Hypertension (High Blood Pressure)
Introduction
Abnormally high blood pressure is called hypertension. When the body’s smallest blood vessels, known as arterioles, narrow, the blood presses too hard against the artery walls, resulting in hypertension and making the heart work harder to keep the pressure constant.
For months or even years, the heart and blood vessels can tolerate elevated blood pressure. Still, eventually, the heart may grow (a condition known as hypertrophy) and weaken until it fails. There is also a chance of blood vessel damage to the eyes, brain, and kidneys.
The systolic and diastolic pressures are measured together to figure out blood pressure. The force that blood applies to the arterial walls as the heart contracts to pump blood to the peripheral organs and tissues is known as the systolic pressure, which is also the first value recorded and the higher pressure.
The residual pressure that the heart applies to the arteries as it relaxes in between beats is known as the diastolic pressure, which is the lower pressure and the second number reported. When blood pressure hits or is above 140/90 mmHg, or “140 over 90 millimeters of mercury,” hypertension is diagnosed.
Causes of Hypertension
Many different factors might affect blood pressure, such as:
- How much salt and water your body carries
- The condition of your blood vessels, nervous system, or kidneys
- Your hormone levels
As you age, the likelihood of hearing that your blood pressure is excessively high increases. This is because as you age, your blood vessels stiffen. Your blood pressure rises as a result. Your risk of heart disease, stroke, heart attack, heart failure, kidney disease, and early mortality is increased by high blood pressure.
High blood pressure is more likely to develop if you:
- Are Overweight
- are frequently anxious or worried
- Consume excessive amounts of alcohol (more than one drink for women and more than two for males each day).
- Eat excessive amounts of salt
- have a family history of hypertension
- have diabetes
- Use or smoke tobacco
Most of the time, there is no known cause of elevated blood pressure. We refer to this as essential hypertension.
Secondary hypertension is high blood pressure brought on by another health condition or medication you are taking. A possible cause of secondary hypertension is:
- prolonged kidney disease
- diseases of the adrenal glands, such as Cushing syndrome and pheochromocytoma
- Hyperparathyroidism
- Preeclampsia or pregnancy
Epidemiology
Over one billion adults globally suffer from hypertension, accounting for as much as 45% of the adult population with the condition. All socioeconomic and income levels have a significant prevalence of hypertension, which increases with age and can affect up to 60% of the population over the age of 60.
Based on patient data from 67 countries, the 2010 global health survey study published in Lancet identified hypertension as the top cause of mortality and disability-adjusted life years globally since 1990.
According to recent predictions, the number of people with hypertension may rise by 15% to 20% by 2025, almost reaching 1.5 billion.
Symptoms
The majority of people with hypertension experience no symptoms. In addition to other symptoms, extremely high blood pressure may lead to headaches, blurring of vision, and chest pain.
The easiest way to find out whether you have high blood pressure is to take your blood pressure. Untreated hypertension raises the risk of developing heart disease, stroke, and kidney damage, among other medical conditions.
Symptoms of abnormally high blood pressure, which is often 180/120 or greater, can include:
- difficulty breathing
- Anxiety
- vomiting
- confusion
- severe headaches
- vision problems, such as blurry vision
- bleeding noses
- nausea
- Pain in the chest
- feeling lightheaded or weak
- ear buzzing
- irregular heartbeat
Seek quick medical attention if you are suffering from any of these symptoms along with high blood pressure.
Risk Factors
There are multiple risk factors for high blood pressure, such as:
- Race. Black persons are more likely to have high blood pressure. Black people experience it at an earlier age than White people experience.
- Family history. If you have a parent or sibling who has high blood pressure, you are more likely to get the condition.
- Age. Increasing age raises the risk of high blood pressure. High blood pressure is more common in men up to the age of 64. Women above the age of 65 are more likely to have high blood pressure.
- lack of exercise. Gaining weight might result from not exercising. Elevated body weight increases the chance of hypertension. In addition, inactive people usually have higher heart rates.
- usage of tobacco or vaping. For a brief period, vaping, smoking, and chewing tobacco all cause blood pressure to rise quickly. Smoking tobacco damages the lining of blood vessels and promotes the artery-hardening process. If you are a smoker, ask your healthcare provider for advice on quitting smoking.
