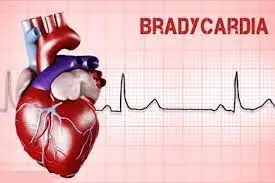
Bradycardia
What is Bradycardia?
Bradycardia is described as a heart rate (HR) lower than 50–60 bpm, & it’s marked as a regular phenomenon in young, athletic individuals, as well as in patients as a position of genuine aging or because of particular illnesses.
Research indicates the presence of a circadian cycle in HR, with the fastest rates occurring between 2:00 PM to 5:00 PM and the slowest rates between 4:00 AM to 6:00 AM. During sleep, HR decreases by an average of 24 beats per minute in young adults and 14 beats per minute in individuals over 80 years of age. Interestingly, women tend to exhibit a higher HR than men during both wakefulness and sleep, with an average difference of 10 bpm in young adults.
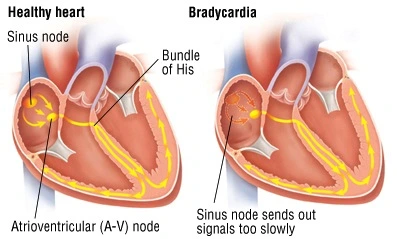
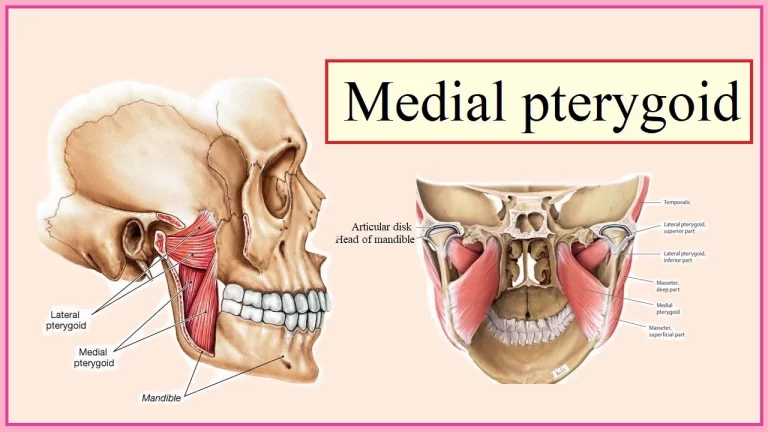
The sinoatrial (SA) node serves as the initiator and regulator of the cardiac rhythm, acting as the heart’s primary pacemaker. Structurally, the SA node contains sets of technical cardiomyocytes enveloped by strands of connective tissue understood as fibrosis. The SA conduction ways establish electrical references between the SA node & the right atrium, recreating an essential role in managing SA node automaticity & therefore preserving the heart rate.
Numerous factors contribute to the modulation of HR, including the autonomic nervous system, which represents a dynamic equilibrium between the sympathetic and parasympathetic nervous systems. Additionally, baroreceptors, the Bainbridge reflex, intrinsic heart rate, and more play roles in influencing HR. The cardiac conduction system and the SA node exhibit a higher density of innervation by the autonomic nervous system, underscoring its pivotal role in initiating and regulating the cardiac impulse.
How to differentiate bradycardia and tachycardia?
Bradycardia and tachycardia stand as contrasting conditions in the realm of heart health.
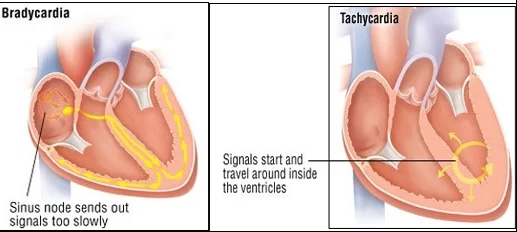
- Bradycardia: The term ‘bradycardia’ finds its origins in the Greek words ‘Bradys’ and ‘kardia,’ which collectively signify ‘slow heart.’
