Chronic Pain Syndrome
What is Chronic Pain Syndrome?
Pain in your body is a normal response to an injury or illness, a sign that something is incorrect. When your body recovers, you generally stop hurting.
But for many people, pain continues to remain in the body after its reason is gone. When it stays for 3 to 6 months or more, it’s known as chronic pain. When you hurt day after day, it can also affect on your emotional well-being and physical fitness.
Approximately 25% of patients with chronic pain lead to a condition known as chronic pain syndrome (CPS). That’s when a person has symptoms beyond pain independently, such as depression and anxiety, which interrupt their daily lives.
CPS can be hard to manage, but it’s not unbelievable. A mix of therapies such as physical therapy, counseling, and relaxation methods can assist to ease your pain and the further symptoms that arrive with it.
Triggers
A mixture of health diseases can activate chronic pain syndrome. These contain, but are not limited to, the following examples:
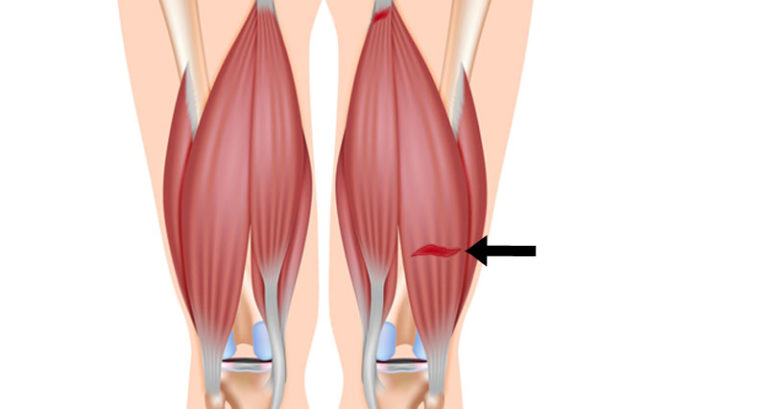
Musculoskeletal conditions: Arthritis, fibromyalgia, disk herniation, polymyalgia rheumatica, Lyme Disease, piriformis syndrome, chronic overuse injuries
Neurological conditions: Cervical radiculopathy, neuralgias, spinal stenosis, muscle tension headaches, migraines, temporomandibular joint dysfunction
Urological conditions: Interstitial cystitis, urolithiasis, prostatitis,
Gastrointestinal conditions: Gastroesophageal reflux, colitis, pancreatitis
Reproductive conditions: Endometriosis, adenomyosis
Psychological disorders: Depression, sleep disturbances, bipolar
Further health conditions: Cardiovascular condition, postoperative difficulties, cancer treatment difficulties
Symptoms of Chronic Pain Syndrome
CPS involves your physical fitness, your emotions, and your social life over time. The pain can conduct to further symptoms, like:
- Anxiety
- Depression
- Poor sleep
- Feeling very tired or wiped out
- Irritability
- Guilt
- Loss of interest in sex
- Drug or alcohol abuse
- Marriage or family problems
- Job loss
- Suicidal thoughts
Some patient with CPS requires to bring more and more drugs to manage their pain, which can create them dependent on these medicines.
Causes of chronic pain syndrome
Diseases that cause overall and long-lasting pain are, not surprisingly, frequently connected to chronic pain syndrome. Some of these conditions contain:
