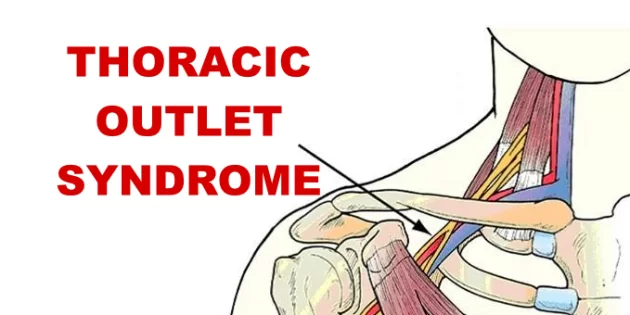
Thoracic outlet syndrome and physiotherapy management :
Thoracic outlet syndrome is a disorder in which neurovascular structures (blood vessels or nerves ) are compressed at the exit of the thoracic outlet (cervicothoracobrachial region).
- The thoracic outlet is marked by the anterior scalene muscle anteriorly, the middle scalene posteriorly, and the first rib inferiorly.
Relevant Anatomy :
- The first narrowing area is the most proximal and is named the interscalene triangle: This triangle is bordered by the anterior scalene muscle anteriorly, the middle scalene muscle posteriorly, and the medial surface of the first rib inferiorly.
- The presence of the scalene minimus muscle and the fact that both the anterior and middle scalene muscles have their insertion in the first rib (which can cause overlapping) can cause a narrow space and therefore compression. The brachial plexus and the subclavian artery pass through this space.
- The second passageway is called the costoclavicular triangle which is bordered anteriorly by the middle third of the clavicle, posteromedially by the first rib, and posterolaterally by the upper border of the scapula.
- The subclavian vein, artery, and plexus brachialis crosses this costoclavicular region and then further enters the subcoracoïd space. Just distal to the inter scalene triangle.
- Compression of these structures can occur as a result of congenital abnormalities, trauma to the first rib or clavicle, and structural changes in the subclavian muscle or the costocoracoid ligament.
- The last passageway is called the subcoracoid or sub-pectoralis minor space: This last passageway is beneath the coracoid process just under the pectoralis minor tendon. The borders of the thoraco-coraco-pectoral space include the coracoid process superiorly, the pec minor anteriorly, and ribs 2-4 posteriorly.
- Shortening of the Pectoralis Major can lead to a narrowing of this last space and therefore compression of the neurovascular structures during hyperabduction.
- Certain anatomical abnormalities can be potentially compromising to the thoracic outlet as well. These include the presence of a cervical rib, congenital soft tissue abnormalities, clavicular hypomobility , and functionally acquired anatomical changes.
- Soft tissue abnormalities may create compression or tension loading of the neurovascular structures found within the thoracic outlet (such as hypertrophy , a broader middle scalene attachment on the 1st rib or fibrous bands that increase the stiffness,…).
- There are several factors which can cause TOS: Cervical ribs are present in approximately 0.5-0.6% of the population, 50-80% of which are bilateral, and 10-20% produce symptoms; the female to male ratio is 2:1.
- Cervical ribs and the fibromuscular bands connected to them are the cause of most neural compression. Fibrous bands are a more common cause of TOS than rib anomalies.
Cause :
Congenital Factors:
- Cervical rib
- Prolonged transverse process
- Anomalous muscles
- Fibrous anomalies (transversocostal, costocostal)
- Abnormalities of the insertion of the scalene muscles
- Fibrous muscular bands
- Exostosis of the first rib
- Cervicodorsal scoliosis
- Congenital uni- or bilateral elevated scapula
- Location of the A. or V. Subclavian in relation to the M. scalene anterior
Acquired Factors :
- Poor posture: Drooping your shoulders or holding your head in a forward position can cause compression in the thoracic outlet area.
- Trauma: A traumatic event, eg. car accident, can cause internal changes that then compress the nerves in the thoracic outlet. The onset of symptoms related to a traumatic accident often is delayed.
- Overuse of Shoulder Girdle joints: Overuse of Shoulder Girdle can, over time, wear on your body’s tissue. Patient may seen symptoms of thoracic outlet syndrome if anyone have job requires to do repeat a movement continuously, eg. typing on a computer, working on an assembly line or lifting things above your head, as you would if you were stocking shelves. Athletes, such as baseball pitchers and swimmers, also can develop gradually thoracic outlet syndrome from years of repetitive movements.
