Bruxism (Teeth grinding)
What is bruxism?
- Bruxism is a condition in which grinding and clenching of the teeth. If the patient has suspected of bruxism, he/she may unconsciously clench the teeth during wake up in the morning and clench or grind the teeth during sleep.
Type of the bruxism
- Sleep bruxism is shown as a sleep-related movement disorder. People who clench or grind their teeth (brux) during sleep are more likely to have other sleep disorders, like harsh sounds and pauses in breathing sleep apnea. sleep bruxism knew as nocturnal bruxism
- Occurrence: While asleep, mostly during periods of the sleep period
- Time-intensity relationship: Pain aggravates on waking, then slowly gets better grinding of the teeth
- Relationship with stress: little evidence of a relationship
- Gender distribution: Equal gender distribution
- Hereditary: Some evidence
- Mild bruxism may not require treatment. However, in some people, the bruxism can be frequent and severe enough to lead to jaw disorders, headaches, damaged teeth, and other connected problems. Because the patient might have sleep bruxism and be unaware of it until some complications develop
- Awake bruxism: the patient clenches her/his jaw and grinds his/her teeth during the day with awake bruxism condition. It’s generally fixed to emotional issues. Feeling fearful, stressed, or angry can lead to teeth grinding. But also can concentrate on something. Awake bruxism generally doesn’t need treatment, if the patient is more likely to notice the bruxism and try to do prevention steps against that. Stress management can help to reduce bruxism and learning ways for stress management should also help reduce the frequency.
- Time-intensity relationship: Pain worsens throughout the day, and not be present upon waking
- Noises: Rarely associated
- Activity: generally clenching, occasionally clenching and grinding
- Relationship with stress: Stronger evidence for a relationship, but not conclusive
- Gender distribution: Mostly females
- hereditary: unclear
Classification of bruxism by cause
- Alternatively, bruxism can be subdivided into primary bruxism which is also termed “idiopathic bruxism”, where the disorder is not connected to any other medical condition, and secondary bruxism, where the disorder is connected with other medical conditions. Secondary bruxism involves iatrogenic causes, like the side effect of prescribed medicines. a further source of bruxism divides the causes of bruxism into three groups, namely central or pathophysiological factors, psychosocial factors, and peripheral factors. listing “tooth grinding” under somatoform disorders which group of psychiatric disorders in which patients present with an infinite of clinically significant disorders but unexplained physical symptoms.
Classification of bruxism by severity
- The ICSD-R classified three different severities of sleep bruxism
- mild bruxism which occurs less than at the night, with no damage to teeth or psychosocial impairment
- moderate bruxism which occurs at night, with mild impairment of psychosocial functioning
- severe bruxism which occurs at the night, with damage to the teeth, temporomandibular disorders, other physical injuries, and severe psychosocial impairment.
Classification of bruxism by duration
- The ICSD-R classified three different types of sleep bruxism according to the duration the condition is present,
- acute bruxism lasts for less than one week
- subacute bruxism lasts for more than a week and less than one month
- chronic bruxism lasts for over a month
- the overall prevalence of bruxism is 8 percent to 31 percent
- awake bruxism prevalence is 22.1 to 31 percent
- sleep bruxism prevalence is 9.7 to 15.9 percent
- Children are reported to brux as generally as adults. It is possible for sleep bruxism to occur as early as the first year of life after the first teeth appear in the mouth termed deciduous incisors, and the overall prevalence in children is about 14 to 20 percent. Sleep bruxism occurs in over 50 percent of normal infants. generally, sleep bruxism develops during adolescence the phase of life between childhood and adulthood, from ages 10 to 19, and the prevalence in 18- to 29-year-olds is appro about 13 percent. The overall prevalence in adults is reported to be 8 percent, and people over the age of 60 are less likely to be affected, with the prevalence dropping to about 3 percent in the old group.
Signs and symptoms of the bruxism
- Increased tooth pain or sensitivity
- a locked jaw that will not open or close perfectly
- the Jaw, the neck, or face pain or soreness
- dislocation of the jaw
- Pain that feels like impaired hearing, though it’s actually not a problem with your ear
- Damage from chewing activity on the inside of the cheek
- most people who have bruxism are not aware of this problem, either because there are no symptoms, or because the symptoms are not understood to be connected with a clenching and grinding problem
- View from an anterior part front tooth showing severe tooth wear which has exposed the dentin layer normally covered by enamel. The pulp chamber is observable through the overlying dentin. The third dentin layer will have laid down by the pulp in response to the loss of tooth substance. Multiple fracture lines are also visible.
- Other parafunctional activities which may happen together with bruxism are cheek biting which may be definite as chronic cheek biting and linea alba and lip biting.
- A burning sensation on the tongue is termed glossodynia, possibly related to a simultaneously “tongue thrusting” parafunctional activity.
- tooth cupping( indentation) is the destruction that forms small cups of the teeth and changes the looks of the tongue which is termed a crenated tongue
- Hypertrophy of the muscles of mastication increases in the size of the muscles that move the jaw, particularly the masseter muscle.
- Tenderness, pain, or fatigue of the muscles of mastication, may get worse during chewing or another jaw movement
- Trismus restricted mouth opening
- Pain or tenderness of the temporomandibular joints, which shows as preauricular pain in front of the ear, or pain referred to the ear (otalgia)
- Clicking of the temporomandibular joints.
- Headaches, particularly pain in the temporalis, are caused by muscle pain associated with the temporalis muscle.
- Excessive tooth wears particularly attrition, which flattens the occlusal (biting) surface, but also possibly other types of tooth wear such as abstraction, where notches form around the neck of the teeth at the gum line.
- Tooth fractures, repeated failure of dental restoration fillings of the dental cap, etc.
- Hypersensitive teeth, dental pain when drinking a cold liquid caused by wearing away of the thickness of insulating layers of dentin and enamel around the dental pulp connective tissue that resides within the center of the tooth, directly under the layer of dentin.
- Inflammation of the periodontal ligament of teeth, which should make the teeth painful to bite on, and possibly also a degree of loosening of the teeth.
- Bruxism is usually detected because of the effects of the process most commonly tooth wear and pain, rather than the dental process itself. The large forces that can be generated during bruxism can have adverse effects on the components of the masticatory system, namely the teeth, the periodontium, and the articulation of the mandible with the skull and the temporomandibular joints. The muscles of mastication that act to move the jaw can also be affected since they are being utilized beyond the above-normal function.
Pain
- Most people with bruxism should experience no pain. The presence of pain and degree of pain does not efficiently correlate with the severity of grinding or clenching. The pain in the muscles of mastication caused by bruxism can be parallel to muscle pain after exercise. The pain may be felt over the angle of the jaw masseter muscle or in the temporalis and may be described as a headache or an aching jaw. Most bruxism but not all bruxism involves clenching force given by the masseter and temporalis muscle groups; but some bruxers who have bruxism habitually clench and grind the front of his/her teeth only, which involves less action of the masseter and temporalis muscles. The temporomandibular joints may also become painful, which is usually felt just in front of the ear, or inside the ear. Clicking of the jaw joint may also develop temporomandibular joint pain. The forces utilized on the teeth are more rather than what the periodontal ligament is organically designed to handle, so the result occurs as inflammation of the ear. A tooth may become painful to bite on, tooth wear may reduce the wrapping width of the enamel and dentin layer that protects the pulp connective tissue of the tooth and result in hypersensitivity, too cold stimuli.
- The relationship of bruxism with temporomandibular joint dysfunction or temporomandibular pain dysfunction syndrome is discussed. sleep bruxism can be a causative or contributory factor to pain symptoms in temporomandibular joint dysfunction In fact, the symptoms of temporomandibular joint dysfunction overlap with bruxism. Others people suggest that there is no strong association between temporomandibular joint dysfunction and bruxism. the possible relationship included that when self-reported bruxism is used to diagnose bruxism, there is a positive connection with temporomandibular joint dysfunction pain, and when lots of diagnostic criteria for bruxism are used, the connection with temporomandibular joint dysfunction symptoms is much lower. In severe, chronic cases, bruxism can lead to happen myofascial pain and arthritis of the temporomandibular joints.
Tooth wear
- Many people list tooth wears as the effect of bruxism, but some report a lack of a positive relationship between tooth wear and bruxism. Tooth wear caused by tooth to tooth contact is known as attrition. This is the most usual type of tooth wear that happens in bruxism and affects the occlusal surface of the teeth. The exact location and pattern of attrition depend on how the bruxism occurs, e.g., when the canines and incisors of the antagonistic arches are moved against each other laterally, by the action of the medial pterygoid muscles, which can lead to the wearing down of the incisal edges of the teeth. To grind the front teeth, the patient needs to posture his/her mandible forwards, unless there is an existing edge-to-edge, class 4 incisal relationship. People with bruxism may also grind their posterior teeth back teeth, which wears down the cups of the occlusal surface. Once tooth wear progresses through the enamel dentin layer, the exposed dentin layer is much softer and more accessible to wear. If the tooth is worn away or ruined enough, the tooth will effectively be weakened and may fracture under the increased forces that occur in bruxism.