- An excessive amount of salt. The buildup of sodium, or salt, in the body can lead to fluid retention. Blood pressure rises as a result of this
- Low potassium levels. Potassium helps in regulating the body’s cell levels of salt. Maintaining a healthy potassium balance is essential for heart health. Low potassium levels can result from specific medical problems, such as dehydration, or a diet low in potassium.
- excessive alcohol consumption. Increased blood pressure has been associated with alcohol consumption, especially in males.
- Stress. High levels of stress might cause an instant rise in blood pressure. Stress-related behaviors like overeating, smoking, or drinking alcohol can raise blood pressure even more.
- multiple long-term diseases. Several diseases, including diabetes, sleep apnea, and kidney disease, can cause high blood pressure.
- pregnancy. Pregnancy can occasionally raise blood pressure.
Pathophysiology of hypertension
Since total peripheral vascular resistance (TPR) × cardiac output (CO) = blood pressure, pathogenic mechanisms include:
- Elevated CO
- A higher TPR
- Both
TPR is elevated and CO is either normal or slightly elevated in the majority of individuals. Primary hypertension, primary aldosteronism, pheochromocytoma, renovascular disease, and renal parenchymal disease are all associated with patterns similar to this one.
In other cases, TPR is unusually normal for the level of CO, and CO is elevated (maybe due to venous narrowing in big veins). TPR rises and CO returns to normal later in the disorder, most likely as a result of autoregulation. Isolated systolic hypertension can result from some conditions that raise CO (such as thyrotoxicosis, arteriovenous fistula, and aortic regurgitation), especially when stroke volume is raised. The aorta and its major branches’ inelasticity is likely the cause of isolated systolic hypertension with normal or low CO in some elderly people. Reduced CO is common in patients with high, constant diastolic pressures.
When blood pressure rises, plasma volume usually lowers; it rarely stays constant or even rises. When hypertension results from renal parenchymal disease or primary aldosteronism, plasma volume is often large; when hypertension results from pheochromocytoma, it may be relatively small.
When diastolic blood pressure rises and arteriolar sclerosis sets in, renal blood flow progressively decreases. The filtration fraction rises as a result of the glomerular filtration rate (GFR) remaining normal until late in the disease.
Unless severe atherosclerosis coexists in these arterial beds, blood flow is maintained in the heart, brain, and muscles.
Abnormal sodium transport
Abnormal sodium transport across the cell wall occurs in many cases of hypertension, Because of increased permeability to sodium ions or defects in the sodium-potassium pump (Na+, K+-ATPase), Increased intracellular sodium is the result, and this increases the cell’s sensitivity to sympathetic stimulation.
Since calcium follows sodium, the buildup of intracellular calcium could be the cause of the increased sensitivity. Inhibiting Na+, K+-ATPase may also increase the effect of norepinephrine, raising blood pressure, since this enzyme can pump norepinephrine back into sympathetic neurons, inactivating the neurotransmitter. Children who have a parent with hypertension but are normotensive may have deficiencies in sodium transport.
Sympathetic nervous system
Blood pressure is raised by sympathetic activation, typically to a higher level in patients with hypertension and increased blood pressure than in those with normotension. It is unknown where this hyperresponsiveness is located—in the heart, vascular smooth muscle, or the sympathetic nervous system.
Hypertension is known to be predicted by a high resting pulse rate, which may be caused by increased sympathetic nerve activity.
During rest, circulating plasma catecholamine levels are elevated among some hypertension people.
Renin, angiotensin, and aldosterone system
Renin, angiotensin, and aldosterone control blood pressure by regulating blood volume. The juxtaglomerular apparatus produces the enzyme renin, which catalyzes the conversion of angiotensinogen to angiotensin I.
Angiotensin-converting enzyme (ACE), which is primarily found in the lungs but is also found in the kidneys and brain, cleaves this inactive product into angiotensin II, a powerful vasoconstrictor that also activates the brain’s autonomic centers to increase sympathetic discharge and triggers the release of aldosterone and vasopressin.
Vasopressin and aldosterone increase blood pressure by causing sodium and water retention. Potassium excretion is further improved by aldosterone; low plasma potassium (< 3.5 mEq/L [< 3.5 mmol/L]) causes vasoconstriction by closing potassium channels.
Circulating angiotensin III has substantially less pressor action than angiotensin II but still induces aldosterone production just as strongly.
Medication that inhibits ACE does not completely stop the synthesis of angiotensin II since chymase enzymes also convert angiotensin I to angiotensin II.