- Tachycardia: Similarly drawn from the Greek language, ‘tachycardia’ amalgamates ‘tachys’ and ‘kardia,’ conveying the notion of a ‘swift heart.’
Whom does it impact?
Bradycardia can manifest across various ages and backgrounds, yet it holds a higher prevalence among adults aged over 65. Its occurrence is relatively rarer in younger adults and children, owing to the inherent gradual slowing of heart rate with advancing age. Notably, exceptions arise when the condition arises due to certain congenital or genetic factors.
Furthermore, its occurrence is more pronounced among individuals bearing specific medical conditions, some of which may be hereditary or passed down from parents, or induced by certain categories of medications. Trauma to the chest region or nutritional challenges and eating disorders can also contribute to its emergence.
How common is this condition?
Bradycardia is prevalent within specific age brackets and circumstances, impacting certain populations. It predominantly manifests in the following groups:
- Individuals aged over 65: This condition gives rise to symptoms in approximately 1 out of every 600 adults beyond the age of 65. Consequently, there exists a population exceeding half a million individuals aged over 65 who exhibit symptomatic signs of this condition. It is worth noting that the number of individuals with bradycardia, albeit lacking symptoms, is likely significantly higher. Notably, among older adults, bradycardia tends to be particularly prevalent during periods of sleep.
- Highly physically active individuals: People who engage in regular exercise can develop bradycardia due to their robust physical condition. Remarkably, this form of bradycardia does not adversely affect these individuals, given that their well-conditioned hearts efficiently pump blood, satisfactorily meeting the body’s demands despite the slower heartbeat.
Is bradycardia an arrhythmia?
Bradycardia, characterized by a heart rate slower than the typical rate, qualifies as an arrhythmia, signifying an abnormal heart rhythm. The standard heart rate range for adults spans from 60 to 100 beats per minute.
Sinus rhythm denotes a heart beating regularly and in its usual pattern. Sinus bradycardia, on the other hand, signifies a situation where the heart maintains a regular beat but at a slower pace than the norm. Notably, sinus bradycardia is generally considered a benign arrhythmia, particularly among highly active individuals. This implies that although the heart rate is below the anticipated range, it doesn’t pose significant harm.
While bradycardia stands as a distinct medical condition, it often arises concurrently with, or as a result of, other underlying conditions. In such instances, treating bradycardia tends to focus more on addressing it as a symptom intertwined with the primary condition, rather than as an isolated ailment.
How does this condition affect my body?
Bradycardia manifests when the heartbeat is slower than the standard rate for adults. This situation becomes concerning when the heart’s rhythm is insufficient to meet the body’s oxygen requirements adequately. The resulting reduction in blood flow and oxygen delivery has far-reaching consequences, primarily impacting vital organs such as the brain and heart.
Types of bradycardia
There are various kinds of bradycardia, relying on which region of the heart they begin in.
Sinus bradycardia:
Sinus bradycardia constitutes a type of slow heart rate that originates from the sinoatrial (SA) node within an individual’s heart.
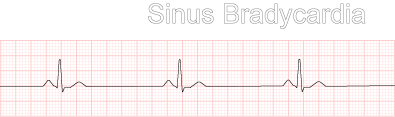
In the case of sinus bradycardia, the SA node generates the electrical impulses to initiate heartbeats; however, these impulses are produced at a slower rate, leading to a reduced heart rate.
The majority of individuals experiencing sinus bradycardia typically remain asymptomatic. This condition can emerge in physically active or athletic individuals, as well as during deep sleep. Nevertheless, sinus bradycardia can also arise due to various health conditions, including heart disease.
Junctional bradycardia:
Junctional bradycardia occurs when the electrical signal initiating the heartbeat arises from the atrioventricular (AV) node rather than the SA node.