- Abfraction is another type of tooth wear that is accepted to happen with bruxism, although some people still argue whether this type of tooth wear is a reality. Abfraction cavities are said to occur generally on the facial aspect of teeth, in the cervical area as V-shaped defects caused by flexing of the tooth under occlusal forces. It is not believed that the same lesions can be caused by long-term forceful brushing of the tooth. However, the fact that the cavities are V-shaped does not suggest that the damage is caused by toothbrush abrasion and that some fraction cavities occur below the level of the gum line, in an area covered by toothbrush abrasion, which supports the validity of this mechanism of tooth wear. In addition to attrition, erosion collectively contributes to tooth wear in some bruxists who have bruxism, according to some sources.
Tooth mobility
- The view that occlusal trauma as may occur during bruxism is a causative factor in gingivitis mild form of the gum that occurs around the base of the teeth and if the condition starts to get worse called periodontitis is not widely accepted It is thought that the periodontal ligament may respond to increased occlusal forces by absorb again some of the bone the alveolar crest, which may result in increased tooth mobility, however, these changes are reversible if the occlusal force is reduced. Tooth movement that occurs during occlusal surface loading is sometimes termed fremitus It is generally accepted that increased occlusal forces are able to increase the rate of progression of pre-existing periodontal disease (gum disease), however, the mainstay treatment is plaque control rather than elaborate occlusal adjustments. It is also generally accepted that periodontal disease is a far more common cause of tooth mobility and pathological tooth transfer rather than any influence of bruxism, although bruxism may much less commonly be involved.
- take an appointment with your doctor if you have any of the symptoms listed above or have other concerns about the teeth or jaw.
- If you observe that your child is grinding his or her teeth or has other signs or symptoms of bruxism be sure to take your child’s next dental appointment.
Causes of the teeth grinding
- There are many causes of bruxism, involving modern Lifestyle habits, like drinking alcohol, using cigarettes and recreational drugs, and consuming a lot of caffeine more than six cups of coffee in a day. People who drink alcohol and smoke twice a day equally grind their teeth as they don’t drink and smoke but grind the teeth are also the same causative factors.
- Sleep disorders.
- Stress and anxiety.
- Taking certain medications, including a drug class of anti-anxiety drugs called selective serotonin reuptake inhibitors.
- the muscles of mastication the temporalis, masseter, medial, and lateral pterygoid muscles are paired on either side and work together to move the mandible, which turns and slides surrounding its double articulation with the skull at the
- temporomandibular joints. Some of the muscles work to elevate the mandible close to the mouth, and other muscles also are involved in lateral side-to-side, protrusive, or retractive movements. Mastication (chewing) process is a much more complex neuromuscular activity that could be controlled either by subconscious processes or by conscious processes. In individuals without bruxism or other parafunctional activities, during alertness, the jaw is usually at rest and the teeth are not in contact, except while speaking, swallowing, or chewing activity. It is estimated that the teeth are in contact for less than 20 minutes per day, mostly during chewing and swallowing tasks. Normally during sleep, the spontaneous muscles are inactive due to physiologic motor paralysis, and the jaw is usually open.
- Some bruxism activity is rhythmic with bite force pulses of the 10th of a second while chewing, and some have longer bite force pulses of 1 to 30 seconds while clenching. Some individuals clench their teeth without significant lateral movements. Bruxism can also be marked as a disorder of repetitive, unconscious contraction of muscles. This typically involves the masseter muscle and the anterior portion of the temporalis which is a large outer muscle that is responsible for clench, and the lateral pterygoids, relatively small bilateral muscles that act together to perform the movement sideways grinding.
Psychosocial factors
- the significant psychosocial risk factors for bruxism, particularly a stressful lifestyle, and this evidence is growing up, but still not conclusive. Some people consider bruxism due to emotional stress and anxiety to be the main triggering factors. persons with bruxism respond very differently to depression, opposition, and stress compared to people without bruxism. Stress has a major role and stronger relationship to awake bruxism, but the role of stress in sleep bruxism is less clear, with states that there is no evidence for a relationship with sleep bruxism. However, children with sleep bruxism have been shown to have greater levels of anxiety rather than other children with awake bruxism. People aged 50 years with bruxism are more likely to be single and have a high level of education. Work-related stress and irregular work shift like changes in the shifts of jobs also be involved. Personality mindsets are also commonly considered the causes of bruxism such as aggressive nature, competitive, or hyperactive personality types, and relaxed anger or frustration can contribute to bruxism. Stressful periods like examinations, family distress, marriage, divorce, or relocation have been suggested to increase bruxism. Awake bruxism generally occurs during periods of concentration such as while working at a computer, driving, or reading. the link between bruxism and psychosocial factors. electrically shock occurred at the laboratory, and then observed high levels of bruxism-like muscular activity in rats that were allowed to watch this treatment compared to rats that did not see the muscular activity. the rats affected by the electrical shock the other rats were going to under emotional stress due to show the effect of electric shock which may cause the bruxism-like behavior
Genetic factors
- there may be a degree of inherited susceptibility to develop sleep bruxism.21 to 50 percent of people with sleep bruxism have a direct family member who had sleep bruxism during childhood, suggesting that there are genetic factors involved, despite no genetic markers have been found yet. the Offspring of people who have sleep bruxism are more likely to bear a child who has sleep bruxism rather than children of people who do not have bruxism. major children of people show awake bruxism rather than sleep bruxism. but related to the offspring sleep bruxism plays a major role rather than awake bruxism
Diagnosis of the bruxism
- During regular dental exams, the physician likely will check for signs of bruxism.
Evaluation of the bruxism
- physicians can generally diagnose bruxism based on physical examination and symptoms. But in some cases, you may need a sleep study called polysomnography shows increased masseter and temporalis muscular activity during sleep Polysomnography may involve electroencephalography, electromyography, electrocardiography, airflow monitoring, and audio–video recording. It should be useful to help exclude other sleep disorders; however, due to the expense of the use of a sleep lab, polysomnography is mostly of significance to research rather than the routine clinical diagnosis of bruxism. polysomnography test takes place in a sleep center clinic and provides a definitive diagnosis. such as sleep apnea, or other condition related to bruxism
- Determining the cause of the bruxism
- If the physician suspects the bruxism, he or she tries to determine its cause by asking questions about general dental health, medications, daily routines, and sleep habits.
- To evaluate the degree of bruxism, the physician may check for
- Tenderness in the jaw muscles
- visible dental abnormalities, such as broken or missing teeth
- Other conditions like damage to the teeth, the underlying bone, and the inside of the cheeks, usually with the help of X-rays
- A dental exam may detect other disorders that can cause related jaw or ear pain, such as temporomandibular joint disorders, other dental problems, or health conditions
- If the bruxism seems to be related to major sleep issues, the doctor may recommend a sleep medicine specialist. A sleep medicine specialist should plan more tests
- If anxiety or other psychological issues seem to be related to your teeth grinding, the patient should be assigned to a licensed therapist
ICSD-R diagnostic criteria
- The ICSD-R recorded the diagnostic criteria for sleep bruxism. The minimal criteria involve both of the following:
- symptom of teeth grinding or teeth clenching during sleep, and
- One or more of the following:
- Abnormal tooth wear
- Grinding sounds
- The discomfort of the jaw muscles
- The following criteria help the diagnosis:
- polysomnography shows both The activity of jaw muscles during sleep and No associated epileptic activity
- No other medical or mental disorders like sleep-related epilepsy, which may cause abnormal movement during sleep.
- The presence of other sleep disorders obstructive sleep apnea syndrome
Treatment for the bruxism
- In many cases of bruxism treatment shouldn’t be essential. Many children prevent bruxism without any treatment, and many adults don’t grind or clench their teeth badly which is not enough to take any kind of therapy. However, if the problem is severe, options involve certain dental approaches, therapies, and medications to prevent more tooth damage and relieve jaw pain or discomfort
- talk with your physician they told you which treatment is best for you
Medications
- In general, medications should not very effective for the treatment of bruxism, and more research is needed to determine the effectiveness of the medication. some drugs Examples of medicines that may be used for bruxism include:
- Muscle relaxants: In some cases, the doctor may suggest taking a muscle relaxant before bedtime, for a short period of time.
muscle relaxants for the bruxism
Cyclobenzaprine
- cyclobenzaprine acts on the central nervous system to generate its muscle relaxant effects. Its actions on the central nervous system may also cause some of this medicine’s side effects.
cyclobenzaprine use For relaxing stiff muscles:
- For oral dosage form expanded-release capsules: for adults—15 milligrams (mg) once a day. Some patients should need one 30 mg capsule or a division of two 15 mg capsules per day.
- Children—Use and dose must be prescribed by your doctor.
- oral route dosage for Adults and children 15 years of age and older—10 (mg) 3 times in a day. The largest amount for oral dose should not exceed more than 60 mg per day.
- Children younger than 15 years of age—Use and dose must be decided by the doctor.