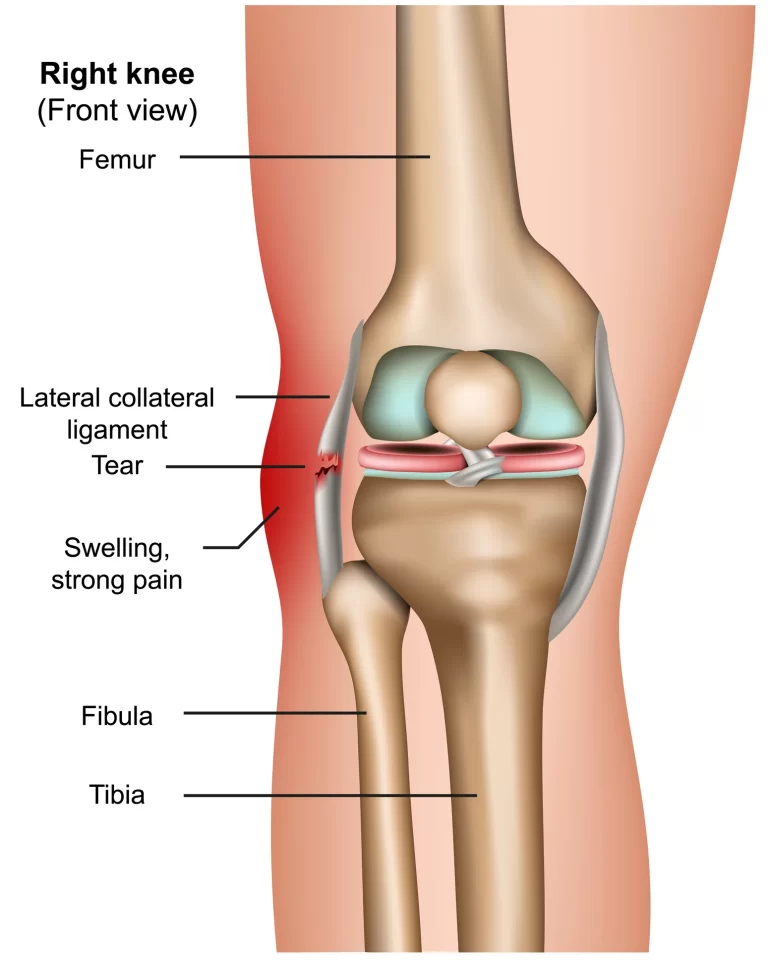
Osteoarthritis. This variety of arthritis is commonly the outcome of wear and tear on the body and happens when the defensive cartilage between bones wears away.
Rheumatoid arthritis. This is an autoimmune condition that generates painful inflammation in the joints.
Back pain. This pain may stem from nerve compression, muscle strains, or arthritis of the spine (known as spinal stenosis).
Fibromyalgia. This is a neurological disease that generates pain and tenderness in different regions of the body (called trigger points).
Inflammatory bowel disease. This disease generates chronic inflammation of the digestive tract and can produce intestinal pain and cramping.
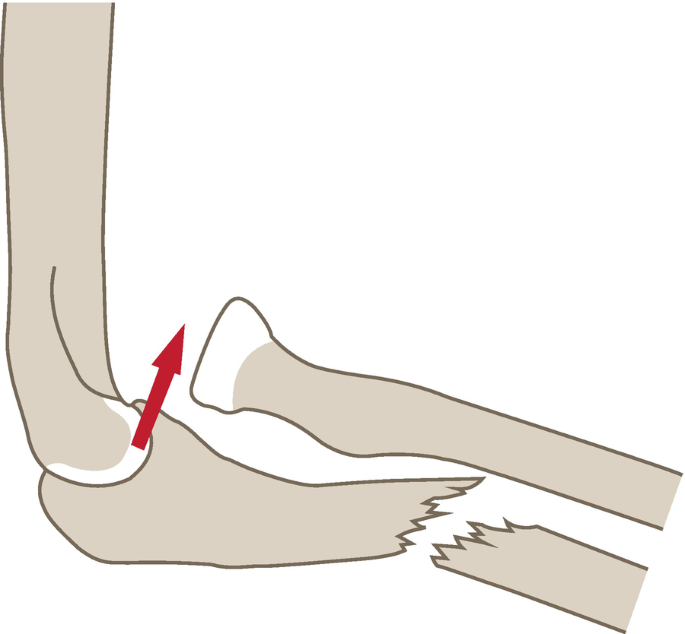
Surgical trauma.
Advanced cancer.
Even when these conditions enhance (through drugs or therapies), some patients can still feel chronic pain. This variety of pain is commonly caused by miscommunication between the brain and nervous system. (For unexplained causes, some patients can encounter this type of pain without any known triggers.)
Chronic pain can alter the way neurons (nerve cells in the brain that transmit and process sensory input) act, creating them hypersensitive to pain messages. For instance, according to the Arthritis Foundation, 20 percent of a patient with osteoarthritis who obtain their knees replaced (and probably have no more painful joint issues) will still document chronic pain.
Risk factors
Investigation indicates that some patients are more exposed to chronic pain syndrome than others. They are:
Those with chronic and painful diseases, like arthritis.
Those who are depressed. Specialists aren’t just certain why this is, but one idea is that depression alters the way the brain accepts and analyzes messages from the nervous system.
Those who smoke. As of yet, there are no final answers, but specialists are investigating why smoking appears to make the pain more harmful in those with arthritis, fibromyalgia, and further chronic pain conditions. According to the Cleveland Clinic, smokers make up 50 % percent of those who pursue therapy for ache relief.
Those who are obese. According to analysis, 50 percent of those who pursue therapy for obesity notice mild to severe pain. Specialists aren’t sure if this is due to the stress extra weight places on the body or if it’s due to the complicated way obesity interplays with the body’s hormones and metabolism.