There are at least four mechanisms that regulate renin secretion, and they are not exclusive:
- Variations in the tension inside the afferent arteriolar will generate a response from a renal vascular receptor.
- A macula densa receptor monitors variations in the distal tubule’s sodium chloride transport rate or concentration.
- Renin secretion is negatively impacted by circulating angiotensin.
- Renin secretion is stimulated by the sympathetic nervous system and is mediated by beta-receptors (via the renal nerve)
The renin-angiotensin-aldosterone system is thought to have a part in primary hypertension, while angiotensin is usually accepted to be the cause of renovascular hypertension, at least in its early stages. Renin levels, however, are often low in elderly individuals with hypertension and patients of African descent. Low levels of angiotensin II are also common in older people.
Renoprival hypertension, or hypertension brought on by chronic renal parenchymal disease, is the outcome of both volume-dependent and renin-dependent mechanisms working together. Increased renin activity is typically not detectable in peripheral blood. Usually mild, hypertension is susceptible to changes in sodium and water balance.
Vasodilator deficiency
Hypertension may result from a deficiency of a vasodilator (bradykinin, nitric oxide) compared to an excess of a vasoconstrictor (angiotensin, norepinephrine). Aging causes reductions in nitric oxide, which causes salt sensitivity (i.e., consuming less salt will result in a higher blood pressure reading than in younger individuals—2).
Stiff artery-related nitric oxide reduction is associated with salt-sensitive hypertension, which is defined as an abnormal rise in systolic blood pressure of more than 10 to 20 mm Hg following a high sodium load, such as a salty meal.
Blood pressure may rise if the kidneys cannot produce enough vasodilators due to renal parenchymal disease or bilateral nephrectomy.
Endothelial cells also produce vasoconstrictors, primarily endothelin, and vasodilators. Therefore, blood pressure is significantly impacted by endothelial dysfunction.
Diagnosis
Sphygmomanometry makes the diagnosis of hypertension. To figure out the cause and whether the target organs have been damaged, a history, physical examination, and other tests are helpful.
Blood pressure measurement
The blood pressure average calculated from two or three measurements taken of the patient at various periods should be considered for the official diagnosis:
- Seated for more than five minutes in a chair (not an examination table), with feet on the ground and a supported back
- with their limb elevated to heart level and the area where the cuff is placed uncovered by clothing
- Having avoided smoking, coffee, and exercising for at least thirty minutes
Measure blood pressure in both arms at the initial visit; the arm that provided the higher result should be used for the following measurements.
The upper arm is fitted with a BP cuff that fits well. Two-thirds of the biceps are covered by a cuff that fits well; the bladder is long enough to wrap more than 80% of the arm, and its width is at least 40% of the arm’s diameter. Therefore, big cuffs are typically needed for overweight patients.
While listening over the brachial artery, the clinician gradually releases the air from the cuff after inflating it over the anticipated systolic pressure. Systolic blood pressure is the point at which the first heartbeat is audible when the pressure decreases. The sound completely stops signaling diastolic blood pressure.
The radial artery in the forearm and the popliteal artery in the thigh are measured using the same principles. Automatic readers are frequently unreliable, thereby mechanical devices should be calibrated regularly.
More blood pressure readings are preferred if the reading is in the stage 1 hypertensive range or is noticeably labile. Before hypertension becomes chronic, blood pressure readings may be intermittently high. This phenomenon is likely responsible for “white coat hypertension,” in which blood pressure is higher in the doctor’s office but normal at home or via ambulatory blood pressure monitoring.
When “white coat hypertension” is suspected, ambulatory or at-home blood pressure monitoring is advised. Furthermore, when “masked hypertension” (a condition in which blood pressure measured at home is higher than values gained in the clinician’s office) is suspected, ambulatory blood pressure monitoring may also be indicated. This condition typically affects patients who show hypertension-related symptoms but lack evidence of hypertension based on in-office measurements.
History
The history involves the following:
- Duration of hypertension and earlier blood pressure readings
- Heart failure, obstructive sleep apnea, or coronary artery disease history or symptoms
- Symptoms show additional important associated conditions, such as gout, diabetes, dyslipidemia, peripheral artery disease, stroke, and renal failure, either personally or in one’s family.