Symptoms of overdose
- Convulsions (seizures)
- drowsiness (severe)
- dry, hot, flushed skin
- fast or irregular heartbeat
- hallucinations seeing, hearing, or feeling things that are not available
- increase or decrease in body temperature
- troubled breathing
- unexplained muscle stiffness
- unusual nervousness or restlessness (severe)
- vomiting occurring together with symptoms of overdose
Diazepam
- Diazepam is used to relieve symptoms of anxiety Diazepam is a benzodiazepine. Benzodiazepines belong to the group of medicines known as central nervous system depressants, which are medicines that slow down the nervous system.
- diazepam medicine should come with Medicine Guidance. Read and follow the instructions carefully
- Swallow the tablet whole. should not crush, break, and chew the diazepam
To use the oral solution:
- Measure the oral liquid with the medicine dropper which comes from the package.
- Mix each dose with water, juice, soda, or a soda-like beverage before taking it. You may also mix the liquid with semisolid food such as applesauce
- Take the entire mixture of the solution right away. the oral solution should not be saved to use later.
For oral dosage forms solutions or tablets
- For anxiety the dose of diazepam
- Adults:2 to 10 milligrams (mg) 2 to 4 times in the day.
- Older adults: 2 to 2.5 milligrams 1 or 2 times a day. the doctor should increase your dose if needed.
- Children 6 months of age and older:1 to 2.5 mg 3 or 4 times per day. the child’s doctor should increase the dose if needed.
- Children up to 6 months of age Use of diazepam is not recommended.
- Symptoms of an overdose involve: change or loss of consciousness, confusion, dizziness lightheadedness when getting up immediately from a lying or sitting position, irregular, fast or slow, or shallow breathing, lack of coordination, loss of strength or energy, muscle pain or weakness, blue lips, fingernails, or skin, steadiness, and unsteady walk, shaking, or other problems with is related to muscle control or coordination, sweating, difficulty in breathing, unusual drowsiness, dullness, tiredness, weakness or feeling of inactive, or unusual weak feeling.
- Some side effects may happen that generally do not need medical attention. These side effects should go away during treatment as your body adjusts to the medicine
Botox injections
- Injections of Botox, a form of botulinum toxin, should help some people with severe bruxism who shouldn’t respond to other treatments.
- Botox treatment for Bruxism is done in approx 10 to 15 minutes with results generally visible the next day.
- Effects will stay normally for 4 to 6 months or sometimes even longer.
- spontaneous movements, like chewing, and facial expressions, which are not affected by the Botox treatment.
- Although Botox injections are not a therapy for Bruxism, botox treatment should effectively control the discomforting symptoms associated with it.
The advantages of Botox injections for Bruxism
- lower grinding of the teeth and clenching of the jaw
- Reduced symptoms like headaches, earache, and facial pain.
- Enhanced sleep for both you and your partner- no noisy grinding
- Reduced teeth weakness, tooth wear, and fracture.
- Reduced prominence of the masseter jaw muscles.
- Quick, noticeable, long-lasting result.
- No healing time is needed you can return to work directly after the treatment.
- Botox treatment can be repeated after the results should disappear
The side effects after Botox treatment
- Most side effects are connected to the basic act of injecting the skin, rather than the Botox itself. The side effects involve minor redness, swelling near the injection site which disappears within 1 to 2 hours, and minor bruising.
- Some patients experience headaches and there is a very small risk of infection near the entry point, which is reduced with hygiene habits.
- In occasional cases, Botox injections in the jaw muscles temporarily reduce bite strength.
- Botox effect stays between 3-4 months.
- Results start to be observable between 1- 10 days.
- Positive Botox review needed 2 weeks following the initial procedure
- Medication for anxiety or stress: the doctor may recommend the short-term use of antidepressants which are classes from selective serotonin reuptake inhibitors (SSRIs). or anti-anxiety medications which are a class of serotonin and norepinephrine reuptake inhibitors ( SNRIs) to help you deal with stress or other emotional issues that may be causing the bruxism.
Antidepressants for the bruxism
citalopram
- Citalopram is utilized to treat depression, including major depressive disorder. It is an antidepressant that comes from a group of medicines known as selective serotonin reuptake inhibitors (SSRIs).
- Citalopram is available in tablets, solutions
- Citalopram should be taken with or without food
- If you should use the oral liquid, shake the bottle well before measuring each and every dose. use a pointed measuring spoon, oral syringe, or medicine cup to measure each and every dose
oral dosage forms for the capsule
- For depression
- Adults—30 milligrams one time a day. the doctor should adjust the dose as required. Do not start treatment with citalopram capsules because the only available dose power is 30 mg. Use another dosage form of citalopram for example solution or pills for initiating treatment and altering doses rather than 30 mg one time in a day.
- Older adult usage of citalopram is not advised.
oral dosage forms for solution or tablets
- For depression:
- Adults—At the first time, 20 milligrams (mg) one time a day, given either in the morning or evening. the doctor should change the dose as required. However, the dose is not generally more than 40 mg per day.
- Older adults—20 mg one time a day, taken either in the morning or evening.
- more common side effects of the citalopram are: reduction in sexual passion or capacity of tiredness or uncommon sleepiness
Escitalopram
- Escitalopram is useful to treat depression and generalized anxiety disorder. It is an antidepressant that comes from a group of medicines known as selective serotonin reuptake inhibitors (SSRIs).
For oral dosage forms (solution or tablets):
- For depression:
- Adults and children 12 years of age and older—10 milligrams (mg) one time a day, taken either in the morning or evening. the doctor may change the dose as required. However, the dose is generally not more than 20 mg per day.
- Older adults—10 mg one time a day, taken either in the morning or evening.
- Children younger than 12 years of age use and dose must be decided by the doctor.
- For generalized anxiety disorder:
- Adults—10 milligrams (mg) one time a day, taken either in the morning or evening. However, the dose is not generally more than 20 mg per day.
- Older adults—10 mg one time a day, taken either in the morning or evening.
side effects of the escitalopram
- Diarrhea
- dry mouth
- heartburn
- sleepiness
- problem in sleeping
Paroxetine
- Paroxetine is used to treat depression, generalized anxiety disorder,
- Paroxetine comes from a group of medicines known as selective serotonin reuptake inhibitors (SSRIs).
For oral dosage form rest:
- For depression:
- Adults: At the first time, 20 milligrams (mg) 10 ml once a day, are generally taken in the morning. However, the dose is not generally more than 50 mg (25 mL) per day.
- Older adults: At the first time, 10 mg (5 mL) once a day, generally taken in the morning. However, the dose is generally not more than 40 mg (20 mL) per day.
- For generalized anxiety disorder:
- Adults: At first, 20 milligrams (mg) (10 ml) once a day, generally taken in the morning. However, the dose is generally not more than 50 mg (25 mL) per day.
- Older adults: At the first time, 10 mg (5 mL) one time a day, usually taken in the morning. However, the dose is generally not more than 40 mg (20 mL) per day.
The more common side effect of the paroxetine
- Acid or sour stomach
- belching
- decreased appetite
- heartburn
- pain or tenderness surrounding the eyes and cheekbone
- passing gas
- problems with urinating
- runny or stuffy nose
- sleepiness or unusual drowsiness
- stomach discomfort or upset
- trouble sleeping
Fluoxetine (Prozac)
- Fluoxetine is used to treat depression, Fluoxetine is an antidepressant, and comes to a group of medicines known as selective serotonin reuptake inhibitors (SSRIs).
- fluoxetine is available in the following dosage forms: Capsule, Delayed Release, Syrup, Table, Capsule, Solution
For depression:
- Adults—At the first time, 20 milligrams (mg) once a day in the morning. . If you are taking more than 20 mg per day, you may take the capsule one time a day in the morning or 2 times a day for example morning and noon. However, the dose is generally not more than 80 mg per day.
- Children 8 years of age and older—At the first time, 10 or 20 mg once a day in the morning.
- For the children: all the antidepressant drugs and doses decided by the doctor
- These selective serotonin reuptake inhibitors (SSRIs) are believed to work by elevating the activity of a chemical called serotonin in the brain.
More common side effects of fluoxetine
- itching, skin rash
- inability to sit still
- restlessness
anti-anxiety medications
- these anti-anxiety medications are supposed to work by elevating the activity of the chemical which is termed serotonin and norepinephrine in the brain
Desvenlafaxine
- Desvenlafaxine is used to treat depression. It comes to a group of medicines which is known as serotonin and norepinephrine reuptake inhibitors (SNRIs).
- For oral dosage form (extended-release tablets):
- For depression: Adults—50 milligrams (mg) one time a day. the doctor should adjust the dose as required.
More common side effects of the Desvenlafaxine
- Decreased appetite
- raised sensitivity of the eyes to light
- sleepiness or unusual drowsiness
- difficulty in sleeping
duloxetine
- Duloxetine is useful to treat depression and anxiety.
- Duloxetine drug comes from a group of medicines which is known as selective serotonin and norepinephrine reuptake inhibitors (SSNRIs).
For oral route dose
- For treatment of anxiety:
- Adults—At the first time, 60 milligrams (mg) one time a day. Some patients may start at 30 mg once a day for 1 week before increasing the dose to 60 mg one time a day. However, the dose is generally not more than 120 mg per day.
