Brachialis Syndrome: Causes, Symptoms, and Treatment
Introduction
Brachialis syndrome is a rare condition that causes compression of the median nerve at the level of the lacertus fibrosus, a thick fascia that covers the brachialis muscle. This compression results from swelling of the brachialis muscle, which can be caused by prolonged elbow extension.
The symptoms of brachialis syndrome include pain, numbness, and weakness in the hand and forearm. In some cases, the symptoms can be severe and permanent.
Anterior interosseous nerve (AIN) compression or injury can result in brachialis syndrome, often referred to as anterior interosseous nerve syndrome. This is an uncommon disorder. The brachial plexus in the neck is the starting point of the median nerve, which branches off into the AIN and goes down the arm and into the forearm. The pronator quadratus, flexor pollicis longus, and flexor digitorum profundus (index and middle fingers) are among the deep flexor muscles of the forearm that are supplied by the AIN.
Brachialis syndrome induces sudden, severe pain in your shoulder and upper arm observed by muscle weakness. Each person is affected differently, and it can last for a few days, weeks, or months. Healthcare providers can offer many treatment choices to assist in treating pain and muscle weakness. This mainly affected the median nerve in the brachial plexus.
The median nerve and musculocutaneous nerve constriction at the elbow have been reported to arise from the lacertus fibrosus in numerous reports and studies. However, we could find information on a median neuropathy at the elbow associated with patient positioning, which we have termed brachialis syndrome. This is mainly characterized by nerve passing through the brachialis muscle, so injury to this muscle and the nearest part can lead to brachialis syndrome.
As the median nerve leaves the brachial plexus in the upper arm and stretches past the elbow, it lays in an external position just behind the bicipital tendon aponeurosis and anterior to the brachioradialis muscle. The medial nerve then departs between the ulnar and humeral heads (upper arm bone) and the larger bone of the forearm. It then crosses the pronator teres muscles.
What is Brachialis Syndrome?
Brachialis syndrome is a neurological disorder that induces sudden and severe pain in your shoulder and upper arm. A few days to a few weeks may pass as the pain persists. Muscle deficiency in your shoulder, arm, forearm, or hand then causes the pain. The defect can last for several months.
The brachialis muscle can be mainly affected by repetitious forceful contractions or muscular contractions with the arm in hyperextension. This is typically seen in climbers, due to the pronation of the hand and the extended initiated position. Physical exercise that involves a lot of pull-ups, curls, and rope climbing can also start brachialis muscle pain. A strain to the brachialis tendon can also induce a patient to offer a lacking elbow extension due to painful end-range stretching of the tendon.
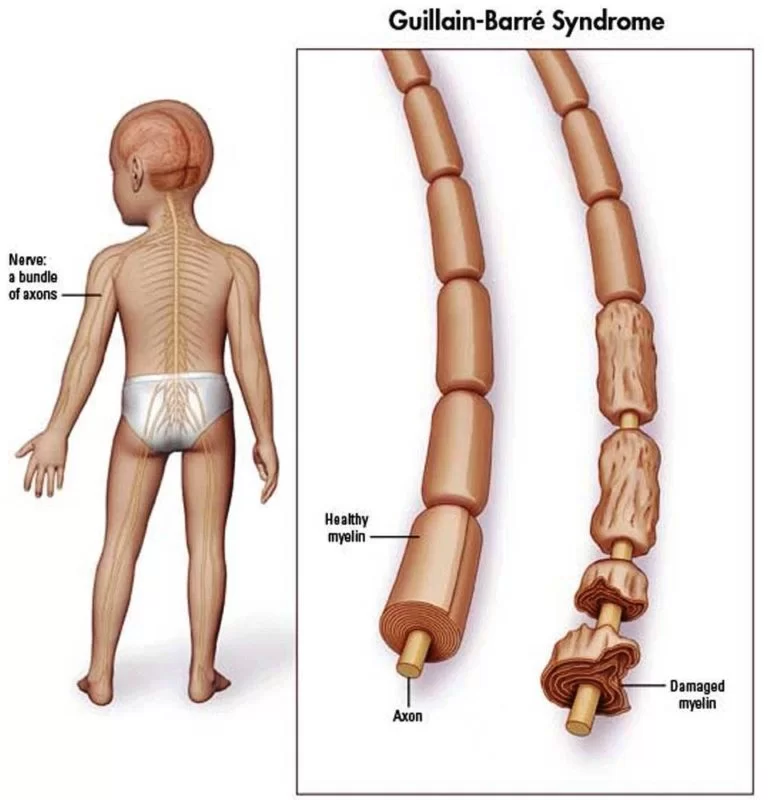
Due to the area of the pain, medial epicondylitis and lateral epicondylitis should also be evaluated. The syndrome occurs due to harm to your brachial plexus and its supply. It is a network of nerves that extends down your arms and into both of your armpits after leaving your spine and passing through your neck. This syndrome mainly affects motor nerves and axons. These nerves are liable for controlling movement. This is why it shows muscle weakness.