Situated at the base of the right atrium, the AV node functions as a backup pacemaker when the SA node’s function is compromised. Additionally, the AV node creates a pause in the electrical impulse from the SA node, allowing the heart’s atria to complete their contractions, causing blood to accumulate in the ventricles. Subsequently, the impulse travels to the His-Purkinje system, triggering the ventricles to contract and propel blood out of the heart.
Junctional bradycardia can occur when issues with the SA node prompt the AV node to assume control. This condition can also affect physically active individuals, young children, and people during deep sleep.
Ventricular:
Idioventricular rhythm also referred to as atrioventricular bradycardia or ventricular escape rhythm, manifests as a heart rate below 50 BPM. This mechanism acts as a safety measure when there’s a lack of electrical impulses from the atrium. Impulses originating below or within the bundle of His result in a broad QRS complex, with heart rates ranging between 20 and 40 BPM. Impulses originating above the bundle of His, termed junctional, typically lead to heart rates between 40 and 60 BPM, featuring a narrow QRS complex.
In cases of third-degree heart block, around 61% occur at the bundle branch-Purkinje system, 21% at the AV node, and 15% at the bundle of His. AV block can be identified through an ECG showcasing a “1:1 relationship between P waves and QRS complexes.” Ventricular bradycardias can co-occur with sinus bradycardia, sinus arrest, and AV block. Treatment typically involves administering atropine and cardiac pacing.
Infantile:
In the context of infants, bradycardia denotes a heart rate below 100 BPM (with the normal range around 120–160 BPM). Premature infants are more prone to experiencing episodes of apnea and bradycardia compared to full-term babies. The cause of these episodes remains somewhat elusive but could be linked to underdeveloped brain centers that regulate breathing.
Gently touching the baby or gently rocking the incubator typically prompts the baby to resume breathing, thereby increasing the heart rate. Medications like theophylline or caffeine might be employed to address these episodes in infants if necessary. Within neonatal intensive care units (NICUs), continuous electronic monitoring of heart and lung activity is standard practice to address these occurrences.
Symptoms and Causes of Bradycardia
What are the symptoms associated with bradycardia?
In numerous cases, bradycardia manifests without any noticeable symptoms. This is particularly true for individuals who are highly physically active, as their efficient hearts compensate for the slower rate. However, for those whose hearts lack the capacity to adapt, the symptoms may encompass:
- Shortness of breath.
- Chest pain (resembling angina).
- Fatigue.
- Heart palpitations (the unsettling sensation of your heart’s rhythm, distinct from manually checking your pulse).
- Memory difficulties.
- Confusion.
- Challenges in concentration.
- Dizziness, lightheadedness, and even fainting (syncope).
- Mood alterations, including irritability or restlessness.
These symptoms arise due to the impacts of bradycardia on both the heart and the brain.
Brain:
Despite its modest size, the human brain, constituting around 1.6% of a 180-pound person’s total weight, receives 15-20% of the blood ejected from the heart. Inadequate blood flow significantly affects brain function.
Heart:
The symptoms of bradycardia often mirror those of heart failure. Additionally, bradycardia can resemble angina, characterized by chest discomfort or pressure that signals potential heart disease.
Measuring Heart Rate:
Individuals can gauge their heart rate by assessing their pulse. For an accurate resting heart rate measurement, one should be seated or lying down, in a calm and relaxed state. Pulse can be checked in various body areas, including the wrists, side of the neck, inside of the elbows, and top of the feet. Using two fingers, the pulse can be felt to identify the most accessible location.
The thumb should not be used for this purpose, as it has its pulse and could distort the results. Counting the number of beats over 60 seconds provides the heart rate. A heart rate low than 60 bpm demonstrates bradycardia. However, bradycardia doesn’t always signal an underlying health condition. Consulting a doctor is recommended to determine its cause.
Children and young individuals typically exhibit faster heart rates compared to adults. Infants might have a heart rate of around 140 bpm, while older children and teenagers typically maintain a resting heart rate of about 70 bpm.
What causes this condition?