- Usage of drugs that increase the risk of hypertension, such as NSAIDs and oral contraceptives that include estrogen
- Duration of sleep.
Exercise habits and usage of alcohol, tobacco, and stimulants (including prescription medicines and illegal narcotics) are all part of social history.
Food intake and stimulant consumption such as tea, coffee, sodas with caffeine, and energy drinks are the main topics of a nutritional history.
Physical examination
Measurements of height, weight, and waist circumference are part of the physical examination, along with a complete cardiac, respiratory, and neurologic examination, a funduscopic examination for retinopathy, and auscultation for bruits in the neck and the stomach.
Abdominal tumors and enlargement of the kidneys are palpated. Evaluation of peripheral arterial pulses is conducted; femoral pulses that are reduced or delayed suggest aortic coarctation, especially in patients under 30 years of age. Thin patients with renovascular hypertension may hear a single renal artery bruit.
Testing
Following a blood pressure measurement-based diagnosis of hypertension, testing is required to:
- Detect damage to the target organ.
- Identify the risk factors for cardiovascular disease.
The level of the evaluation increases with the severity of the patient’s hypertension and age. Tests might include:
- Renal ultrasound should be considered if there are any abnormalities in the urine, albumin, and creatinine ratio.
- Complete metabolic panel (which includes potassium, calcium, and creatinine), lipid panel, and fasting plasma glucose ECG
- Thyroid-stimulating hormone levels can sometimes be measured
- Measurement of plasma-free metanephrines can occasionally be used to identify pheochromocytomas.
- A sleep study may sometimes
More tests might be required based on the examination and initial test findings.
If a urinalysis finds casts, albuminuria (proteinuria), microhematuria, or if serum creatinine or cystatin C is increased, renal ultrasonography to assess kidney size may be helpful.
Plasma aldosterone levels and plasma renin activity are used to assess patients with hypokalemia unrelated to diuretic therapy for high salt intake and intrinsic aldosteronism. Approximately 10 to 20% of patients with resistant hypertension have primary aldosteronism, a number that is significantly higher than earlier estimates.
A broad, notched P-wave on the electrocardiogram (ECG) is indicative of atrial hypertrophy and, while nonspecific, could be among the initial indications of hypertensive heart disease. Elevated QRS voltage is indicative of left ventricular hypertrophy (LVH) and can happen later, even in the absence of ischemia. Echocardiograms are typically performed when LVH is observed on the ECG.
When aortic coarctation is suspected, diagnostic imaging such as echocardiography, CT scan, or MRI aids in the diagnosis.
Plasma-free metanephrine screening is used to test for pheochromocytoma in patients with labile, significantly increased blood pressure, and symptoms such as pallor, headache, palpitations, a rapid heartbeat, heavy perspiration, and tremors.
Thyroid-stimulating hormone (TSH) measurement is the initial step in the screening process for hyperthyroidism. If a person’s medical history points to sleep apnea, they should seriously consider getting a sleep study done.
Further investigation is necessary for patients showing symptoms suggestive of Cushing syndrome, systemic rheumatic diseases, eclampsia, acute porphyria, hyperthyroidism, myxedema, acromegaly, or disorders of the central nervous system (CNS).
Treatment of Hypertension
Medications
The kind of medication used to treat hypertension is decided by your blood pressure level and general health. It’s common for two or more blood pressure medications to function better than one. Finding the medication or medication combination that is most effective for you may take some time.
Knowing your target blood pressure level is important while taking blood pressure medication. A blood pressure treatment target of less than 130/80 mm Hg is what you should aim for if:
- You’re a fit adult who is 65 years of age or older.
- You are a healthy adult under 65 years old who has a 10-year risk of cardiovascular disease of 10% or more.
- You suffer from diabetes, coronary artery disease, or chronic kidney disease.
Age and medical problems can have an impact on the ideal blood pressure target, especially if you’re over 65.
High blood pressure is treated with the following medications:
- Diuretics (water pills). These medications help in the body’s removal of water and sodium. When treating high blood pressure, these are frequently the first medications used. Diuretics come in several types, such as potassium-sparing, thiazide, and loop. The only one is any additional medical issues, such as heart failure or kidney disease. Diuretics such as chlorthalidone and hydrochlorothiazide (Microzide) are frequently used to treat hypertension. Increasing urine production is a common diuretic adverse effect. High urination can lower potassium levels. A healthy potassium balance is necessary for proper heartbeat. Your medical professional might suggest a potassium-sparing diuretic that contains triamterene if you have low potassium or hypokalemia.