This is rarely observed that why healthcare providers usually misdiagnose it as cervical radiculopathy (pinched nerve) or cervical spondylosis. These are much more typical conditions that have similar symptoms.
- Brachial neuritis.
- Brachial plexus neuritis.
- Brachial plexus neuropathy.
- Idiopathic brachial plexus neuropathy.
- Neuralgic amyotrophy.
Phases of brachialis syndrome :
There are usually three phases of this syndrome:
- Phase 1 (acute pain phase): This affects severe and sudden pain that usually involves one shoulder. The pain and this stage may persist for several days or weeks. In general, the extended this phase lasts, the longer it takes to recover.
- Phase 2: After the pain decreases, you begin to produce muscle weakness, such as arm and shoulder girdle weakness. This can lead to muscle loss (atrophy). Phase 2 can extend beyond the usual duration of six to eighteen months.
- Phase 3: Your muscles eventually restore their power and functionality.
How common is Brachialis Syndrome?
Brachialis syndrome is irregular. Up to three people per 100,000 get per year. Anyone at any age can get the syndrome. However, men who were assigned male at birth (AMAB) are more commonly involved than women who were declared female at birth (AFAB). The average age of beginning is 41 years.
Symptoms
Sudden pain and following muscle deficiency are the main symptoms of brachialis syndrome. They can impact you:
- Shoulder.
- Upper arm.
- Forearm.
- Hand.
- Hurt in the front of your elbow
- Swelling in the anterior side of the elbow
- Problem extending your elbow.
- Pain and numbness in the forearm
- Weakness in the grip
- Difficulty flexing the index and middle fingers
- Weakness when flexing your elbow, particularly when your forearm is in the pronated position
In about 80% of cases, it only involves one arm (unilateral) most usually your dominant arm/hand. In about 25% of cases, it involves both arms (bilateral). Rarely, it can even impact your lower trunk and lower extremities.
In most cases, the pain hits all of an impulsive. It is sharp and intense and is usually worse at night. Severe discomfort may persist for several hours or even for a week. After the pain moves away, the muscles in your involved arm will begin to get weak.
You will likely experience muscle weakness in your shoulder or upper arm, although it can also impact your forearm and hand. Sometimes, weakness can impact your chest or diaphragm. You gradually lose muscle mass (muscle atrophy) when your muscles are weak.
Because of the usual nerves, the severity of the symptoms might differ greatly from person to person.
- Issues with your reflexes in your involved arm.
- Abnormal sensations (paresthesia) or numbness in your involved arm. This could have a burning, prickling, or tickling sensation.
- Partial shoulder and elbow dislocation.
- Abnormal range of movement in your involved joints.
- Winged scapula: the protrusion of the shoulder blade.
- Shortening of the muscles or tendons in your involved arm.
- Red, purple, or stained hands (due to insufficient circulation).
- Swelling in your hands.
- Shortness of breath (dyspnea). This is irregular.
Causes of Brachialis Syndrome
the exact cause of this syndrome. They believe that the primary cause is an atypical immune system response or immunological-mediated response. They have two approaches:
- Viral, bacterial, or parasitic infections instantly affect your brachial plexus, generating the symptoms.