Bradycardia can manifest due to a diverse range of factors. Among the numerous common causes are the following:
- Electrolyte Imbalances: Insufficient intake of vital electrolytes such as calcium, magnesium, and potassium can influence heart rate.
- Anorexia Nervosa: This eating disorder can contribute to the development of bradycardia.
- Inflammation: Inflammation affecting different aspects of the heart, such as the inner lining (endocarditis), heart muscle (myocarditis), or the pericardial sac (pericarditis), can trigger bradycardia.
- Infections: Bacteria responsible for many strep throat infections can also inflict damage upon the heart, particularly the heart valves if not promptly treated.
- Rheumatic Fever and Rheumatic Heart Disease: Untreated bacterial infections like strep throat can evolve into rheumatic fever, eventually leading to rheumatic heart disease several years later.
- Lyme Disease: Contracted through tick bites, Lyme disease, also known as borreliosis, can affect the heart if left untreated for an extended duration.
- Chagas Disease: Similar to Lyme disease, this condition emerges due to a parasite transmitted by blood-sucking insects known as “kissing bugs.”
- Sick Sinus Syndrome: This occurs when the heart’s natural pacemaker, the sinoatrial (SA) node, malfunctions, hindering its ability to generate the required electrical impulses that synchronize the heart’s contractions.
- Heart Block: This comprehensive term encompasses various disruptions within the heart’s electrical system, causing impediments or decelerations in the electrical currents, ultimately disrupting the heart’s rhythm. These blocks can occur at multiple points along the heart’s electrical conduction network.
- Medications: Prescription drugs like beta-blockers, calcium-channel blockers, anti-arrhythmia medications, narcotics, lithium, and even recreational substances like cannabis (marijuana) can induce bradycardia.
- Heart Surgery: Interventions addressing congenital heart conditions, valve repair, or valve replacement surgeries can lead to the development of bradycardia.
- Radiation Therapy: This treatment modality can result in toxic effects that subsequently trigger radiation heart disease.
Other underlying conditions encompass:
Sick Sinus Syndrome:
Known as sinus node dysfunction (SND), this ailment affects the sinoatrial (SA) node located at the apex of the right atrium. Responsible for initiating the electrical impulse that initiates a heartbeat, SND can result in varying heart rates—acceleration, deceleration, or a combination of both. Additional manifestations of SND encompass palpitations, feelings of fluttering, pounding, or pausing in the heart, as well as tiredness, lightheadedness, and fainting. While SND can manifest at any age, its typical onset occurs around the age of 68. It stands as a common cause of bradycardia.
Other Heart Electrical Abnormalities:
Failure of the heart to transmit electrical signals due to blockages or heart diseases can lead to bradycardia. Complete heart block occurs when communication between the atria and ventricles is severed, often due to the SA node’s inability to relay signals to the AV node. Complete heart block prompts independent activation of the atria and ventricles, a situation that demands swift medical attention to avert potential fatality.
Metabolic Disorders:
Certain metabolic disorders can decelerate heart rate. One prevalent example is hypothyroidism, where the thyroid gland produces insufficient hormones, possibly affecting blood vessel health and thus slowing heart rate. Common thyroid disorders, like hypothyroidism, can impact even young and otherwise healthy individuals, with a prevalence of 4 to 10% among individuals in the United States. Other metabolic conditions contributing to bradycardia include acidosis, elevated potassium levels (hyperkalemia), deficient potassium levels (hypokalemia), and hypothermia due to excessively low body temperature.
Heart-Damaging Conditions:
Heart damage stemming from specific conditions can impede effective pumping, resulting in a slower pace. Damaging conditions encompass congestive heart failure, coronary artery disease, heart attacks, myocarditis (inflammation of heart muscle), Lyme disease, thickened heart muscle, hypertension, and diabetes.
Heart Medications:
Certain medications, including those addressing heart disease and high blood pressure, might lower heart rates. Beta-blockers and calcium channel blockers, prescribed for rapid heart rates and certain heart conditions, may also induce a decrease in heart rate. Individuals initiating new medications and experiencing bradycardia symptoms should promptly consult a medical professional.
