectoralis major and minor, etc)
- Start Scapular movement re-education including shoulder shrugs, shoulder rolls, scapular retraction, or depression exercises
- Upper thoracic exercises upper thoracic extension, cat & camel exercises, upper thoracic rotation, arm locks, etc.
- Neuromuscular re-education with pressure biofeedback of regional muscle.
- confined( to 5 lbs) arm exercises. Progress to outflow after 6 weeks
- Cervical isometric
- Modalities for symptom modulation if demanded
Phase- III 9- 12 weeks and 2- 3 times per week
- Posture emphasis with exercises, posture training
- Work/ activity-specific training
- Soft tissue mobilization to diminish guarding
- common mobilizations on determined joints (around fusion) to elevate contribution to the overall movement. defend fusion.
- Neural mobilizations (nerve glides). Don’t reproduce symptoms.
- Upper limb strengthening exercises (Rhythmic stabilization of upper extremity, free weight shoulder strengthening)
- Scapular stabilization & strengthening exercises (shoulder shrugs rolls, incline push-ups, chest presses, seated rows, pull-downs)
- Spinal stabilization exercises lumbar and cervical
- Continue Upper thoracic mobilization exercises
- Advanced balance training exercises.
- Progress with ADL and exertion simulation with the replenishment of longus colli neutral spine.
- Cardiovascular training, treadmill, stationary bike
Post-Operative lumbar laminectomy
Phase I-( 0 to 2 Weeks) Protective Phase
- Avoid bending and twisting, lifting, pushing, and pulling 5kgs or further for two weeks.
- Limit sitting, including the auto, to go no further than 30 minutes at a time( standing/ walk breaks).
- No extension range of movement or rotation exercises for eight weeks
- Educate regarding posture and body mechanics
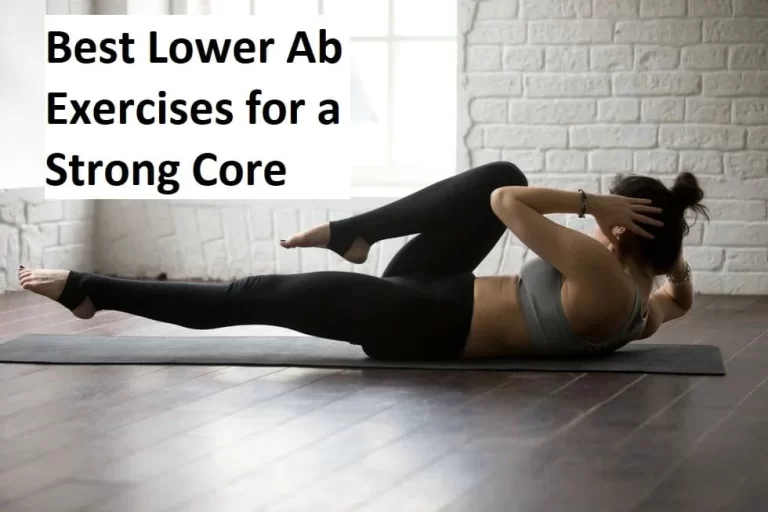
- Light Stretching of Hip flexors, quadriceps, hamstrings, calf, Gluteal, multifidus, & transverse abdominals (without pelvic tilt) bracing isometrics
- Walk for 10 mins twice daily
Phase II-( 2 to 6 Weeks) earliest Strengthening Phase
- Frequency- One to two times a week, for four or further weeks
- Lifting Restrictions commence at 5kgs
- Keep the spine in a neutral position with a focus on proper neuromuscular control
- Walking Progression At least 30 minutes or further Stationary Bike Recumbent Can start at two weeks
- Transverse Abdominis & Multifidus Progression (maintain neutral spine)- beginning with isometrics & advancing to SLR, marches, superman, etc.
- Continue with actual Gluteal Activation Exercises eg, Hip extensions in the prone position, bridging, gluteus isometrics, side lying clams, side lying, 90/90 leg raises, side lying abduction, quadruped hip extension & bird dog
- Upper Extremity & Lower Extremity Strength Training- Step ups, wall squats, leg presses, squats, etc. Balance exercise (with Transverse Abdominals bracing) tandem, single leg stance, foam, etc. Upper extremity mild resistive exercises (machines, theraband, free weights)
Continue stretching exercises
Phase III-( 6 to 8 Weeks) Progression to Advanced Strengthening
- Stabilization exercises & advanced core strengthening exercises in Progression with weight bearing, balance, Swiss Ball, Reformer, etc.
- Progress to multi-planar exercises with upper extremity & lower extremity
- Progress upper extremity & lower extremity strengthening
- Begin running, agility, and plyometrics for return to sport after 8 to 12 weeks( if symptoms stable and unobstructed)
- Lumbar Spine more than 8 weeks to enhance lumbar extension range of movement, but avoid end-range movement Eg. prone lying, prone on elbows, press-ups, & standing extensions (if no peripheralization)
FAQ (frequently asked questions)
Is laminectomy major surgery?
During a laminectomy, a spine surgeon mostly removes all of the laminae. This is considered major surgery & typically is not performed unless more conservative treatment approaches have failed. Laminectomy might be done on the cervical, lumbar, sacral, or thoracic spine.
How long is the recovery for a laminectomy?
In general, here’s what we can expect: After a minor (decompressive) laminectomy, patients are usually able to return to light activity (desk work & light housekeeping) within a few days to a few weeks. If they also had spinal fusion with laminectomy, their recovery time will likely be longer from two to four months.
What are the rules after a laminectomy?
Patients need to avoid twisting & bending. they also need to avoid lifting, pushing, or pulling objects greater than 5 lbs. Lifting & activity restrictions will be gradually eliminated as the healing process takes place. Remember to keep the spine in a neutral position & maintain good posture throughout the day.
Is leg weakness normal after a laminectomy?
Some patients who have had lumbar decompression surgery will develop new numbness or weakness in one or both legs as an outcome of the operation. Paralysis is not common, but serious, complication that can occur as a result of lumbar decompression surgery.
Can laminectomy cause nerve damage?
One kind of post-laminectomy pain is neuropathic pain, which is caused initially by primary injury to the nervous system. In patients with post-laminectomy syndrome, the original spinal disorder that caused the nerve injury before surgery might cause neuropathic pain to return.
Can a laminectomy fail?
In some patients, even after performing a laminectomy, patients experience pain because the spinal column itself is narrowed in a condition called spinal stenosis. Sometimes, there might be a small particle of the disc still remaining following the laminectomy which can irritate the spinal cord causing pain.


One Comment