- Older adults—At the first time, 30 mg once a day for 2 weeks However, the dose is generally not more than 120 mg per day.
- Children 7 years of age and older—At the first time, 30 mg once a day for 2 weeks However, the dose is usually not more than 120 mg per day.
- Children younger than 7 years of age: use and dose must be decided by the doctor.
- For treatment of depression
- Adults—40 milligrams (mg) per day given as 20 mg two times per day to increase the dose to 60 mg per day given either one time a day or as 30 mg two times per day. However, the dose is generally not more than 120 mg per day.
More common side effects for Desvenlafaxine
- Body discomfort or pain
- cough
- difficulty having a bowel movement (stool)
- dry mouth
- ear congestion
- frequent urination
- headache
- lack or loss of strength
- loss of appetite
- loss of voice
- muscle aches
- nausea
- sleepiness or unusual drowsiness
- sneezing
- sore throat
- stuffy or runny nose
- sweating increased
- trouble sleeping
- weight loss
venlafaxine
- Venlafaxine is used to treat depression. It is also used to treat general anxiety disorder, and social anxiety disorder, Venlafaxine comes from a group of medicines known as serotonin and norepinephrine reuptake inhibitors (SNRI).
- For depression:
- Adults— 75 milligrams (mg) per day, taken as one dose in the morning or one dose in the evening. Some patients should need a starting dose of 37.5 mg per day, taken for 4 to 7 days. . However, the dose is generally not more than 225 mg per day.
- For generalized anxiety disorder:
- Adults—At the first time, 75 milligrams (mg) per day, taken as one dose in the morning or one dose evening. Some patients should need a starting dose of 37.5 mg per day, which is taken for 4 to 7 days. However, the dose is generally not more than 225 mg per day.
For oral dosage forms of tablets
- For depression:
- Adults—At the first time, a total dose of 75 milligrams (mg) per day, is divided the dose and taken 2 or 3 times during the day. However, the dose is generally not more than 225 mg per day.
More common side effects of venlafaxine
- decreased interest in sexual intercourse
- inability to have or keep an adjustment
- lack or loss of strength
- loss in sexual capability, passion, movement, or performance
- severe headache
- sweating
- for the children, all the anti-anxiety medications dose and use decided by the doctor
Tricyclic antidepressant for the bruxism
- tricyclic antidepressant drugs help to reduce depression with associated grinding of the teeth
amoxapine
- amoxapine can be used to treat more severe conditions of depression.
- Compared to similar medicines, amoxapine improves the mood in depression more quickly.
- amoxapine is available as a generic.
- While amoxapine should treat depression, you have to take it several times a day and it can make feel sleepy.
- It works on the central nervous system to increase levels of certain chemicals in the brain. amoxapine medicine comes from the tricyclic antidepressant drug
for oral dosage forms for tablets
- For depression:
- Adults: At the first time, 50 milligrams two or three times per day. the doctor should increase the dose as required. However, the dose is generally not more than 300 mg per day unless you are in a hospital. Some hospitalized patients require higher doses. I take amoxapine medicine once a day, before bedtime.
- Older Adults: 25 milligrams (mg) two or three times per day. However, the dose is generally not more than 300 mg per day
Symptoms of overdose of amoxapine
- Change in consciousness
- sleepiness
- an epileptic seizure that will not stop
- fatigue
- increased blood pressure
- increased hunger
- loss of consciousness
- swelling on the face, fingers,
- total body jerking
- disturbed in breathing
- weight gain
- dry mouth
Clomipramine
- Clomipramine is used to treat obsessive-compulsive disorder. obsessive-compulsive disorder is a nervous condition where in people have frequent thoughts or ideas or do repetitive things because of anxiety.
- Clomipramine is a tricyclic antidepressant. It is supposed to work in the brain by increasing the activity of the chemical called serotonin.
- dosage form: capsule
For oral dosage form for capsule
- For obsessive-compulsive disorder:
- Adults: 25 milligrams (mg) one time a day at bedtime. Higher doses may be given in smoothly divided doses during the day. However, the amount of dose is generally not more than 250 mg per day.
- Children 10 years of age and older: 25 mg once a day at bedtime. However, the amount of dose is generally not more than 200 mg per day.
side effects of clomipramine
- Bladder pain
- bloody or cloudy urine
- blurred vision
- body aches or pain
- burning, creeping, itching, numbness, pins, and needles, or tingling feelings
- confusion
- difficult, burning, or painful urination
- dizziness, lightheadedness when awake suddenly from a lying or sitting position
- excessive muscle tone
- fear or nervousness
- feeling sad
- fever
- hearing changes
- lumps, skin rash
- irritability
- poor concentration
- the rhythmic movement of muscle
- unusual tiredness or weakness
- voice changes
desipramine
- Desipramine is used to treat depression. desipramine works by raising the activity of a chemical named norepinephrine in the brain. desipramine is a tricyclic antidepressant.
For oral dosage forms for tablets
- For depression:
- Adults:100 to 200 milligrams (mg) one time a day or in divided doses during the day. However, the amount of the dose is generally not more than 300 mg per day.
- Older adults and teenagers:25 to 100 mg one time a day or in divided doses during the day. . However, the amount dose is generally not more than 150 mg per day.
imipramine
- Imipramine is used to treat depression. It comes to a group of medicines which is known as tricyclic antidepressants (TCA). These medicines are supposed to work by raising the activity of a chemical called serotonin in the brain.
- dosage form: tablet and capsule
For oral dosage form for capsule
- For depression:
- Adults:75 milligrams (mg) one time a day. However, the dose is generally not more than 200 mg per day, Some hospitalized patients may require higher doses.
- Teenagers and older adults: 25 to 50 mg per day using tablets However, the dose is generally not more than 100 mg per day.
For oral dosage form for tablet
- For depression:
- Adults— 75 milligrams (mg) per day. However, the dose is generally not more than 200 mg per day.
- Teenagers and older adults: 30 to 40 milligrams per day. However, the dose is generally not more than 100 mg per day.
- For bed rest
- Children 6 years of age and older: 25 milligrams (mg) one time in a day, taken 1 hour before bedtime.
Symptoms of overdose of imipramine
- The blue color of fingernails, lips, skin, palms, or nail beds
- cold, moist skin
- decreased awareness or responsiveness
- disorientation
- hallucinations
- irregular, fast, slow, breathing
doxepin
- Doxepin is useful to treat anxiety and depression.
- Doxepin is a tricyclic antidepressant (TCA). It works on the central nervous system to increase levels of specific chemicals in the brain.
- dose form: tablet, solution, capsule
For oral dosage forms capsules or solution
- For depression or anxiety:
- Adults and children 12 years of age and older:75 milligrams (mg) once a day or in divided doses during the day. However, the amount of the dose is generally not more than 150 mg per day.
- For children younger than 12 years of age; use is not advised.
Symptoms of overdose
- feeling awkward
- disturbed concentration
- drowsiness
- enlarged pupils
- increased or excessive unconscious
- low body temperature
- weak pulse
- weight gain
Nortriptyline
- it is used to treat depression. It is supposed to work by raising the activity of the chemical called serotonin in the brain. Nortriptyline is a tricyclic antidepressant.
- dose form: capsule, solution
For oral dosage forms for capsules or solution
- For depression:
- Adults:25 milligrams 3 to 4 times per day. . However, the amount of the dose is generally not more than 150 mg per day.
- Teenagers and older adults:30 to 50 milligrams (mg) one time a day or in divided doses during the day.
Symptoms of overdose
- cold, skin
- confusion
- decreased urine output
- enlarged neck veins
- extreme tiredness
- fainting
- fast, slow, or irregular heartbeat
- fast, weak pulse
- irregular breathing
- loss of consciousness
- restlessness
- seeing things that are not there
- seizures
Protriptyline
- it is used to treat depression. It is supposed to work by raising the activity of serotonin substance in the brain. protriptyline comes from the drug group tricyclic antidepressant (TCA).
For oral dosage forms for tablets
- For depression:
- Adults: 15 to 40 milligrams (mg) a day divided into three or four doses. . However, the dose is generally not more than 60 mg per day.
- Teenagers and Older Adults: 5 milligrams (mg) three times a day.
Trimipramine
- it is used to treat depression. It comes to the group of medicines known as tricyclic antidepressants (TCA)
For oral dosage form for capsule
- For depression:
- Adults: 75 milligrams (mg) per day, taken in divided doses. However, the amount of the dose is generally not more than 200 mg per day.
- Teenagers and older adults: 50 milligrams per day. However, the dose is generally not more than 100 mg per day.
- all the tricyclic antidepressant drugs dose are increased by the doctor as a requirement of the patient
Precaution for medication
- Do not bring the medication with a monoamine oxidase inhibitor (eg, isocarboxazid, linezolid ), methylene blue injection, phenelzine, selegiline, or tranylcypromine. Do not start taking the drugs during the 2 weeks after you stop a monoamine oxidase inhibitor and wait for 2 weeks after stopping the drug before starting to take a monoamine oxidase inhibitor. If you take the monoamine oxidase and the drug together or do not wait for 2 weeks, the person should create confusion, agitation, restlessness, stomach or intestinal symptoms, a gradual high body temperature, severely high blood pressure, or severe convulsions.