Those who are female. Females tend to have more sensitivity to pain as compared to males. Investigators theorize that may be due to hormones or dissimilarities in the density of woman versus mannish nerve fibers.
Those who are more senior than 65. As you age, you’re more facedown with all types of diseases that can create chronic pain.
Differential Diagnosis
Chronic pain can be mistaken for recurrent attacks of acute pain which could herald a larger condition process. A person should be considered for autoimmune diseases and oncological procedures via a complete study of systems. Various diseases can cause chronic pain, involving those that conduct to nerve pain. Some of these contain:
- Central pain syndrome (CPS)
- Complex regional pain syndrome (CRPS)
- Trigeminal neuralgia
- Phantom limb pain
- Post-herpetic neuralgia (PHN)
Diagnosis
Your doctor will question you regarding any illnesses or injuries that might have begun the pain. They will also ask different questions to learn more regarding the variety of pain you experience and how long you’ve had it:
When did the pain begin?
Where on your body does it injure?
What does the pain sense like? Is it pounding, throbbing, sharp, shooting, stinging, pinching, burning, etc.?
How extreme is your pain on a scale of 1 to 10?
What appears to set off the pain or make it more harmful?
Have any therapies reduced it?
Imaging examinations can display whether you have a joint injury or other issues that cause pain:
CT, or computed tomography. It’s a strong X-ray that makes precise images inside your body.
MRI, or magnetic resonance imaging. It utilizes magnets and radio waves to create images of organs and structures inside you.
X-ray. It utilizes radiation in low doses to create pictures of structures in your body.
Treatments for Chronic Pain Syndrome
To manage your pain, you can see:
Your primary care doctor or physician
A professional for the medical disease that’s causing your pain – for instance, a rheumatologist to manage arthritis
A pain clinic or center
Your doctor will tailor your treatment to the origin of your pain. You might bring one or more of these therapies:
- Physical therapy
- Counseling, one-on-one, or group therapy
- Braces
- Relaxation methods like deep breathing or meditation
- Biofeedback
- Spinal cord stimulation
- Nerve blocks
- Pain medicines like antidepressants, NSAIDs, anti-seizure medicines, and muscle relaxants
- Surgery to manage the disease that generated the pain
Alternative
Acupuncture. According to an investigation of analyses, acupuncture decreased pain levels in 50 percent of those who tested it, corresponding with a 30 percent pain decrease in those who did not accept acupuncture.
Hypnosis. The analysis says that 71 percent of topics with irritable bowel syndrome (IBS) documented much-improved symptoms after a period of hypnosis. These outcomes extended up to five years post-therapy.
Yoga. Because it assists to encourages deep, relaxed muscles, and restorative breathing and raises mindfulness, analysis indicates that yoga can be useful in decreasing the depression and anxiety that arrives with chronic pain, thus enhancing your quality of life.
Physiotherapy treatment for Chronic Pain Syndrome
Physiotherapist mostly uses Pain relieving Electrotherapy modalities such as Interferential therapy(IFT), Transcutaneous electrical nerve stimulation (TENS), Ultrasound therapy, Short wave Diathermy, Wax bath, and Contrast Bath. These modalities are useful to relieve pain and related symptoms. Massage and other relaxation techniques with a combination of Yoga are helpful to some extent.
Exercise is a familiar therapy for chronic pain. Relying on your current condition of health, may assist in the reduction of inflammation, raise mobility, and reduce overall pain levels, no additional drug is needed.
Attempt a mixture of the relaxation technique with cardio, stretching, and strength exercises describe below and you may experience some of your pain relief away over time.
Cardio exercises
Cardiovascular activity has several physical and mental uses and can be especially useful for a patient with chronic pain. Cardio can be accomplished any time of day and frequently needs little or no equipment. Attempt these two exercises.
Walking
Walking 30 minutes 3 to 5 times per week can assist to gain strength, endurance, and heart fitness. If walking is challenging for you, begin gradually and work your way up to longer walks as you obtain stronger. If you utilize a walker or a cane, make certain to bring it with you.
Swimming and water aerobics
This is a perfect alternative to walking for a patient with mobility problems. This low-impact cardiovascular exercise can assist maintain your movement without placing added stress on your joints and muscles. Swimming can frequently be therapeutic, and it’s a significant way to clear your mind.
Relaxation exercise
Relaxation exercises are essential for many patients who live with chronic pain. Visualization needs no tools and can be done anywhere.
Deep breathing and visualization
Lie on your back in a supine position or another relaxed position on the bed or bottom.
