Arthritis-dermatitis syndrome
What is Arthritis-dermatitis syndrome?
Arthritis-dermatitis syndrome is a form of Disseminated gonococcal infection (DGI) that usually include three types of manifestations such as dermatitis, tenosynovitis, and polyarthralgia. It is also seen with other symptoms such as fever, chills, and body restlessness.
Arthritis-dermatitis syndrome Infectious condition An arthropathy caused by N gonorrhea, represented by tenosynovitis with skin rash and fever, frequently with a positive blood culture; the arthralgia of gonococcal infection is most frequently an asymmetric polyarthralgia;1/4 of Patients have just a monoarthralgia; asymmetric joint involvement often affects the knee joint, elbow joint, wrist joint, metacarpophalangeal, and ankle joints.
Epidemiology
- Half of the twenty million new sexually transmitted infections (STI) in the United States US each year appear in adolescents and grown-ups ages 15 to 24.
- Gonorrhea, the second most general sexually transmitted infection (STI), has continued to raise with more than half a million cases observed in 2018. This numerical rate represents a two-fold raise since 2014.
- In most cases, sexually involved adolescents and grown-ups with gonococcal infections of the genital tract, rectum, and pharynx are asymptomatic.
- Between 0.5 and 3% of hidden and untreated mucosal infections can result in the hematogenous transmission of Neisseria gonorrhoeae. Bacteremia leads to the attack of skin and joints or junctions manifesting as disseminated gonorrhea infection also known as arthritis-dermatitis syndrome. Women (during pregnancy and menstruation) and people with complement disorder (e.g., lupus and immunosuppressive treatment) are at a higher risk of the syndrome.
Host factor
factors include:
- Incidence
- Sex
- Age
- Psychosocial factors
- Menstruation
- Pregnancy
- Site of initial colonization
- Asymptomatic infection
- Complement deficiency
What are the Symptoms of Arthritis-dermatitis syndrome?
The symptoms of Arthritis dermatitis syndrome generally occur two to three weeks after the genitourinary infection, although in a few patients the initial genitourinary illness does not cause any symptoms.
Main symptoms
Patients who develop Arthritis dermatitis syndrome generally experience one of two types of symptoms. In the first type of characterized, known as “arthritis-dermatitis syndrome,” patients have a combination of skin symptoms and pain in multiple joints or junctions and tendons. In the second type of display, known as “purulent arthritis,” patients generally only develop aches in one or a few joints or junctions with substantial swelling. More details on these symptoms are listed below:
Joint pain:
Joint pain can be seen in both varieties of disseminated gonococcal infections. In arthritis-dermatitis syndrome, joint pain generally involves multiple joints or junctions throughout the body, and may “move” from one joint or junctions to the next.
Tendon pain:
Patients with arthritis-dermatitis syndrome can develop aches in the tendons, which are difficult, fibrous bands in our body that attach muscles to bones. The tendons that are involved are generally in the arms. You may feel pain in the front of your forearms when you flex your fingers.
Small fluid-filled bumps on the skin:
Many patients with the arthritis-dermatitis syndrome form of disseminated gonococcal infection will develop skin results. The most general skin results are small fluid- or pus-filled bulges, generally located on the hands or feet. This bulge generally lasts three to four days and then disappears without management. In a few cases, patients may have red spots, increased red bumps, large fluid-filled bulges, or other skin results.
Fever and chills:
Some patients with Arthritis dermatitis syndrome may develop a fever and chills near the start of the infection. This is more general in the arthritis-dermatitis syndrome form of disseminated gonococcal infection.
Presenting signs
Skin lesions-
- On investigation, 47% to 80% of people with arthritis dermatitis syndrome have specific skin lesions, which begin in tiny pink or red macules that blanch with stress.
- They differ from one to 20 mm in diameter.
- They move to the papular, vesicular, petechial, and pustular phases with or without a necrotic center and generally have a hemorrhagic bottom.
- Pustules may damage to create shallow ulcers. Rarely, large bullae may appear.
- In starting phase, the lesions are nonpruritic, painless, and generally seen during the first few days of infection.
- They occur at a small numerical rate and are unevenly divided on the trunk and extremities or limbs, involving the palmar and plantar surfaces.
- The most general site is the distal part of the extremities or limbs near the periarticular location.
- The face, scalp, and oral mucosa are generally not affected.
- Lesions are frequently seen in different phases of development and resolve within four to five days, generally without scarring.