- Obesity can increase an undue amount of stress on your joints, reducing joint space eg.Person can carrying around an oversized bag or backpack with belt passed through over the shoulder joint may reducing space and seen symptoms.
- Pregnancy: During Pregnancy joints become loosen and Obesity is also associated, This may reduce space and seen signs/Symptoms of thoracic outlet syndrome may first appear while you’re pregnant.
Types of TOS :
There are 3 Main types of thoracic outlet syndrome, as per following :
- Neurological thoracic outlet syndrome : This is the most common type of thoracic outlet syndrome in which brachial plexus are compressed. The brachial plexus come from spinal cord and control muscle movements and sensation in shoulder, arm and hand. Brachial Plexus Injury related sign and Symptoms are seen on affected side of Upper limb.
- Vascular thoracic outlet syndrome : This type of thoracic outlet syndrome occurs when one or more of the veins (venous thoracic outlet syndrome) or arteries (arterial thoracic outlet syndrome) are compressed in Thoracic outlet space. This may created sypmtoms according to compression.
- Nonspecific-type thoracic outlet syndrome : This type is rarely seen, is also called idiopathic thoracic outlet syndrome. There is a discussion in medical researcher that whether it exist or not. People with nonspecific-type thoracic outlet syndrome have chronic pain in the area of the thoracic outlet that worsens with activity, but a specific cause of the pain can’t be determined.
Sign and Symptoms of TOS :

- Signs and symptoms of thoracic outlet syndrome vary from patient to patient due to the location of the nerve and/or vessel involvement. Symptoms range from mild pain and sensory changes to limb-threatening complications in severe cases.
- Patients with thoracic outlet syndrome will most likely present pain anywhere between the neck, face, and occipital region or into the chest, shoulder, and upper extremity and paresthesia in the upper extremity.
- The patient may also complain of altered or absent sensation, weakness, fatigue, a feeling of heaviness in the arm and hand. The skin can also be blotchy or discolored. A different temperature can also be observed.
- Signs and symptoms are typically worse when the arm is abducted overhead and externally rotated with the head rotated to the same or the opposite side. As a result activities such as overhead throwing, serving a tennis ball, painting a ceiling, driving, or typing may exacerbate symptoms.
- When the upper plexus (C5,6,7) is involved there is pain in the side of the neck and this pain may radiate to the ear and face. Often the pain radiates from the ear posteriorly to the rhomboids and anteriorly over the clavicle and pectoralis regions.
- The pain may move laterally down the radial nerve area. Headaches are not uncommon when the upper plexus is involved.
Common Symptoms in Neurological TOS :
Thoracic outlet syndrome symptoms can vary, depending on which parts are compressed. When nerves are compressed, signs and symptoms of neurological thoracic outlet syndrome are as per below :
- Muscle Weaknes and wasting in the hypothenar area (Gilliatt-Sumner hand)
- Tingling Numbness, Parasthesia in patient arm or fingers
- Pain,spasm of muscle around neck, shoulder or hand
- Weakening grip
- Occipital Headache
- Loss of fine motor skills
Common Symptoms in Vascular TOS :
Signs and symptoms of vascular thoracic outlet syndrome are as per following :
- Discoloration of your hand (bluish color)
- Arm pain and swelling, possibly due to blood clots
- Blood clot in veins or arteries in the upper area of patient body
- Cold intolerance
- Lack of color (pallor) in one or more of patient fingers or patient entire hand
- Weak or no pulse in the affected arm
- Feeling of heaviness
- Cold fingers, hands or arms
- Arm fatigue with activity
- Numbness or tingling in patient fingers
- Weakness of arm or neck
- Throbbing lump near your clavicle
- Claudication
- Cyanosis
- Paresthesias
How Diagnosis is done in TOS ?
- The diagnosis of TOS is essentially based on history, physical examination, provocative tests, and if needed ultrasound, radiological evaluation, and electrodiagnostic evaluation.
- It must always keep in mind that TOS diagnosis is usually confirmed by the elimination of other causes with similar clinical presentations. Especially differential diagnosis of cervical radiculopathies and upper extremity entrapment neuropathies can be hard.