Put your hands on your belly and rest your shoulders and feet.
Close your eyes and bring a deep breath in via your nose. Exhale via your
mouth, being certain to dismiss all of the air.
Continue breathing in via your nose and out via your mouth, feeling your belly
rise beneath your fingertips with per breath.
Continue this way and imagine pain going through your body with every breath.
Reprise every evening before bed or throughout the day as required.
Stretching exercises
If you keep chronic pain in your low back or neck, stretching can ease tension and stiffness. Attempt these equipment-free stretches for the back and neck to enhance general mobility and promote appropriate motion.
Low back stretch and glute stretch
Lie on your back in a supine position on the bottom.
Obtain your knees towards your chest, then cover your arms near your knees and provide yourself with a delicate hug.
Rock side to side, sensing a stretch via your hips and low back.
Attempt crossing one leg over the further for an added glute and piriformis stretch.
Levator scapula stretch and neck stretch
Stand or sit beside an entrance.
Lift your elbow beyond the shoulder on the side you like to stretch.
Relax your elbow against the door blockage. This will turn the outside of the shoulder edge up.
Following, bend your head out from that side and obtain your head to look down.
Slightly deepen the stretch by putting your free hand on the shelter of your head and using little pressure.
Strengthening exercises
Building strength is essential for stabilizing the joints and controlling coming injuries.
For a patient living with chronic pain, good core strength is particularly essential. It assists you to keep good posture and balance and decreases the chance of injuries that could guide to more pain.
Performing the muscles of the hips, abdomen, and back can assist to enhance core strength and stability. Attempt the exercises below.
Dead bug
Start by lying on your back in a supine position with your arms stretched above you, like you’re reaching for the roof.
Raise your feet into the air and flex your knees to 90 degrees. Commit your core by resting your ribcage and pulling your belly button down towards the bottom.
Exhale, then stretch your left leg down toward the bottom without letting it touch. At the same time, stretch your right arm toward the bottom above your head.
Maintain this position for 1 second. Return to the beginning position.
Reprise on the further side. Do 10 recurrences per side.
Begin by kneeling on all fours with your wrists beneath your shoulders and knees beneath your hips.
Make a flat back. Pull your shoulder edges down your back and engage your core by drawing your belly button up towards your spine. Accomplish not to allow your back arch throughout this motion.
Stretch one leg straight out after you. Lower the leg, dab your toe on the bottom, then raise.
Accomplish not raising the leg beyond hip level. Recount 10 times, maintaining your core activated throughout the activity and moving nobody but your leg.
Reprise on the further side.
You can raise the intensity of this activity by kneeling on a little stability
ball or foam roller.

Warnings
Always confer with your doctor before beginning an exercise schedule. Precise activities may alter relying on the origin of your chronic pain. It’s always most useful to confer with a physical therapist for a personalized activity routine. Specific diseases, like fibromyalgia, may lead to raised pain with activity, so begin gradually and monitor your symptoms.
Prognosis
The result of a person with CNCP is greatly influenced by the person’s capability to manage and self-regulate as pain and its next impact happen at the level of the higher cortical centers that are favorably contextualized and established on the person’s previous experiences.
FAQ
Is chronic pain syndrome a real thing?
Approximately 25% of people with chronic pain will go on to have a disease known as chronic pain syndrome (CPS). That’s when a person has symptoms above pain independently, such as depression and anxiety, which interrupt their daily lives. CPS can be difficult to manage, but it’s not unthinkable.
Is chronic pain syndrome curable?
There’s no known treatment for complex regional pain syndrome (CRPS), but a mixture of physical therapies, drugs, and psychological help can assist to control the symptoms. It’s calculated approximately 85% of people with CRPS gradually feel a decrease in their pain and some of their symptoms in the first 2 years.
Can you live a prolonged life with chronic pain?
The idea of living well while living with chronic pain can say unthinkable, but you can succeed despite chronic pain. Living well with your chronic pain isn’t only regarding managing your pain, but instead regarding finding methods to live a joyful, fulfilled life despite your symptoms.
Is chronic pain syndrome a disease?
This is an autoimmune condition that generates painful inflammation in the joints. Back pain. This pain may arise from nerve compression, muscle strains, or arthritis of the spine (known as spinal stenosis).
How long does chronic pain syndrome last?
Chronic or persistent pain is pain that takes on for longer than 12 weeks despite drug or treatment. Most patients get back to normal after pain following damage or operation. But occasionally the pain brings on for longer or arrives on without any record of an injury or operation.


5 Comments