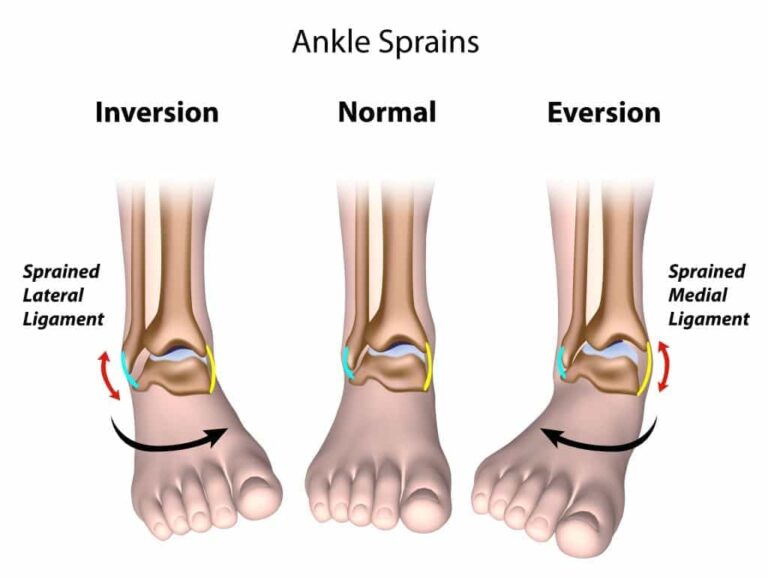
Tenosynovitis and arthritis:
- The connective tissue indication of arthritis dermatitis syndrome involves both tenosynovitis and suppurative arthritis.
- Clinical measures differentiating these two commodities are not clear in the largest case research we reviewed.
- Admittedly, tenosynovitis of arthritis dermatitis syndrome is transitory and migratory, creating a standardized assessment hard.
- In some cases, distinguishing tenosynovitis from suppurative arthritis may be unthinkable without a diagnostic aspiration conducted by a skilled clinician.
- Because of the problem in assessing tenosynovitis, some reports have shown more than defining details.
- There is an understanding that the hand and fingers are included in half of the people with tenosynovitis.
- Tenosynovitis includes the wrist in a quarter of people; the ankle joint and knee joint in less, and the foot, elbow, and shoulder in even less.
- Suppurative arthritis in arthritis dermatitis syndrome can be explained by a large suppurative effusion (WBC, 30,000 to 80,000/ JUL) most frequently of the knee.
- Suppurative arthritis less frequently includes the wrist joint, ankle joint, and elbow joint and rarely the hip and shoulder.
Mucosal signs:
- Although the primary mucosal infection in arthritis dermatitis syndrome is generally asymptomatic, a quarter to a half of people in whom the urethra and cervix are observed have genitourinary signs of the primary illness.
- Infections of the rectum and pharynx are generally asymptomatic and are not observable in clinical studies.
Systemic signs:
- Most arthritis dermatitis syndrome peoples have no fever or chills.
- If positive, fever is infrequently greater than 39 °C.
- This is in notable contrast to other bacterial arthritides.
What are the Causes of Arthritis-dermatitis syndrome?
There are various factors that may raise the risk of developing Arthritis dermatitis syndrome detailed below. It should also be informed that Arthritis dermatitis syndrome occurs more often in patients younger than 40 years of age and in women.
Untreated genitourinary Neisseria gonorrhoeae infection
The primary cause of Arthritis dermatitis syndrome is untreated genitourinary Neisseria gonorrhoeae infection. This can occur because most patients of genitourinary Neisseria gonorrhoeae infection do not cause any symptoms, particularly in females (more than 95 percent of the time). Therefore, the patient may have Neisseria gonorrhoeae infection without realizing it and not seeking management.
Recent menstruation
Recent menstruation in a female with a Neisseria gonorrhoeae infection may raise the risk of developing Arthritis dermatitis syndrome. The proper reason for this is undefined, but it may be due to differences in the female’s body and in the Neisseria gonorrhoeae bacteria during menstruation that make the bacteria more likely to transmit.
Pregnancy or recent childbirth
Owning a Neisseria gonorrhoeae infection while pregnant or if you have recently given birth also raises the risk of developing Arthritis dermatitis syndrome. This may be due to modifications to the immune system during pregnancy that make it more possible for Neisseria gonorrhoeae to transmit.
Deficiency in a particular part of the immune system
Some patients have a defect in a particular part of the immune system known as the complement system. The complement system is a part of the immune system that affects certain bacteria like Neisseria gonorrhoeae. Therefore, having a defect in the complement system raises the risk of developing Arthritis dermatitis syndrome.