- Your immune system strikes the bacteria, virus, or antigen and harms your brachial plexus in the process.
Having a current viral infection is the most typical trigger of PTS. The subsequent viral illnesses are most typically involved:
- Coxsackie B virus can generate several conditions, like pneumonia, gastrointestinal illness, myocarditis, aseptic meningitis, encephalitis, and viral hepatitis.
- HIV (human immunodeficiency virus).
- Fifth disease (parvovirus B19).
- Mumps.
- Smallpox (variola major and minor).
In some cases, healthcare providers can not select a triggering occasion. In occasional cases, this syndrome occurs due to a genetic (inherited) condition named hereditary neuralgic amyotrophy.
What are the risk factors for developing Brachialis Syndrome?
Investigators think that specific conditions and situations may make you more vulnerable to creating brachialis syndrome. These include:
- Current surgery and/or anesthesia.
- Connective tissue diseases, like Ehlers-Danlos syndrome.
- autoimmune diseases such as polyarteritis nodosa, temporal arteritis, and lupus (systemic lupus erythematosus).
- Traumatic shoulder damage.
- Strenuous activity involving your shoulder and elbow.
- Vaccines (immunizations).
- Pregnancy and childbirth.
- Radiation therapy.
- Receiving contrast dye for an imaging test.
Diagnosis and Tests
Your physician will ask about your symptoms and medical record and do a physical exam. They will test for muscle strength, reflexes, and feeling in your arm. They might suggest visiting a neurologist.
If your doctor thinks you have brachialis syndrome, they may suggest a test called an EMG (electromyography). It assesses the health and process of your skeletal muscles and the nerves that regulate them.
You might also have the following imaging tests to establish the diagnosis or rule out other conditions:
- MRI (magnetic resonance imaging) scan.
- Nerve ultrasound.
- CT (computed tomography) scan.
Management and Treatment
There is no specific treatment or therapy for this syndrome it usually goes away on its own. However early diagnosis and supporting therapies can help enhance your outlook (prognosis).
Your healthcare provider will suggest certain therapies for controlling your symptoms. A group of experts may be working with you to create a care plan.
- Primary care physicians (PCPs).
- Orthopaedists.
- Neurologists.
- Neuromuscular disease specialists.
- Physical therapists.
Treatments for the acute pain phase may include:
- Analgesics (pain medicine, like over-the-counter NSAIDs).
- Oral corticosteroids.
- Using a shoulder stabilizer or minimizing the usage of your arm will immobilize it.
- Transcutaneous electrical nerve stimulation (TENS).
- Acupuncture.
Your healthcare professional will probably suggest the following treatments when the acute period has passed:
- Physical therapy: A physical therapist can guide you in stretching and strengthening activities to help your muscles and joints recover.
- Co-analgesics: These are drugs that specifically treat nerve pain. Examples include gabapentin, carbamazepine and amitriptyline.
In severe cases, your provider may suggest surgery if nothing else has helped your symptoms. Tendon transfers and nerve grafting are examples of surgical procedures.
Types of surgical procedures include:
- Nerve repair: Your surgeon attaches the two torn edges of a severed nerve during this treatment. When you have a knife wound or other sharp lacerations to your nerves, surgeons usually take care of you right away.
- Nerve graft: Your surgeon attaches the two torn edges of a severed nerve during this treatment. When you have a knife wound or other sharp lacerations to your nerves, surgeons usually take care of you right away.
- Nerve transfer: When there are no viable nerve stumps in your neck that can be linked to nerve grafts, surgeons will undertake this treatment. To send a signal to a paralyzed muscle, the surgeon in this technique slices and reattaches a healthy donor nerve to the damaged nerve.
How to Prevent Brachialis Syndrome?
As researchers do not know the exact reason for brachialis syndrome there is nothing you can do to prevent it. Certain viruses may initiate brachialis syndrome, so staying as healthy as possible may help in lowering your chance of getting it.