- Inhibitors of the angiotensin-converting enzyme (ACE). These medications aid in blood vessel relaxation. They prevent a naturally occurring substance from constricting blood arteries. Benazepril (Lotensin), captopril, lisinopril (Prinivil, Zestril), and other medications are examples.
- Blockers of the angiotensin II receptor (ARBs). These medications relax blood vessels as well. They obstruct a naturally occurring chemical that narrows blood arteries, not the chemical’s synthesis. Among the angiotensin II receptor blockers (ARBs) are losartan (Cozaar), candesartan (Atacand), and other medications.
- Blockers of calcium channels. These medications help in the blood vessel’s muscular relaxation. Some cause your heart rate to slow. They consist of diltiazem (Cardizem, Tiazac, and other brands), amlodipine (Norvasc), and other brands. When taking calcium channel blockers, avoid eating or drinking grapefruit-based products. Some calcium channel blockers are elevated in the blood by grapefruit, which can be harmful. Should you be worried about interactions, check with your pharmacist or healthcare professional.
Other medications that are occasionally used to treat hypertension
Your doctor may recommend the following if the above medication combinations aren’t helping you achieve your blood pressure target:
- Alpha blockers. These drugs reduce the impulses that nerves provide to blood arteries. They reduce the effects of organic compounds that constrict blood arteries. Examples include Doxazosin (Cardura), prazosin (Minipress), and other alpha-blockers.
- Alpha-beta blockers. Alpha-beta blockers reduce the heartbeat by obstructing nerve signals to blood vessels. They decrease the blood volume that needs to be circulated via the arteries. Two examples of alpha-beta blockers are labetalol (Trandate) and carvedilol.
- Beta-blockers. These medications enlarge blood arteries and lessen the strain on the heart. This facilitates a slower, less forceful heartbeat. Metoprolol (Lopressor, Toprol-XL, Kapspargo Sprinkle), atenolol (Tenormin), and other medications are examples of beta blockers. It is not normally advised to administer beta blockers as the only medication. When taken alongside other blood pressure medications, they function best.
- Aldosterone antagonists. Resistant hypertension may be treated with these medications. They prevent the body from accumulating salt and fluid due to the action of a naturally occurring molecule. Spironolactone (Aldactone) and eplerenone are two examples.
- Renin-inhibitors.. Aliskiren (Tekturna) decreases the kidneys’ synthesis of renin, an enzyme that initiates a series of chemical reactions that raise blood pressure.
- VasodilatorsThese medications stop the arterial wall muscles from contracting. By doing this, the arteries are kept from narrowing. Minoxidil and hydralazine are two examples.
- Central-acting agents. These medications stop the neurological system from receiving signals from the brain to shorten blood vessels and raise heart rate. Clonidine (Catapres, Kapvay), guanfacine (Intuniv), and methyldopa are a few examples.
Always take the recommended blood pressure medication. Never miss a dosage or stop taking blood pressure medication suddenly. Rebound hypertension is a sudden rise in blood pressure that can occur when certain medications, such as beta-blockers, suddenly stop working.
Home remedies for high blood pressure.
Healthy changes to your lifestyle can help you control the risk factors for hypertension. These are a few of the most common examples.
Developing a heart-healthy diet.
A heart-healthy diet can help control high blood pressure. It is also useful for treating well-controlled hypertension and lowering the risk of complications. Heart disease, stroke, and heart attack are some of the possible complications.
A heart-healthy diet points out:
- Vegetables
- Whole grains
- Fruits
- Lean proteins, such as fish
Increasing physical activity
In addition to weight loss (if suggested by your doctor), exercise can naturally lower blood pressure as well as improve your cardiovascular system.
Weekly targets should include 150 minutes of moderate exercise. That takes around 30 minutes, five times each week.
Reaching an optimum weight
If you have to be overweight, maintaining an appropriate weight with a heart-healthy diet and increased physical exercise will help lower your blood pressure.
Stress management
Exercising is a good way to reduce stress. Other activities can be beneficial. This includes:
- Deep breathing.
- muscle Relaxation
- meditation
- Yoga
- massage
Getting enough sleep may also help relieve stress.
Quitting smoking and limiting drinking alcohol.