Being infected with a more aggravated strain of Neisseria gonorrhoeae
A few strains of Neisseria gonorrhoeae have particular factors that assist them to avoid the body’s immune system and transmit throughout the body. Being infected with one of these more aggravating strains of Neisseria gonorrhoeae can raise the risk of developing Arthritis dermatitis syndrome.
Major clinical aspects of disseminated
- gonococcal infection
- Sex
- Women are involved three to five times more frequently than men
- Asymptomatic
- Mucosal sites of the primary infection are generally asymptomatic, but cultures of one or more sites are generally positive
- Antibiotic management
- Effects rapid improvement
- Two major patterns of disorder
- Tenosynovitis-dermatitis (group 1)
- Tenosynovitis and typical skin lesions are present
- Blood cultures are positive in <40%
- May be managed with oral antibiotics on an ambulatory basis (if compliant people)
- Suppurative arthritis (group 2)
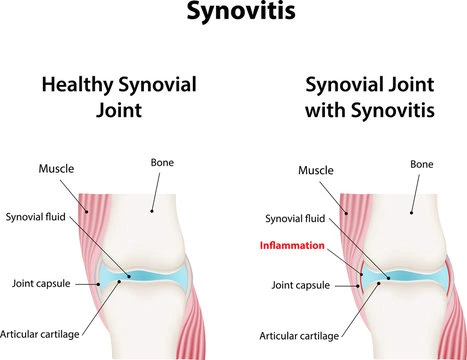
- Purulent synovial fluid aspirated
- Synovial fluid cultures are positive in <50%
- Blood cultures negative
- Persistent effusion managed with repeated aspiration
- Hospitalization
Diagnosis
MRI can also be produced to examine tenosynovitis. Point-of-care ultrasound (POCUS) can be beneficial for prompt diagnosis of tenosynovitis. POCUS can assist localize swelling in the tendon sheath, thus promoting an earlier diagnosis. This can assist distinguish between abscess, cellulitis, tenosynovitis, joint effusions, and tendon sheath effusions.
Treatment of Arthritis-dermatitis syndrome
Medication
- Aqueous crystalline penicillin G (10 million units, administered intravenously, per day) until progress occurs, followed by amoxicillin (500 mg) or ampicillin (500 mg) by mouth, four times a day, to finish at least seven days of antibiotic treatment
- Amoxicillin (3.0 g) or ampicillin (3.5 g) by mouth, each with probenecid (1.0 g) followed by amoxicillin (500 mg) or ampicillin (500 mg) by mouth, four times a day for at least seven days
- Tetracycline HCl (500 mg) by mouth, four times a day, for at least seven days, but not for involved gonococcal infections in pregnant female
- Cefoxitin (1.0 g) or cefotaxime (500 mg) given four times a day, intravenously, for at least seven days—the treatment of selection for this syndrome caused by penicillinase-producing iV gonorrhea (PPNG)
- Erythromycin (500 mg) by mouth, four times a day for at least seven days.
Antibiotics
All patients who develop Arthritis dermatitis syndrome require to be treated with a course of antibiotic medications. The particular drugs used may vary based on the doctor or physician’s preferences and the particular strain of the organism causing the infection. Still, most patients will be managed with ceftriaxone (Rocephin), which is delivered intravenously or injected into the muscle, and azithromycin (Zithromax), which is given as a pill. Antibiotics are generally continued for one to two weeks until symptoms enhance.
Drainage of joint fluid
Patients with Arthritis dermatitis syndrome who have joint or junction swelling may benefit from having the liquid drained from the joint or junction. Drainage of the liquid should decrease some symptoms and may assist in the diagnosis of the infection. The fluid is generally first drained by using a syringe. If the fluid cannot be fully drained with a syringe, a surgical method may be used to empty the fluid.
Test and treatment of sexual partners
In most patients with Arthritis dermatitis syndrome, your doctor or physician may suggest that you try to contact any sexual partners you have had in the last 60 days to offer them examination and potential management options for Neisseria gonorrhoeae infection. Since most people with Neisseria gonorrhea infections do not cause any symptoms, this can assist to catch Neisseria gonorrhoeae infections early and control them from transmitting.
Physiotherapy treatment
Walking
It’s free for you, you can do it basically anywhere, no particular training is required, and it’s comfortable on sore joints or junctions. Walking can assist you to keep a healthy weight or losing weight, resulting in less pressure on your joints. In extra, walking can enhance your heart health and bone health. The cardiac advantage of exercise is particularly important for patients with arthritis, as the condition is known to raise the risk of heart disorder.