- The drugs should cause a serious condition called serotonin syndrome if taken together with some medicines. Do not use the drug with buspirone, fentanyl, lithium, tryptophan, or some pain or migraine medicines that involve rizatriptan, sumatriptan, or tramadol, Check with your doctor first before taking any other medicines with monoamine oxidase.
- For fewer people, these medicines should raise thoughts of suicide. Inform the doctor right away if start to feel more depressed and have thoughts about hurting yourself. Report any unusual thoughts or behaviors that disturb you, particularly if they are new or get worse quickly. Make sure the doctor knows if you have problems sleeping, get upset easily, have a big increase in energy, or start to act carelessly. Also tell the doctor if you have sudden or strong feelings, such as feeling nervous, angry, restless, forceful, or fearful. Allow the doctor to know if you or anyone in your family has bipolar disorder (manic-depressive) or has attempted to commit suicide.
- Do not stop taking the medicines without checking with the doctor. the doctor should want to slowly reduce the amount of the medicine used before stopping it completely. This may help prevent possible troubling of the condition and reduce the possibility of leaving symptoms like headache, nausea, or a general feeling of discomfort or illness.
- This medicine may cause a few people to become light-headed or fatigued. Make sure you should know how to react to this medicine before you drive, use medicines, or do anything else that could be dangerous if you are fatigued or not alert.
- Before having any type of surgery, tell the medical doctor that you are using this medicine. Taking the medicines together during surgery should increase the risk of side effects.
- These medicines should affect blood sugar levels. If you are diabetic and notice a change in the results of blood or urine sugar tests, check with the doctor.
- This medicine will add to the effects of alcohol and other central nervous system depressants medicines that cause sleepiness. CNS depressants are antihistamines or medicine for hay fever, allergies, or colds, sedatives, or sleeping medicine, prescription pain medicine or drugs, medicine for seizures or barbiturates, muscle relaxants, or anesthetics, including some dental anesthetics. This effect lasts for a few days after you stop taking medicine. Check with the doctor before taking any of the above effects while you are using the medicine. This involves prescription or nonprescription over-the-counter medicines and herbal or vitamin supplements.
Dental approaches for the bruxism
- If the patient and the patient’s child have bruxism, the doctor may suggest ways to preserve or improve the teeth. Although the dental approach methods may prevent or correct the wear to the teeth, should not stop the bruxism:
- Splints and mouth guards. These are designed to keep teeth separated from each other to prevent the damage caused by clenching and grinding. splints and mouth guards can be constructed of hard acrylic or soft materials and fit over your upper and lower teeth.
- Dental correction. In severe cases when tooth wear should be conducted to sensitivity or the inability to chew properly the dentist may need to reshape the chewing surfaces of the teeth or use crowns to repair the damage.
Other approaches for the treatment of the bruxism
- Stress or anxiety management. If the person grinds his/her teeth because of stress, the person should be able to prevent the problem by learning strategies that promote relaxation, such as meditation. If the bruxism is connected to anxiety, advice from a licensed therapist or counselor should help.
- Behavior change. Once the person discovers that he/she has bruxism, he/she should be able to change the behavior by practicing proper mouth and jaw position. Ask the dentist to show you the best position for your mouth and jaw.
Physical therapy for the bruxism
Biofeedback
- If the patient having a hard time changing her/his habits, they should get benefit from biofeedback, a method that uses monitoring procedures and equipment to teach you to control muscle activity in your jaw.
- Biofeedback is a technique that provides individuals with information about their bodily functions with the intention of promoting changes in behavior that result in improved health or performance. Electronically detected physiological measurements are coupled with a feedback signal that is inserted when pre-specified criteria are met and terminated only when the desired change in behavior occurs. Biofeedback aims to generate a learned response that continues even after the technique is discontinued. BioFeedback can be provided in a number of ways like visual information displayed to a patient or as visual information showing like a sensory stimulus.
- Bruxism biofeedback typically includes a contemporary stimulus produced in response to a detected grinding or clenching event. Detection may depend on mechanical sensors integrated into splints, Electromyography, or polysomnography analysis, with subsequent electronic analysis based on patterns of activity meeting pre-specified criteria. The paired feedback may be auditory, vibratory, electrical, or gustatory, and, in the case of sleep bruxism, the feedback can either be planned to be waking or non-waking. In wakeful patients, the stimulus is planned to develop an awareness of clenching and develop relaxation of the jaw muscles as well as allow reflection on the background or patterns of thought that may have given rise to the bruxism. The stimulus is not planned to be noxious but to be of sufficient magnitude to, at least initially, disturb conscious thought and alert the patient. For sleeping patients, stimuli may either be planned to disturb sleep or provide a non-waking stimulus that is processed in some way by the sleeping brain. the condition that can occur during sleep in humans suggests that biofeedback is not needed to wake a patient to be effective. Because biofeedback is planned to create a learned change in behavior, there is the possibility of long-term reduction or elimination of symptoms in addition to easing the condition by disturbing the bruxism during the period of active treatment.
- A related mode of management for sleep bruxism is contingent electrical stimulation, in which feedback is generated as an electrical stimulus applied to the skin, lip, or masticatory muscles. The possibility of local effects involving changes in biochemistry in stimulated tissues, in addition to higher cognitive responses, sets the contingent electrical stimulation apart from other forms of bruxism biofeedback.
The basic components of the biofeedback process
- the basic components of the biofeedback process should be understood from mid daugh’s conceptual framework
- in this framework, the therapist assesses the patient’s parameters in the instrument plans the strategies and gives the patient instruction about the strategies to be followed, as the patient tries the strategies the biofeedback system records the parameter and components in the physiological changes, and after processing displays the information before the patient is turned tries to perform movement strategies to alter the biofeedback signal, by altering the physiological changes thereby giving the therapeutic benefit
principles of biofeedback
- a behavioral positive reward model is generally employed with biofeedback
- simply when the patient generates the appropriate motor behavior, patients are positively reinforced
- the audio and visual feedback stimuli and other nonverbal information are usually much faster and more accurate rather than the therapist’s comments
- unlike other intervention of produces small changes in the motor behavior in the desired direction can be reinforced which should speed the rehabilitation process
- in behavior learning terminology, the therapist uses the biofeedback signals to shape the motor behavior by reinforcing the patients’ successive approximation to the goal behavior
- the therapist relates the controlling signals to the underlying motor behavior and re-establish the expected outcome
- reinforce already learned behavior, so the machine threshold should be monitored frequently
- feedback should be intrinsic or extrinsic, intrinsic feedback is the body’s internal feedback mechanism which uses a visual, auditory, vestibular, and proprioceptive mechanism
- extrinsic feedback is any kind of feedback is come from an external source that augments intrinsic feedback
limitations of the biofeedback
- relevancy: useful relevant information is important for the desired motor response, it should neither be short nor too long.EMG biofeedback can provide relevant information about the motor uni activity
- accuracy: the biofeedback device and the way it is used to provide accurate information they use specific devices that directly measure the force or range of motion of the joint for achieving accurate results, proper biofeedback device and technique of application should be used
- rapid information: all EMG processes delay electrical events during signal amplification and conversation to the audio speaker and visual meter due to inherent delays from the electrical circuits most commercial EMG biofeedback instruments give a 50 to 100 ms delay before the signals reach the ears and eyes of the patients
- biofeedback must provide immediate and rapid information, when biofeedback is employed the movements are essential to close the loop
Treating associated disorders with bruxism
- Medications. If the patient has developed bruxism as a side effect of a drug, the doctor may change the medication or prescribe a different one that is suitable.
- Medical conditions. If an underlying medical condition, such as gastroesophageal reflux disease is identified as the cause of the bruxism, treating the condition may improve bruxism.
Lifestyle and home-based exercise for the bruxism
- These self-care steps may prevent bruxism or help treat bruxism:
- Reduce stress. Listening to music, taking a warm bath, or exercising can help to relax and reduce the risk of developing bruxism.
- Avoid stimulating substances in the evening. Don’t drink caffeinated coffee or caffeinated tea after dinner and avoid alcohol during the evening, as this substance may worsen bruxism.
- Practice good sleep habits. Getting a good night’s sleep, which involves treatment for sleep problems, also helps to reduce bruxism.
- Talk to your sleep partner. If the person has a sleeping partner, ask him or/and her to be aware of any kind of grinding or clicking teeth sounds that the person should produce while sleeping so the person can report this to their dentist or doctor.
- Schedule regular dental exams. Dental exams are the best way to the identification of bruxism.
Try Splint Therapy
- Splint therapy is the first line of treatment of defense against teeth grinding. It includes wearing a custom-made dental night guard, bite guard, or occlusal splint. The night guard provides a physical boundary to protect the teeth and help to ease the symptoms like jaw pain and headache. the patient can either purchase a generic one from a drugstore or else, preferably, get one custom-made night guard from the dentist. They will take effect on your upper and lower teeth to create a mouthguard that fits into the jaw perfectly. Store-bought splints are not as durable or fitted.