If you are a smoker and have been diagnosed with high blood pressure, your doctor will probably advise you to stop. The chemicals found in tobacco smoke can harm the body’s tissues and stiffen blood vessel walls.
See a therapist to reduce your alcohol consumption or stop altogether if you have an alcohol addiction or consume too much. Drinking too much alcohol might elevate your blood pressure.
If you have hypertension risk factors, you can take action right away to reduce your chances of developing the condition and its complications.
Lifestyle Changes That Lowering Your Risk of Hypertension
Add vegetables and fruit to your diet.
Gradually increase your intake of heart-healthy vegetables. Aim to eat seven servings of fruits and vegetables every day. Then, attempt to add one extra serving per day for two weeks. After those two weeks, plan to add one additional serving. The goal is to consume ten servings of fruits and vegetables each day.
Limit refined sugar.
Try to restrict your daily intake of sugar-sweetened items such as flavored yogurts, cereals, and sodas. Packaged foods include unnecessary sugar, so read the labels.
Reduce your salt consumption.
People with hypertension and those at risk for heart disease may be advised by their doctor to keep their daily salt consumption between 1,500 milligrams and 2,300 milligrams per day.
The simplest way to minimize salt is to cook fresh foods more frequently and limit your intake of fast food and prepackaged foods, both of which can be rich in sodium.
Set weight loss goals
If your doctor has recommended that you lose weight, talk to them about the best weight reduction target for you. The Centers for Disease Control and Prevention (CDC) suggests losing one to two pounds every week. This can be accomplished by a healthier diet and greater physical activity.
Using a trainer or fitness app, as well as maybe a dietitian, can help you understand how to make the best decisions for your body and lifestyle.
Monitor your blood pressure regularly.
Early detection of hypertension is the most effective strategy to avoid complications and issues.
Keep a record of your blood pressure readings and bring it to your regular doctor’s appointments.
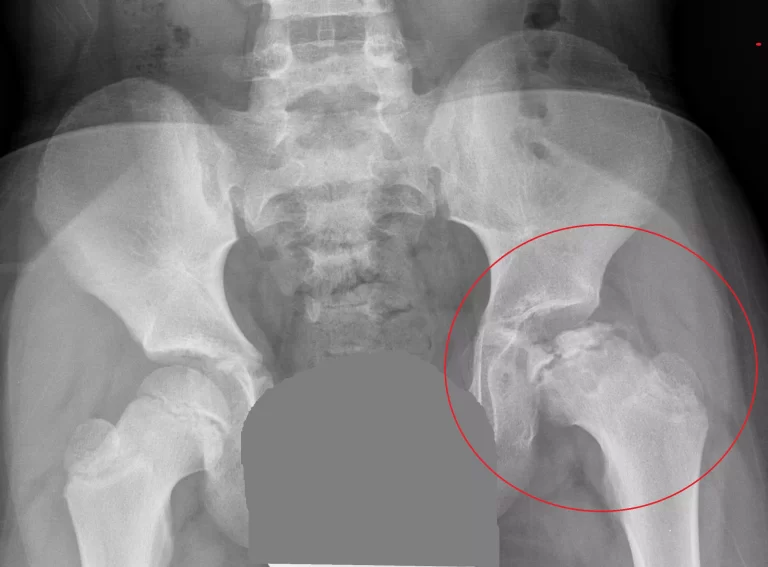
Differential Diagnosis
When making a differential diagnosis, secondary hypertension should always be considered, particularly if the patient is at an extreme age (young or older).
The differential diagnosis should always include:
- hyperaldosteronism
- aortic valve disease
- renal artery stenosis
- coarctation of the aorta
- chronic kidney disease
Complications
High blood pressure causes excessive pressure on artery walls, which can damage blood vessels and organs. The higher the blood pressure and the longer it remains uncontrolled, the worse the damage.
Uncontrolled high blood pressure might result in complications like:
- Heart attack or a stroke. High blood pressure-induced arterial hardening and thickening can result in a heart attack, stroke, or additional complications.
- Aneurysm. Increased blood pressure can cause a blood artery to weaken and bulge, resulting in an aneurysm. A ruptured aneurysm can be deadly.
- Heart failure. High blood pressure causes your heart to work harder to pump out blood. The strain causes the wall of the heart’s pumping chamber to thicken. This disease is known as left ventricular hypertrophy. The heart eventually fails because it is unable to pump enough blood to meet the body’s needs.