- In order to diagnose accurately, the clinical presentation must be evaluated as either neurogenic (compression of the brachial plexus) or vascular (compression of the subclavian vessels).
- TOS manifestations are varied and there is no single definitive test, which makes it difficult to diagnose.
- Patients with lower plexus (C8,T1) involvement typically have symptoms which are present in the anterior and posterior shoulder region and radiate down the ulnar side of the forearm into the hand, the ring and small fingers.
- There are four categories of thoracic outlet syndrome and each presents with unique signs and symptoms. Typically TOS does not follow a dermatomal or myotomal pattern unless there is nerve root involvement, which will be important in determining your PT diagnosis and planning your treatment.
Examination
- The following includes common examination findings seen with TOS that should be evaluated; however, this is not an all-inclusive list and examination should be individualized to the patient.
- Electrodiagnostic evaluation and imaging :
- Nerve conduction studies and electromyography are often helpful as components of the diagnostic evaluation of patients with suspected TOS.
- Nerve conduction studies usually reveal decreased ulnar sensorial potentials, decreased median action potentials, normal or close to the normal ulnar motor, and median sensorial potentials. Vascular TOS can be identified with venography and arteriography.
- Besides the electrophysiological studies, imaging studies can provide useful information in the diagnosis of TOS. Cervical spine and chest x-rays are important in the identification of bony abnormalities (such as cervical ribs or a “peaked C7 transverse processes)
History
Make sure to take a thorough history, clear any red flags, and ask the patient how signs/symptoms have affected his/her function.
- Type of symptoms
- Location and amplitude of symptoms
- Irritability of symptoms
- Onset and development over time
- Aggravating/alleviating factors
- Disability
- Physical Examination :
- Observation
- Posture
- Cyanosis
- Edema
- Paleness
- Atrophy
- Palpation
- Temperature changes
- Supraclavicular fossa
- Scalene muscles (tenderness)
- Trapezius muscle (tenderness)
- Neurological Screen
- MMT & Flexibility of the following muscles:
- Scalene
- Pectoralis major/minor
- Levator scapulae
- Sternocleidomastoid
- Serratus anterior
Special Tests :
- Elevated Arm Stress/ Roos test: the patient has arms at 90° abduction and the therapist puts downwards pressure on the scapula as the patient opens and closes the fingers. If the TOS symptoms are reproduced within 90 seconds, the test is positive.
- Adson’s: the patient is asked to rotate the head and elevate the chin toward the affected side. If the radial pulse on the side is absent or decreased then the test is positive, showing the vascular component of the neurovascular bundle is compressed by the scalene muscle or cervical rib.
- Wright’s: the patient’s arm is hyper abducted. If there is a decrease or absence of a pulse on one side then the test is positive, showing the axillary artery is compressed by the pectoralis minor muscle or coracoid process due to stretching of the neurovascular bundle.
- Cyriax Release: the patient is seated or standing. The examiner stands behind patient and grasps under the forearms, holding the elbows at 80 degrees of flexion with the forearms and wrists in neutral. The examiner leans the patient’s trunk posteriorly and passively elevated the shoulder girdle. This position is held for up to 3 minutes. The test is positive when paresthesia and/or numbness (release phenomenon) occurs, including reproduction of symptoms.
- Supraclavicular Pressure: the patient is seated with the arms at the side. The examiner places his fingers on the upper trapezius and thumb on the anterior scalene muscle near the first rib. Then the examiner squeezes the fingers and thumb together for 30 seconds. If there is a reproduction of pain or paresthesia the test is positive, this addresses compromise to brachial plexus through scalene triangles.
- Costoclavicular Maneuver: this test may be used for both neurological and vascular compromise. The patient brings his shoulders posteriorly and hyperflexes his chin. A decrease in symptoms means that the test is positive and that the neurogenic component of the neurovascular bundle is compressed.
- Upper Limb Tension: These tests are designed to put stress on the neurological structures of the upper limb. The shoulder, elbow, forearm, wrist, and fingers are kept in a specific position to put stress on a particular nerve (nerve bias) and further modification in the position of each joint is done as “sensitizer”.