Do Muscle Stretching Exercises
- Certain muscle stretching exercises help to decrease the discomfort related to tooth grinding and prevent its repetition. The exercises include
- Mindful Teeth Placement: Maintain a gap between the upper and lower teeth to avoid grinding or clenching. Try doing exercise all the time, except when chewing.
- Jaw Exercise: Open the mouth as broad as you comfortably can and try to touch your tongue to the front of your teeth. This exercise should help to relax your jaw muscles.
Warm Compress
- If you’re unconsciously clenching your teeth, a warm compress therapy can relax the muscles and increase blood circulation in the mouth area. Lie down and rest one side of your face either the right side or left side on a heating pad. Apply a warm compress therapy for 15 minutes and then repeat on the other side.
Meditation and Practice Yoga
- Mental health issues like stress, anxiety, and depression are all basic causes of bruxism. Stress reduction methods can help improve your overall health. To meditate, sit comfortably, and focus your mind for some time in a silent place. Don’t let your thoughts knock around the mind and try to empty your mind. You can also practice yoga with pelvic tilts, low lunges, and mountain poses which are the best poses to manage stress.
low lunges
- From Downward-Facing Dog (Adho Mukha Svanasana), expiration and step your right foot forward between your hands, aligning the right knee up the heel. Then lower the left knee to the floor and, keeping the right knee fixed, slide the left back until feeling a comfortable stretch in the left front thigh muscle and groin. Turn your left foot to the top of the floor.
- Inspiration and lift the torso upright. As you do, sweep the arms out to the sides and upward the arms perpendicular to the floor. Draw the tailbone down toward the floor and lift the pubic bone toward the navel. Lift the chest from the hardness of the shoulder blades against the back of the body.
- Take your head and back and looks up, careful not to touch the back of the neck. Reach the toe toward the ceiling. Hold for a minute, expiration the body back to the right thigh and your hands to the floor, and turn your back toes under. With another expiration, lift your left knee off the floor and step back to Adho Mukha Svanasana. Repeat with the left foot forward for the same period of time.
- Stand with your feet parallel, the bases of your big toes touching the floor, and your heels slightly apart from each other.
- Lift and spread the toes apart from each other and then release them back down on the mat.
- Without pushing the lower front ribs forward, lift the top of the sternum straight toward the ceiling. widen through the chest. permit the shoulder blades to draw toward each other and down your back, away from your ears.
- Let your arms relax equally with you, palms facing forward.
- Balance your head directly over your hips and look straight forward
Beginner Tips
- To find a better balance in Mountain Pose, place your feet hip distance apart from each other about where they naturally fall when walking forward. Keep your hips, knees, and feet facing the front of the room.
- support slightly back and front and side to side on your feet. Gently reduce the control and come to a stand position with your weight balanced smoothly beyond your feet. Root down through all edges of your feet. Feel that the energy drawn from your feet passes upward through your core muscle.
- Ask a therapist to stand beside you and confirm that your ears, shoulder joints, hips, and ankles are in a straight line.
- Lengthen through all sides of your neck and rest your look on a fixed point straight forward while in Tadasana.
- lengthen from your pelvis through the top of your head. You’ll notice where your body is drawn from stress or lack of movement,
yoga with pelvic tilt
- yoga with pelvic tilt involves some stages of the yoga
Yama
- Yama means moral or ethical discipline, the great principle rule controlling idea, age, time
- the principles are the rule of the mortality for the individual and society which is if not followed bring untruth, violence, disorder, distraction, collections
- the emotion of desired attachments is the main root that causing the trouble
- Yama only includes ignorance and pain, Patanjali tries to reduce these roots of the situation by modifying one’s ability to think along the 5 principles of the Yama
- ahimsa (nonviolence): not to give physical and mental pain to anybody
- Satya(truth): the simple meaning of Satya is reality
- Asatya (nonstealing): the person controls their need and reduces their wants
- brahmacharya(continence): the simple meaning of continence is to control sex life even as a householder living in the society, moral law and love should act as a guard against the demand
- aparigraha (noncoveting): the simple meaning of the noncoveting is not to collect.
niyama
- niyama are the rules of conduct that need which is applied to individual discipline(self-purification of the discipline )
- patanjali listed 5 niyama
- shaucha (purity): shaucha means cleanliness, it involves both physical cleanliness as well as cleanliness of the mind which is disturbing with emotions like passion, anger, greed, pride(mada), false belief
- good habits like bathing purify the body externally whereas asana, and pranayama clean it internally
- santosha: santosha is a state of satisfaction, the mind that is not satisfied cannot concentrate, differences arising from people because of race, wealth, and learning to distract them and they can’t become focused
- so the simple meaning of the santosha is the person feels the lack of nothing so he naturally feels satisfaction
- tap: tap involves self-discipline and strictness. to be efficient, tolerant, and champion over difficulties is the simplest meaning of the tap
- it is a conscious effort to achieve the ultimate goal with the separation and to lose all the wishes that act as a barrier in the way of this goal
- swadhyaya: it means self-education .it brings knowledge and put an end to ignorance to make life happy, healthy, and peaceful
- it is essential to study separate kinds of literature regularly, by self-education the person understands the nature of their soul better and gains communication with the religious
- ishwara pranidhana: it means surrendering all of one’s actions to the god
- when the priority of I and MINE disappears, the individual soul reaches full growth, person who knows that all creation belongs to god will not show the ego and be drunk with power
Asana (posture)
- asana is the third stage of yoga, a continuous and pleasant posture prevents instabilities of the mind and produces mental equilibrium unlike other systems of physical training which need large playfields and costly instruments
- asana should be done alone as the limbs of the body provide the essential weights and counterweights
- asana helps to maintain fine fitness which is strong and elastic without being muscle-bound and stiff
- asana keeps the body free from diseases, a soul without a body can be linked to a bird that loses its power to fly
- the person controls the body from diseases with the practice of the asana
- the names of the asana are significant and express the principle of evolution
- vegetations like padmasana
- insects like salabhasana
- aquatic animals like matsyasana
- birds like mayurasana
- quadriceps like ustrasana
- snake like bhujangasana
- human sperms like garbhapinda
dualities like body and mind, gain and loss, and mind and soul disappear with asana
Pranayama
- prana means breath it also suggests the soul is opposed to the body
- Ayama means the length of the expansion
- pranayama indicates the extension of the breath and a way to control
- control the overall function of breathing
- an inhalation termed Puraka (filling up)
- exhalation which is called a Rechaka (emptying the lungs)
- holding the breath in a state where no inhalation no exhalation which is termed Kumbhaka
- two ways of Kumbhaka first when the breathing is available after full inhalation but before exhalation begins known as antara kumbhaka
- second, when breathing is suspended after full exhalation but before inhalation begins known as Bahya kumbhaka
- in both types, breathing is suspended and restrained
- every living human unconsciously breathes prayer with each inward breath and exhalation
- the person fully realizes the importance of unconscious repetitive prayer
- prana in the body of an individual is part of cosmic breath
pratyahara
- pratyahara means gathering toward. the mind receives sensory impulses from the outside world and the body also forms extra sensory perception from the self
- in pratyahara, the outward senses are filtered out and turned into inward senses. the inward sense turns into eyes and ears
- one can experience optical and auditory extra-sensory perception
dharna
- when the mind is conscious and intelligence is confined to and concentrated upon a certain place in the body known as dharana
- the mind should be made to think of the one point in the heart or between two eyebrows on the forehead
dhyana
- when dharana continues for a long time it becomes Dhyana meditation .in dhyana there is no movement in the body
- meditation is a subjective experience and can’t be taught
- it is an incredible state that has to be experienced, it releases all the tension, in meditation the flow of energy is continuous and stable
Samadhi
- the merging of the individual’s consciousness with the object of the meditation is a total consummation called samadhi,
- when the uninterrupted flow of the individual’s awareness gets absorbed in the object of meditation their consciousness loses its identity and becomes one with the object
Eat Magnesium-Rich Food
- Magnesium benefits relaxation and regulates mood. Include magnesium-rich foods such as dry roasted almonds, boiled spinach, bananas, fish, black-eyed peas, peanut butter, and flaxseed in the diet. These items will help relax muscle tissues and blood vessels and inhibit grinding caused by tight or spasming jaw muscles. You can also take magnesium supplements, but it’s necessary to consult a doctor or nutritionist first before taking them.
Drink Turmeric Milk
- Turmeric has anti-inflammatory properties that benefit in relieving the aching jaw muscles. And add the amino acid tryptophan to milk helps the nervous system makes relax and developed sound sleep. If you don’t like the taste of turmeric milk, add some kind of honey for sweetness and drink a glass of turmeric milk with added honey daily before bedtime for the correct results.
Drink Herbal Tea
- Instead of caffeinated beverages like coffee, better off consuming non-caffeinated alternatives. preferring herbal or chamomile tea is a great way to naturally reduce stress and ease the symptoms of grinding in sleep as it’s elevated by nervous tension. Herbal tea relaxes the body and mind and keeps you fit and cool. Try a cup of warm green tea before bed to reduce the possibility of grinding or clenching the teeth while sleeping
What you can do if suspected of bruxism?