- Kidney problems. High blood pressure can cause the blood arteries in the kidneys to constrict and weaken. This can cause renal damage.
- Problems with the eyes. Increased blood pressure can lead to thickened, constricted, or torn blood vessels in the eyes. This can cause visual loss.
- Metabolic Syndrome. This syndrome refers to a group of metabolism-related diseases. It involves the irregular breakdown of sugar, often known as glucose. The syndrome is characterized by an expanded waist circumference, high triglycerides, low high-density lipoprotein (HDL or “good”) cholesterol, high blood pressure, and high blood sugar levels. Your chance of acquiring diabetes, heart disease, and stroke is raised by these conditions.
- Changes in memory or understanding. Uncontrolled high blood pressure can impair the ability to think, remember, and learn.
- Dementia. Blood flow to the brain might be limited due to narrowed or clogged arteries. This can lead to vascular dementia. A stroke that stops blood flow to the brain can potentially result in vascular dementia.
Types of Hypertension
Hypertension is classified as systemic hypertension or localized hypertension based on whether it affects the entire body or just a specific area.
There are multiple forms of systemic hypertension, which include:
- Essential or primary hypertension: This form of hypertension has an unknown origin and affects the majority of individuals (approximately 90%). Essentially, genetics play an important effect in it.
- Secondary hypertension occurs owing to a variety of unique factors.
- Malignant hypertension is characterized by severe high blood pressure that damages the target organ.
- Isolated systolic hypertension is a common occurrence in the elderly due to elasticity loss in major arteries.
- Resistant hypertension is defined as the persistence of higher blood pressure despite treatment with more than three antihypertensive medications.
- Refractory hypertension is defined as high blood pressure that persists despite treatment with more than five different antihypertensive medications.
- Postpartum hypertension occurs when blood pressure peaks three to six days after giving birth, even in mothers with normal blood pressure.
- Preeclampsia (pregnancy-related hypertension): During pregnancy, it is common to develop hypertension known as gestational hypertension or preeclampsia, which raises the risk of maternal death and fetal abnormalities.
- White coat hypertension occurs during hospital stays but is otherwise normal. In India, shockingly, younger populations have a higher incidence of white coat hypertension than the elderly.
- Masked hypertension occurs when blood pressure seems normal at the doctor’s office but is elevated outside of the office.
- Labile hypertension refers to frequent variations in blood pressure (between normal and high).
- Nocturnal hypertension refers to having a blood pressure of ≥120/70 mmHg at night. It is capable of causing subclinical organ damage.
- Permissive hypertension is a treatment-induced technique used to keep blood pressure elevated following a stroke by lowering hypertensive medication. It helps a quicker recovery.
- Hypertension is connected with asthma. This was proven after years of research, but the causes are unknown.
- Carcinoid hypertension occurs when cancer releases chemicals into the bloodstream, which can lead to a variety of problems. Hypertension is one of these.
- Pseudohypertension is a falsely inflated blood pressure reading seen in the elderly, diabetics, or people with a chronic renal illness caused by stiff, calcified brachial arteries.
There are multiple types of local hypertension:
- Portal hypertension is elevated blood pressure in the liver (portal vein) and the capillaries that branch from it.
- Pulmonary hypertension is defined as elevated blood pressure exerted against the blood arteries that connect the heart and lungs.
- Idiopathic intracranial hypertension: Increased pressure in the brain (for unknown reasons), resulting in vision changes and headaches.
- Epididymal hypertension occurs when blood accumulates in the testicles during arousal, resulting in pain and a firm erection. This condition is also known as blue balls.
- Ocular hypertension is defined as elevated intraocular pressure (high pressure in the aqueous humor of the eyes) caused by a failure in fluid outflow.
- Postural hypertension is defined as hypertension that occurs while standing upright, often known as orthostatic hypertension.
- Renovascular hypertension occurs when the blood supply to the kidneys is compromised. This dangerous condition could result in a heart attack, a stroke, or even death.
- Venous hypertension is defined as elevated blood pressure in the veins, particularly in the lower extremities (legs), caused by compromised vein valves.
- Pediatric hypertension refers to elevated blood pressure in children and adolescents between the 90th and 95th percentiles based on height, gender, and age. Hypertension is defined as blood pressure above or equal to the 95th percentile.