Oxygen Deprivation:
Hypoxia arises when bodily tissues lack sufficient oxygen, often due to choking, severe asthma attacks, or chronic conditions like chronic obstructive pulmonary disease. If hypoxia results in a decreased heart rate, prompt attention to the underlying cause is imperative.
Is Bradycardia Contagious?
Bradycardia is not contagious, although some of the underlying conditions causing it might be.
Diagnosis of Bradycardia
How is bradycardia diagnosed?
The diagnosis of bradycardia involves a comprehensive assessment conducted by a medical professional, combining physical examinations and specialized tests to gauge heart rate and analyze heart rhythm.
Which diagnostic tests are typically employed?
- Physical Examination: Healthcare providers perform a thorough physical examination to detect any visible indications of underlying conditions or anomalies. They may also employ tactile examination to identify changes that may not be visible but are perceptible through touch.
- Electrocardiogram (ECG/EKG): This essential test is climactic in analyzing bradycardia, as it meticulously tracks the electrical activity of the heart. By affixing multiple electrodes (typically 12) to your chest, this test captures the heart’s electrical impulses, portraying them as distinct waves on a paper printout or computer display.
- Laboratory Tests: Various lab tests aid in diagnosing bradycardia, many of which are used to rule out alternative problems. These tests encompass:
- Electrolyte Levels: Assessment of blood electrolyte levels, especially calcium, potassium, and magnesium.
- Thyroid Hormone Levels: Evaluation of thyroid hormone levels, as hypothyroidism (low thyroid function) can contribute to bradycardia.
- Troponin: This test measures a specific heart muscle protein called troponin, which is released into the blood following heart muscle cell damage. Elevated troponin levels can indicate heart damage, including heart attacks.
- Toxicology Screen: Identification of toxic substances within the bloodstream. This screen can pinpoint drugs, both prescription and recreational, that might lead to bradycardia, as well as other substances detrimental to the heart.
Additional tests might be recommended if bradycardia is detected, particularly if healthcare providers suspect an underlying condition. It is advisable to consult your healthcare provider to gain insight into any additional tests suggested and their rationale.
Treatment of Bradycardia
How is bradycardia treated, and is it curable?
If you’re experiencing bradycardia without noticeable symptoms, it’s improbable that treatment is necessary. However, for individuals with symptoms, bradycardia is frequently manageable and occasionally even reversible. In instances where bradycardia is a result of an underlying medical issue, addressing that root cause can often resolve the bradycardia. For instance, if medication is causing your bradycardia, adjusting the medication could lead to its cessation.
What medications/treatments are used?
There exist two primary approaches to addressing bradycardia:
Medication:
In cases where bradycardia leads to significant issues, like dangerously low blood pressure, intravenous or injectable medications, such as atropine, may be administered to stimulate a faster heart rate. Typically, these treatments are administered within a hospital setting to ensure close monitoring and additional care.
Oral medications can also be prescribed for daily use to enhance heart function, bolster the strength of heart contractions or increase heart rate.
Temporary Pacing:
Temporary pacing involves the utilization of a device with electrical contacts that attach to the skin of the chest. These contacts introduce a mild electrical current into the body, stimulating the heart to beat. This method is effective for individuals requiring short-term treatment due to the likelihood of needing a permanent pacemaker or experiencing transient bradycardia.
Permanent Pacemaker:
For many individuals with bradycardia, a permanent pacemaker is often the optimal solution. This is particularly effective for conditions like sick sinus syndrome, where the heart’s natural pacemaker cells function improperly.
While a permanent pacemaker cannot completely cure the condition, it serves as a long-term remedy that manages and prevents the issue from causing further complications. These pacemakers typically have a lifespan of several years, with some boasting batteries that last over a decade.