Prognosis
The prognosis can change at any time. Some individuals only participate in one episode of brachialis syndrome and fully recover their strength in the impacted areas. Other people have persisting weakness and pain. Some people develop brachialis syndrome more than once (repeat).
Some factors that may improve your risk of a proper prognosis include:
- Females.
- Persistent pain and lack of muscle healing by three months.
- If brachialis syndrome affects your lower trunk/abdomen.
- If the reason is hereditary. These issues have much more common recurrence rates.
According to a study, 89% of people with brachialis who received symptom management and physical therapy recovered within three years. About 36% of those individuals recovered in the first year, and about 75% did so in two years.
According to recent research, a large number of patients still experience pain and other functional problems. However, a complete return to strength is feasible and may require up to eight years.
FAQ
What is the best treatment for brachialis syndrome?
Casts and Splints. Our physicians may suggest using a series of custom casts to treat the brachial plexus injury and enhance the range of movement and joint alignment by slowly stretching the joint. During this procedure, a new cast is used weekly for up to 6 weeks to the affected area.
Which muscles are involved in brachialis syndrome?
Severe upper-trunk damage may paralyze the shoulder muscles (deltoid muscle and rotator cuff), as well as the muscle in the upper arm brachialis, and biceps. When a fall forces the shoulder down and the head to the opposing side, upper-trunk palsy can result.
Which are the two types of brachial plexus injuries?
Constriction neuropraxia is the most typical form and commonly occurs in older people. When a nerve is pulled, usually downward, traction neuropraxia occurs. This damage is less common than compression neuropraxia but is more common among adolescents and young adults.
What are the symptoms of brachial pain?
Symptoms of brachial pain include Severe pain in the upper arm or shoulder. Pain usually involves just one side of the upper body. After a few hours or days, the pain transfers into weakness, limpness, or paralysis in the muscles of the involved arm or shoulder.
Which test is done for brachialis syndrome?
To help diagnose the extent and severity of a brachialis syndrome. you may have one or more additional of the following examinations: X-ray. An X-ray of the shoulder and neck can tell the provider if you have fractures or other associated damages. Electromyography (EMG)
How do you manage nerve damage in the upper limb?
Restoring function
Braces or splints. These appliances keep the involved limb, fingers, hand, or foot in the right position to enhance muscle function.
Electrical stimulator. Stimulators can activate muscle performed by an injured nerve while the nerve regrows.
Physical therapy.
Exercise.
References
- Beacon Health System. (2022, June 3). Brachial plexus injury. https://www.beaconhealthsystem.org/library/diseases-and-conditions/brachial-plexus-injury?content_id=CON-20127291
- Normandin, B. (2017, May 3). Brachial plexus neuropathy. Healthline. https://www.healthline.com/health/brachial-plexopathy
- UpToDate. (n.d.). UpToDate. https://www.uptodate.com/contents/brachial-plexus-syndromes
- Ewumi, O. (2022, June 29). What to know about brachial plexus injuries. https://www.medicalnewstoday.com/articles/brachial-plexus
- Koehler, S. M., Meier, K. M., Lovy, A. J., Fitzpatrick, D., Kim, J., & Hausman, M. R. (2016). Brachialis syndrome: a rare consequence of patient positioning causing postoperative median neuropathy. Journal of Shoulder and Elbow Surgery, 25(5), 797–801. https://doi.org/10.1016/j.jse.2015.12.023
- Lox. (2019, July 31). Median Neuropathy – Dennis M. Lox, M.D. – Regenerative Medicine. Dr. Dennis Lox Stem Cell Therapy. https://www.drlox.com/elbow/median-neuropathy/
- Koehler, S. M., Meier, K. M., Lovy, A. J., Fitzpatrick, D., Kim, J., & Hausman, M. R. (2016b). Brachialis syndrome: a rare consequence of patient positioning causing postoperative median neuropathy. Journal of Shoulder and Elbow Surgery, 25(5), 797–801. https://doi.org/10.1016/j.jse.2015.12.023
- Brachialis. (n.d.). Physiopedia. https://www.physio-pedia.com/Brachialis





2 Comments