- Reactive pulmonary hypertension: During hypoxia (low oxygen levels), blood pressure in the pulmonary vasculature rises, which can be managed with medications or by raising alveolar oxygen tension.
Prognosis
Large-scale meta-analyses have also indicated that rising systolic and diastolic blood pressures increase the risk of cardiovascular disease and vascular disease, with the risk of death from heart disease and stroke nearly doubling with increased SBP of up to 20 and DBP of 10 mm Hg, respectively.
The prognosis is dependent on blood pressure control and is only positive if blood pressures are adequately controlled; however, complications may occur in some patients due to hypertension’s progressive nature.
Adequate control and lifestyle changes only serve to delay the onset and progression of complications like chronic kidney disease and renal failure.
Consultations
Such individuals should be managed together by A cardiologist, nephrologist, and hypertension expert should work together to care for people with this condition.
Patients usually need psychosocial therapy as well as consultations with nutritionists and dietitians.
Patient Education
Hypertension is a chronic condition that requires long-term treatment and management. Detailed education about lifestyle modifications and pharmacological therapy is necessary for better blood pressure control and avoiding problems.
Weight control, physical activity, and restricting alcohol, tobacco, and smoking are essential strategies for reducing cardiovascular risk.
Result of Healthcare Team Outcomes
Nurses charting patients in ERs and outpatient settings frequently detect hypertension, which requires rapid recognition and referral to a physician because the majority of these hypertensive patients may be unaware of their disease, hence the term “silent killer.”
Inter-professional communication is essential, especially in cases of resistant or difficult-to-treat hypertension, where a referral and inter-specialty strategy can help a patient the best.
Effective communication in an interprofessional team approach, which includes nursing staff and nurse practitioners, primary referring physicians, cardiologists, nephrologists, and pharmacists, plays an important role in maintaining blood pressure control. This team can also monitor for proper patient compliance, as well as potential toxicities and adverse effects, resulting in fewer future problems, lower healthcare costs, and better patient outcomes.
FAQ
References
What is the main cause of hypertension?
Hypertension usually develops over time. It can happen as a result of bad lifestyle choices, such as failing to participate in adequate regular physical activity. Some medical disorders, like diabetes and obesity, might raise the chance of developing high blood pressure.
What are the 5 symptoms of hypertension?
If hypertension is severe enough, it can harm the brain and cause symptoms including tiredness, headaches, nausea, vomiting, shortness of breath, restlessness, and loss of vision. In rare situations, it might cause brain swelling, resulting in drowsiness and coma.
How serious is Stage 2 hypertension?
A blood pressure level that is more than 180/120 mm Hg is called a hypertensive emergency or crisis. If anyone has these blood pressure levels, get emergency medical attention. High blood pressure, when untreated, raises the risk of a heart attack, stroke, and other major health problems.
What are 3 treatments for hypertension?
Hypertension can be treated with a variety of medications, including Inhibitors of the angiotensin-converting enzyme. Diuretics are angiotensin II receptor blockers (ARBs).
Can hypertension be cured?
While there is no cure for high blood pressure, patients must take the proper steps, such as making successful lifestyle modifications and using BP-lowering drugs as prescribed by their doctors.
How can hypertension be reduced?
Lose weight and watch your waistline.
Regular exercise
Eat a healthy diet.
Reduce your salt (sodium) intake.
Sleep well.
lower your stress level
- Iqbal, A. M. (2023, July 20). Essential Hypertension. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK539859/
- Hypertension – Symptoms, Causes, Types, Complications, Prevention. (2023, July 6). https://www.pacehospital.com/hypertension-symptoms-causes-types-complications-prevention
- High blood pressure (hypertension) – Symptoms & causes – Mayo Clinic. (2022, September 15). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/symptoms-causes/syc-20373410
- Holland, K. (2023, March 27). Everything You Need to Know About High Blood Pressure (Hypertension). Healthline. https://www.healthline.com/health/high-blood-pressure-hypertension#treatment
- Bakris, G. L. (2024, January 29). Hypertension. MSD Manual Professional Edition. https://www.msdmanuals.com/en-in/professional/cardiovascular-disorders/hypertension/hypertension
- Hypertension. (2023, March 16). https://www.who.int/news-room/fact-sheets/detail/hypertension
- High blood pressure in adults – hypertension: MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/article/000468.htm






3 Comments