The process of receiving a permanent pacemaker involves a surgical procedure to implant the device. The pacemaker, which emits electrical pulses to stimulate heart muscle contractions, is placed in a small pouch beneath the skin. Wires, referred to as leads, are positioned and connected to different points in the heart.
Innovative Options:
In recent years, advancements have introduced leadless pacemakers for bradyarrhythmias. These devices can be implanted via a catheter-based procedure, bypassing the need for surgery. A catheter is inserted through a major blood vessel, directed to the heart, where the pacemaker is implanted. These compact devices, about the size of a large multivitamin pill, offer a quicker recovery period compared to surgery and allow patients to return home sooner.
What are the complications of bradycardia?
Delayed treatment of bradycardia increases the likelihood of complications. This underscores the significance of timely diagnosis and prompt intervention.
The potential side effects or complications stemming from medication administration are diverse, contingent upon the specific drugs prescribed and your existing medications. Your healthcare provider is the most qualified individual to address this concern, customizing their response to align with your unique situation, requirements, and circumstances.
How to manage symptoms of bradycardia?
Managing bradycardia is not advisable without the guidance of a healthcare professional. If you suspect you might be experiencing this condition, seeking assistance from a medical provider is crucial, and it’s advisable to do so sooner rather than later.
How soon after treatment will I feel better?
After undergoing treatment for bradycardia, you should typically experience an improvement in your condition as the treatment takes effect. Rapid-acting medications, particularly those administered intravenously, often yield prompt results. In the case of requiring a pacemaker, you can anticipate a swift alleviation of symptoms immediately following the surgery. As you progress through the recovery process, your overall well-being should noticeably improve.
The majority of individuals will experience a recovery period lasting a few weeks after undergoing a pacemaker implantation procedure. However, your healthcare provider possesses the most accurate insights to provide you with detailed expectations regarding your recovery timeline and what you can anticipate during this phase.
Physiotherapy Relevance
Physiotherapy interventions can lead to changes in blood pressure, a reduction in oxygen saturation, and the potential for arrhythmias, particularly bradycardia. Therefore, it is essential to conduct a comprehensive multisystem assessment before initiating any intervention. This assessment should evaluate the potential benefits, possible adverse effects, and overall patient stability, ensuring the safety and efficacy of the physiotherapy measures. Throughout the interventions and the subsequent recovery period, continuous monitoring of heart rate, blood pressure, and a 12-lead ECG is imperative.
Prevention of Bradycardia
How to prevent bradycardia?
For a significant portion of individuals, the prevention of bradycardia remains a challenge, particularly in cases where it stems from factors such as exceptional physical fitness or the natural aging process.
However, bradycardia can be proactively prevented under certain circumstances, including:
- Recreational drug use: Steering clear of recreational drugs, especially illicit substances like narcotics and cannabis-derived products that lack medical prescription, can significantly reduce the likelihood of developing bradycardia.
- Infections: Swiftly addressing infections, even seemingly minor ones, can play a pivotal role in averting potential long-term heart complications.
- Anorexia nervosa: Needing a suitable cure for anorexia nervosa can contribute to the prevention of continuing problems for example bradycardia.
In most other scenarios, the occurrence of bradycardia remains unforeseeable. Its unpredictability makes prevention challenging. Despite proactive measures, aging can still lead to bradycardia in many cases, irrespective of efforts aimed at mitigating the risk.
Prognosis of Bradycardia
What can I expect if I have Bradycardia?
For a significant portion of individuals, bradycardia operates silently, devoid of symptoms, and without causing concern. This is particularly applicable to those who experience bradycardia due to their robust physical fitness.
However, for those who encounter symptoms or complications stemming from bradycardia, swift diagnosis, and intervention can lead to favorable outcomes. Timely treatment becomes pivotal, as delays in addressing the condition, especially when it arises from specific underlying conditions, tend to elevate the risk of complications or even mortality.
How long does bradycardia last?