- take an appointment with the doctor by making a list of proper medical history, particularly, past bruxism-related problems and information on any medical conditions.
- Any symptoms that are experienced, involving any that may tend to be unrelated to the reason for the appointment. If you experience pain, make a note of when it occurs, like when you wake up or at the end of the day.
- make a keynote of personal information, including any major stresses or recent life changes.
- All medications, including beyond-the-counter medications, vitamins, herbs, or other supplements, are taken by the person, and the dosages of that medications. Let the doctor know about anything that a person has taken to help him/her sleep.
- Most people possibly grind and clench their teeth from time to time. Occasional teeth grinding, medically called bruxism, does not generally create harm, but when teeth grinding occurs on a regular basis the teeth can be damaged and other oral health complications can awake
How should I Find Out if the Teeth are grinding?
- grinding generally happens during sleep, most people are not aware that they grind their teeth. However, a dull, constant headache or soreness in the jaw when you wake up is a disclosing symptom of bruxism. Many times people learn that they grind their teeth from their loved one who likes to hear the grinding at night.
- If you suspect that grinding the teeth, talk to your dentist. Dentists can examine the mouth and the jaw for signs of bruxism, such as jaw tenderness and excessive wear on your teeth.
Why the Teeth Grinding is Harmful?
- chronic teeth grinding can outcome in a fracturing, loosening, or loss of teeth. The chronic grinding may wear teeth down too. When chronic teeth-grinding events happen, bridges, crowns, root canals, implants, partial dentures, and even complete dentures surgeries should be needed.
- Not only can severe grinding damage teeth and result in tooth loss, but it can also affect the jaws, cause or worsen temporomandibular joint/temporomandibular dysfunction, and even change the appearance of your face.
- the dentist should fit a mouth guard to protect the teeth from grinding during sleep.
- Till if you think you may be grinding your teeth after the application of the mouth guard, see your dentist. They should examine the temporomandibular joint, jaw muscles, and teeth for signs of bruxism.
- ask your healthcare provider for reducing stress
- Cognitive behavioral therapy (CBT) is a short-term therapy technique that can help people for finding new ways to behave by changing their thought patterns. Sessions focus on analyzing new ways to approach everyday challenges.
- cognitive behavior therapy sessions focus on exploring and developing methods to deal with challenges and behavior patterns that arise from day to day. Cognitive behavior therapy is one type of therapy that can be much more effective in treating depression, anxiety, bipolar disorder, and various other mental health conditions.
- cognitive behavior therapy generally contains 5 to 21 sessions in one session, though some people might have more sessions. Cognitive behavior therapy should also take the form of group sessions.
Cognitive behavior therapy for bruxism
- Cognitive behavior therapy is a form of psychotherapy that generally concentrate on how thoughts, mindset, and attitudes affect feelings and behaviors.
- Unuseful ways of thinking and behavior can lead to psychological distress.
- People can learn more beneficial ways of thinking and behave in Cognitive behavior therapy.
- New habits can relieve symptoms of mental and physical conditions and permit people to act in more beneficial ways.
- Cognitive behavior therapy is support people with depression, panic disorder, and various other health conditions. There is also growing evidence to help relieve chronic pain.
- A course of Cognitive behavior therapy contains a series of sessions in which a counselor and an individual or group meet regularly and participate in the session. Counselors typically hold the meetings weekly.
- Cognitive behavior therapy concentrates on present thoughts and mindset and points out the need to identify, challenge, and change how a person views a situation.
- Changing distortions and perceptions
- Cognitive behavior therapy’s goal is to transform the ways of thinking and behaving that stand in the way that how a person should like to live their life. Cognitive behavior therapy involves analyzing negative perceptions or distortions that are affecting behavior.
- A twisted view can make a person more susceptible to:
- an unhelpful mindset
- direct jumping to conclusions
- falsely seeing situations
- see things as either good or bad, with nothing available in between
- If people learn fearful or unuseful ways of thinking, they can start to think in this way automatically. Cognitive behavior therapy concentrates on challenging these automatic thoughts and comparing those thoughts with reality.
- When a person comes to view a particular situation in a more helpful way, their distress generally reduces, and the person should take actions or make decisions that are more likely to serve the situation in the long term.
What can Cognitive behavior therapy do?
- During a course of Cognitive behavior therapy, a person can learn to:
- develop a way of awareness of automatic, unuseful thoughts
- challenge underlying acceptance that may be unuseful
- determine between facts and unhelpful thoughts
- develop a more useful way of thinking and seeing situations
- The activities involved the exact course of a person with Cognitive behavior therapy alters, depending on their symptoms and circumstances. During a typical course, a person has regular one or more group sessions, or a combination of both gets frequent feedback
- does role-playing activities
- learns new ways to calm the mind and body
- gradually increased exposure to the things which they are fear in the past
- does homework assignments
- keeps a cognitive behavioral diary
- practices skills to develop positive behavioral change and growth
- exercise
- physical therapy
- medication
Do Children Grind Their Teeth?
- The problem of teeth grinding is not limited to only elders. Approximately 15 percent to 33 percent of children also grind their teeth. Children who grind their teeth tend to do so at two peak times when their baby emerges their teeth and when their permanent teeth come in. Most children lose the teeth-grinding habit after these two sets of teeth should come in more fully.
- in general, most children grind their teeth during sleeping hours rather than during waking hours. the considerations include improper alignment of the teeth or irregular contact between upper and lower teeth, illnesses, and other medical conditions like nutritional deficiencies, pinworm, allergies, an endocrine disorder, and psychological factors involving anxiety and stress.
- Grinding of the baby’s teeth rarely results in problems.
Specific tips to help a child stop grinding the teeth include
- reducing a child’s stress, especially just before bed.
- Try to do massage and stretching exercises to relax the muscles in the child.
- Make sure about the child’s diet involves plenty of water. Dehydration is related to teeth grinding.
- Ask your dentist to monitor the child’s teeth.
- If stress leads you to grind your teeth, ask your doctor about options to reduce your stress. Attending stress counseling seminars, starting an exercise program, seeing a physical therapist, or obtaining a prescription for muscle relaxants medication are some of the options that may be offered.
- While stress is a main cause of bruxism in adults, that’s not generally happening in the case with children. Teeth grinding in children may arise from Allergies, misalignment of the teeth, Mouth irritation, Obstructive sleep apnea, and Heredity.
- If a sleeping disorder is causing the grinding, treating it with exercise should reduce or eliminate the grinding habit.
Other tips for stopping teeth grinding involve:
- Avoid cutting back on foods and drinks that contain caffeine, like colas, chocolate, and coffee.
- Avoid alcohol. Grinding leads to an increase in alcohol consumption.
- Do not chew pencils or pens or anything that is not food. Avoid chewing bubblegum as it grants the jaw muscles to get more habit to do clenching and makes you more grind the teeth.
- Train yourself to not clench and grind your teeth. If you notice that you clench or grind during the day, position the tip of the tongue in the middle of the teeth. This position’s daily practice trains your jaw muscles to relax.
- Relax the jaw muscles at night by grasping a warm washcloth as opposed to the cheek in front of the earlobe.
- breathing exercises, listening to music and taking exercise
Diaphragmatic Breathing
- Patient Instructions: Position the patient with one hand on the stomach and the other hand on the chest. Feel your stomach elevate and fall downward with each individual breath. Continue for 1 minute.
- When you do breathe in: the stomach pushes outward. The hand on the chest should remain and maintain its position.
- When you breathe out or exhale: Tighten the stomach muscles and feel the stomach pull inward. The hand on the chest should remain in its position.
- Breathe in, feeling your stomach push out. As you breathe out or/and exhale, say the following sounds and words, remaining aware of the stomach slightly pulling in.
- Start breathing exercises with easy sounds like “sss” and “shh”
- normally work up to sounds like “ahh” and “ooh”
- do tasks up to single words like “hello” and your first name etc
- generally work up toward longer words, phrases, and sentences
Pursed lip breathing
- Improves ventilation
- Releases trapped air in the lungs
- manage the airways open for a prolonged time and reduce the work of breathing
- continuously exhalation to slow down the breathing rate
- recover breathing patterns by moving old air out of the lungs and granting new air to enter the lungs
- Relieves shortness of breath
- Create general relaxation
Pursed lip breathing technique
- Relax your neck and shoulder muscles.
- Breathe in or/and inhale simply slow over your nose for 2 counts, keeping your mouth closed. Do not take a to many long breaths inhale; a normal breath pattern will do. breathe in which may help to count to yourselves for inhale
- Pucker your lips as if you are trying to use a whistle or gently flicker the flame of a candle.
- Breathe out slowly and slightly with pursed lips while counting to 4. Breathing out helps to count to yourselves for exhale, one, two, three, four.
Pursed lip breathing reminders
- Do not force the air out.
- Always breathe out and exhale for too much longer than you breathe in and inhale.
- Breathe slightly slow, and relaxed manner and breathe out till you are in complete control.