Swimming
The water is a wonderful place to stretch your muscles and soothe your joints or junctions, so go to the pool for an aerobic workout. Swim laps, or try water walking or a water aerobics course.16 weeks of water-based activity in females with arthritis led to marked improvements in joint or junctions and other pain, as well as lowered disorder activity when compared with the significance of land-based aerobic activities. Swimming assists to boost mood, controlling weight, and enhancing sleep, and it’s better for overall health.
Strength Training
For patients with arthritis, certain joint or junctions pain triggers can make symptoms severe. But the build-up your muscles are, the less pressure there is on your joints. So don’t be scared of weights, because they’re a good way to get build up and boost muscle mass. For older adults with arthritis, aerobic and resistance activities combined can enhance endurance, aerobic capacity, and strength.
Experiment with free weights, weight machines, and resistance bands. Begin slowly and raise your intensity gradually. The goal for two or three days a week, doing eight to 10 various exercises that work various large muscle groups across your body. You can do two or three sets of eight to 12 repetitions per activity. Of course, if you feel pain or ache, come back off a little.
Cycling
Cycling is a good form of aerobic activity that’s easy on the joints or junctions. But it does arrive with the chance of falling, so it’s essential to get the right variety of bikes for your body. Looking into recumbent bikes, comfort bikes (cruisers), mountain bikes, or hybrid bikes, all of which have well stability and handling.

Yoga and Tai Chi
When a joint or junction and its surrounding muscles are involved by arthritis, the result is frequent position awareness, impaired coordination, balance, and a raised risk of falling, which is why patients complain of their ‘knees giving out’ with exercise. Yoga and tai chi are examples of activities that enhance body awareness, which can raise coordination and balance, a sense of where joints or junctions are positioned (proprioception), and relaxation. Plus, they involve flexibility and range-of-movement moves, which boost joint or junction flexibility and function, according to the CDC.
Pilates
Pilates focuses on building up and enhancing control of muscles, providing you with a low-impact workout that may decrease pressure on your hips and other joints or junctions. Pilates can also be beneficial in managing pain or ache and coping with the symptoms of arthritis. Cautions patients to hold to their own pace in a Pilates class and ask the informer about progression if arthritis symptoms are affecting them. Balance exercises like walking backward or standing on one foot are also useful for promoting balance and avoiding falls. Just be mindful that you may require to modify some postures to lessen pressure on joints or junctions and possibly combines props to assist with your balance.
Differential diagnosis
The differential diagnosis for the syndrome involves:
- nongonococcal polyarticular septic arthritis
- bacterial endocarditis
- viral arthritis
- meningococcemia
- Up to 40% of cases of meningococcemia have articular symptoms; meningococcus-associated arthritides are nearly always sterile and present either as a monoarticular or polyarticular condition.
- Postinfectious forms of arthritis (acute rheumatic fever and reactive arthritis) also can be hard to determine from the syndrome early in their course. Both can begin suddenly and be associated with fever; tenosynovitis is frequently noted in reactive arthritis, as it is in the syndrome.
Prognosis
The prognosis of arthritis in the syndrome is considerably more clear than that of nongonococcal septic arthritis, with full recovery in almost all people after the institution of proper antibiotic therapy.
FAQ
What are the main causes of dermatitis?
A general cause of dermatitis is a connection with something that upsets your skin or triggers an allergic reaction — for example, perfume, poison ivy, lotion, and jewelry involving nickel.
Is there a link between dermatitis and arthritis?
Atopic dermatitis is associated with a raised risk for rheumatoid arthritis-RA and inflammatory bowel condition, and a reduced risk for type 1 diabetes
What happens if dermatitis is untreated?
Bacterial skin infections
As atopic eczema can cause your skin to start cracking and breaking, there’s a risk of the skin starting infected with bacteria. The risk is higher if
you irritate your eczema or do not use your treatments properly. Signs of a bacterial infection can involve fluid oozing from the skin.
What underlying conditions cause dermatitis?
Other causes of dermatitis involve a viral infection, dry skin, stress, genetic makeup, bacteria, and an issue with the immune system.
What vitamin deficiency is dermatitis?
Dermatitis is characterized by erythematous, itchy, vesicular, edematous, flaking, weeping, and crusting patches of skin. Protein, niacin (vitamin B3), essential fatty acids, and zinc defects can result in dermatitis.






One Comment