Bradycardia’s duration can vary widely, spanning from a transient issue to a lifelong concern. The duration is predominantly determined by the underlying cause. Bradycardia often assumes a temporary nature when linked to drug use, whether prescription or recreational or when associated with other short-term conditions.
Ultimately, your healthcare provider possesses the expertise to offer insights into whether bradycardia will be a fleeting episode or a long-term challenge. Instances where persistent symptoms align with a lifelong presence of bradycardia often necessitate daily medication or pacemaker implantation through surgical intervention to manage the condition effectively.
Living with Bradycardia
How do I take care of myself?
If you’re experiencing bradycardia along with symptoms, consider the following steps:
- Consult your healthcare provider for assistance: Engaging with your healthcare provider is crucial to receive tailored guidance on self-care strategies.
- Adhere to your medication regimen: If you’re prescribed medication for bradycardia, ensure you follow the prescribed dosage and schedule. Don’t hesitate to seek clarification from your doctor if you have any uncertainties about your medication.
- Maintain recommended appointments: Regularly visit your healthcare provider as advised or as needed. If you have asymptomatic bradycardia, adhering to scheduled check-ups aids in the early detection of potential issues.
When should I see a doctor?
Regular healthcare check-ups are essential, irrespective of whether you’re dealing with bradycardia or not. A yearly visit to your healthcare provider for an annual physical is a crucial practice. This routine examination serves as a valuable opportunity for your healthcare provider to identify a spectrum of potential health issues early on, even those that might not manifest noticeable symptoms.
In the case of bradycardia without accompanying symptoms, maintaining regular medical visits is vital. If you detect any novel symptoms or experience shifts in your overall well-being, promptly consult your healthcare provider. Similarly, if you’re contending with symptoms related to bradycardia and they undergo changes, especially ones affecting your daily routines, seeking medical attention is advisable.
When should I go to the hospital?
If you experience a swift onset of bradycardia symptoms or notice a sudden worsening or alteration in your symptoms, it is advisable to seek immediate medical attention at a hospital.
Furthermore, you should not hesitate to head to the hospital promptly if you encounter any of the subsequent symptoms, which can also be indicative of more critical conditions such as a heart attack:
- Chest pain or discomfort (angina).
- Difficulty breathing or shortness of breath (dyspnea).
- Feelings of dizziness, lightheadedness, or fainting (syncope).
Conclusion
Bradycardia represents a frequent clinical observation, stemming from either physiological responses or underlying pathological states such as sinus node dysfunction and AV conduction issues. The management of unstable or symptomatic bradyarrhythmia often involves the administration of medications and pacing techniques.
FAQ
What is the main reason for bradycardia?
Bradycardia is usual for a few individuals, specifically if you are too fit. Regardless, it can even be induced by impairment of the heart because of aging/heart diseases (for example heart attack), cardiomyopathy, and myocarditis.
Is bradycardia a serious problem?
The hearts of adults at rest generally beat between 60 to 100 times per minute. If you undergo bradycardia, your heart beats lower than 60 times per minute. Bradycardia can be a severe difficulty if the heart rate is extremely slow & the heart can not pump adequately oxygenated blood to the body.
What are some symptoms of bradycardia?
The major symptom of bradycardia is a heart rate lower than 60 beats/minute. This abnormally down heart rate can affect the brain & other organs to evolve oxygen-underprivileged, which can cause symptoms for example Fainting and Dizziness.
Can bradycardia be cured?
For those who undergo symptoms, bradycardia is nearly consistently treatable & occasionally repairable. If you have bradycardia due to other medical circumstances, sometimes regaling that situation is all it brings to prevent your bradycardia.
What is the diet for bradycardia?
If it’s induced by heart drugs, he/she will accommodate your drugs. Assemble lifestyle modifications to enhance your heart health. Consume a heart-healthy diet that contains vegetables, fruits, nuts, beans, lean meat, fish, & whole grains. Limit alcohol, sodium, & sugar.