Glossopharyngeal breathing
- glossopharyngeal breathing is an elevating the patient’s inspiratory capacity when there is severe weakness in the inspirator’s muscle
- it is taught to that patient who have difficulty in taking deep breathing and who can develop respiratory muscle problems due to weakness of respiratory muscles
- the patient takes in several swallows of air then the mouth is closed and the tongue gives force to the air back and catches in the pharynx, then the air is forced to pushes air back into the lungs organ while the glottis is opened
- glossopharyngeal elevates the depth of the inhalation and the patient’s vital capacity
- try to improve your sleep pattern by going to bed at the same time every night and relaxing before bedtime, and making sure your bedroom is dark and quiet
- take painkillers like paracetamol or ibuprofen if you have jaw pain or swelling in the jaw
- use an ice pack wrapped in a towel for 20 to 30 minutes to help reduce jaw pain or swelling
The best way to take care of the jaw and teeth
- You may find that certain sleeping positions like prone, supine, and side-lying cause you to grind your teeth more. You may be able to reduce bruxism by avoiding those positions.
- Also, look for ways to manage stress. stress management should greatly relieve the teeth grinding. In addition, to talk therapy, you should try at home how to relieve stress, including a warm bath before bed and listening to peaceful music.
- Tongue and jaw muscle exercises should help you to relax the jaw and facial muscles and maintain proper alignment of the jaw. You can try the exercises at home or work with a physical therapist.
Try the following exercises
- Open your mouth broad while touching your tongue to the front of the teeth. This helps relax the jaw.
- Say the letter “N” loudly. This will keep your upper and lower teeth from touching that and help you to avoid clenching.
Goldfish Exercise
- The goldfish exercise helps you align the jawbone while you are chewing.
- Step 1: Press the tongue to the roof of the mouth.
- Step 2: Now place one index finger on the left temporomandibular joint and another index finger on your chin.
- Step 3: Drop your chin backward, applying light pressure with each finger and keeping the tongue to the roof of the mouth. Repeat the goldfish exercise for the right temporomandibular joint.
- Try the goldfish exercise a total of six times daily
Mandibular Stabilization Exercise

- mandibular stabilization exercises similarly try to align the jawbone and improve its range of motion beyond time.
- Step 1: Start with the jaw in a neutral and relaxed position.
- Step 2: Hold the thumb to the base of the jaw, just under the chin, and apply slight pressure to open the mouth.
- Step 3: Repeat the movement, moving the thumb to the left side and right sides of the jaw respectively.
- Try mandibular stabilization exercises at least five times daily
Cervical Retraction “Chin Tucks”
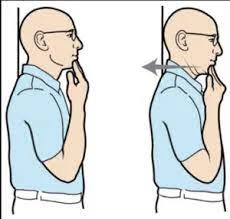
- The goal of the Chin Tucks exercise is to strengthen the cervical muscles and improve the alignment of the head and spine.
- Step 1: Start from a standing position with your shoulders turn backward and your chest lifted up.
- Step 2: carry out your head straight backward, tuck with your chin
- Step 3: Keep your head straight throughout this movement.
- Hold this movement for three seconds at a time and repeat it up to 10 times.
Side-to-Side Jaw Exercise

- For side-to-side jaw exercise, need a small object, like a flat wooden stick. the flat wooden stick will work to target the jaw’s range of motion.
- Step 1: Place a clean wooden stick, like a craft stick, in the mouth, holding it softly between the upper and lower teeth.
- Step 2: Now start shifting your jaw from side to side without loosening the hold on the stick.
- Step 3: Shift your lower jaw forward and backward, still keeping the teeth clenched.
- Try side-to-side jaw exercise at least once a day and use a thicker stick if it gets too easy for you.
Tongue Up Exercise

- Tongue up is an easy exercise that targets the jaw muscles and also helps improve the range of motion.
- Step 1: Start with a seating or standing position, slightly touching your tongue to the roof of your mouth.
- Step 2: Now, without allowing your tongue to drop down, extend the jaw as far down as you can.
- Step 3: without moving the tongue, close your jaw and then open the jaw again.
- Repeat this chewing movement at least 10 times, three times a day.
Risk factors for the bruxism
- Men and women get bruxism at approximately the same rate. If you have a family history of teeth grinding, you should face a higher risk of bruxism. Other risk factors include:
- Personality type, like people who are very driven, may be more prone to teeth grinding.
- Stress
- anxiety
- depression
- Cigarette smoking and caffeine use.
- Certain anti-anxiety medications.
What else should I ask my physician about the bruxism?
- If you have bruxism, ask your physician:
- should I need a night guard?
- should I need dental treatment to fix teeth problems?
- What other treatments should help stop teeth grinding?
- Will I need a sleep study to detect bruxism?
- What medications should help?
- Will there any long-term effects from teeth grind?
FAQS
What’s the outlook for people with bruxism?
The outlook for people with bruxism is good. Children generally develop teeth grinding followed by adolescence. For adults, follow your doctor’s suggestion. if you have a night guard for teeth grinding as per the doctor’s prescription, wear it regularly. Following the treatment plan helps improve the symptoms, so you feel your best.
Is bruxism a sleep disorder?
sleep bruxism is a type of sleep disturbance that occurs in the central nervous system.
Why Do People Grind Their Teeth?
Although teeth grinding can be caused by stress and anxiety, it generally happens during sleep and is more likely caused by an abnormal bite or missing or crooked teeth. teeth grinding can also be caused by a sleep disorder like sleep apnea.
How common is bruxism?
Bruxism is a common sleep disorder. It affects about 10 percent of adults and up to 15 percent of children
which medicines are best for bruxism?
Muscle relaxants like diazepam, and cyclobenzaprine has taken before bedtime, for a short period of time.
Injections of Botox, a form of botulinum toxin, should help some people with severe bruxism who shouldn’t respond to other treatments.
Medication for anxiety or stress: the doctor may recommend the short-term use of antidepressants like citalopram, and escitalopram, which are classes from selective serotonin reuptake inhibitors (SSRIs). or anti-anxiety medications like desvenlafaxine, duloxetine, and venlafaxine which are class of serotonin and norepinephrine reuptake inhibitors ( SNRIs) to help you deal with stress or other emotional issues that may be causing the bruxism.
tricyclic antidepressant medication which includes Anafranil, Norpramin, doxepin, etc . helps to reduce depression
what is the role of biofeedback in bruxism?
The biofeedback method uses the approach that bruxers can unlearn their undesired behaviors when a stimulus makes them aware of their adverse muscle activities. Biofeedback has been applied for bruxism during awake bruxism as well as for sleep bruxism.
Is cognitive behavioral therapy good for bruxism?
Cognitive behavioral therapy is helpful to treat bruxism and other psychological problems, including stress and anxiety. These issues occur behind the teeth grinding. Cognitive behavior therapy helps you to change your way of thinking or acting so that you can easily manage your problem.
Can bruxism affect breathing?
Bruxism is an oral para-functional activity of the teeth grinding and/or jaw clenching. As muscles of the body relax during sleep, the closed tongue, resting low in the mouth, can fall backward and obstruct the airway, causing difficulty in breathing.
why breathing exercises are useful in case of bruxism?
diaphragmatic breathing can strengthen and extend your airway muscles to reduce bruxism. and pursed lip breathing is help to reduce anxiety





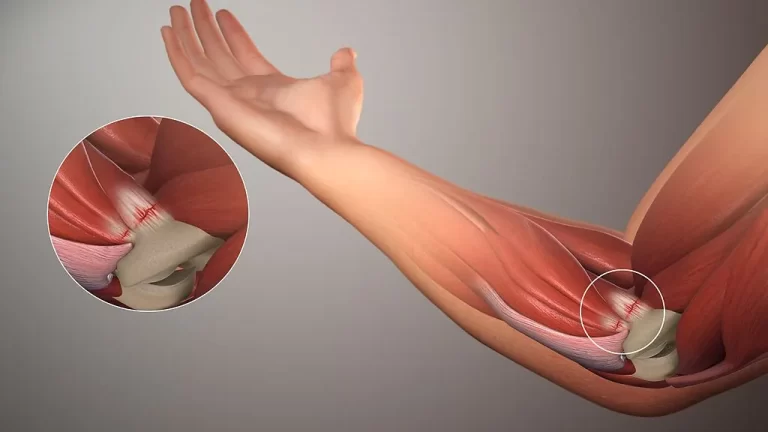
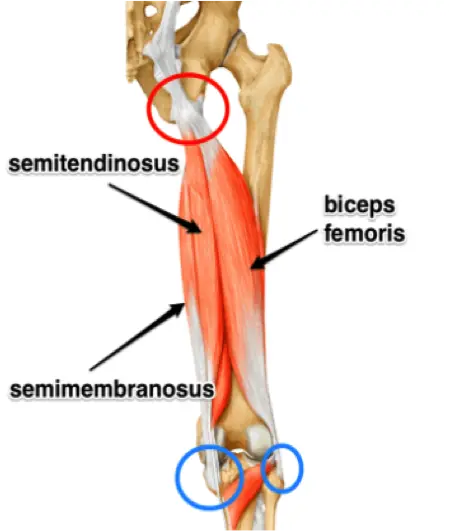
2 Comments