- Cervical Rotation Lateral Flexion: The test is performed with the patient sitting. The cervical spine is passively and maximally rotated away from the side being tested. While maintaining this position, the spine is gently flexed as far as possible moving the ear toward the chest. A test is considered positive when the lateral flexion movement is blocked.
- Dropped shoulder condition
- Wrong work posture (standing or sitting without paying attention to the physiological curvature of the spine)
- Heavy mammaries
- Trauma
- Clavicle fracture
- Rib fracture
- A hyperextension neck injury, whiplash
- Repetitive stress injuries (repetitive injury most often form sitting at a keyboard for long hours)
- Muscular Causes:
- Hypertrophy of the scalene muscles
- Decrease of the tonus of the M. trapezius, M. levator scapulae, M.rhomboids
- Shortening of the scalene muscles, M. trapezius, M. levator scapulae, pectoral muscles
Medical Management
- Nonsteroidal anti-inflammatory drugs have been prescribed to reduce pain and inflammation. Botulinum injections to the anterior and middle scalenes have also found to temporarily reduce pain and spasm from neurovascular compression, further research is needed because there are discrepancies in the literature.
- Surgical management of TOS should only be considered after conservative treatment has been proven ineffective.
- However, limb-threatening complications of vascular TOS have been indicated for surgical intervention.
- Surgery to treat thoracic outlet syndrome may be performed using several different approaches, including transaxillary approach, supraclavicular approach, and infraclavicular approach.
- Transaxillary approach. The first rib forms the common denominator for all causes of nerve and artery compression in this region so that its removal generally improves symptoms. The surgeon makes an incision in the chest to access the first rib, divide the muscles in front of the rib and remove a portion of the first rib to relieve compression, without disturbing the nerves or blood vessels.
- The supraclavicular approach has been advocated to perform first rib resection and splenectomy, a safe and effective procedure, characterized by a shorter operative time and having a complication rate lower or comparable to that of transaxillary first rib resection.
- This approach repairs compressed blood vessels. The surgeon makes an incision just under the neck to expose the brachial plexus region. Then he looks for signs of trauma or muscles contributing to compression near the first rib. The first rib may be removed if necessary to relieve compression.
- Infraclavicular approach. In this approach, the surgeon makes an incision under the collarbone and across the chest. This procedure may be used to treat compressed veins that require extensive repair.
- Neurogenic TOS: Surgical decompression should be considered for those with true neurological signs or symptoms. These include weakness, wasting of the hand intrinsic muscles, and conduction velocity less than 60 m/sec.
- The first rib can be a major contributor to TOS. There is controversy, however, regarding the necessity of a complete resection to reduce the chance of reattachment of the scalenes, scar tissue development, or bony growth of the remaining tissue. In addition to the first rib, cervical ribs are removed, scalenectomies can be performed, and fibrous bands can be excised. Terzis found that the supraclavicular approach to treatment to be an effective and precise surgical method
- Arterial TOS: Decompression can include cervical and/or first rib removal and scalene muscle revision. The subclavian can then be inspected for degeneration, dilation, or aneurysm. Saphenous vein graft or synthetic prosthesis can then be used if necessary
- Venous TOS: Thrombolytic therapy is the first line of treatment for these patients. Because of the risk of recurrence, many recommend removal of the first rib is necessary even when thrombolytic therapy completely opened the vein. The results of a study show that infraclavicular approach is a safe and effective treatment for acute VTOS. They had no brachial plexus or phrenic nerve injuries.
- Angioplasty can then be used to treat those with venous stenosis
- In venous or arterial TOS, medication can be administered to dissolve blood clots prior to thoracic outlet compression. It may also be to conduct a procedure to remove a clot from the vein or artery or repair the vein or artery prior to thoracic outlet decompression.
- Some larger-chested women have sagging shoulders that increase pressure on the neurovascular structures in the thoracic outlet. A supportive bra with wide and posterior-crossing straps can help reduce tension. Extreme cases may resort to breast-reduction surgery to relieve TOS and other biomechanical problems.
Physiotherapy Management :
- Conservative management should be the first strategy to treat TOS since this seems to be effective at decreasing symptoms, facilitating return to work and improving function, but yet a few studies have evaluated the optimal exercise program as well as the difference between a conservative management and no treatment.
- Conservative management includes physical therapy, which focuses mainly on patient education, paincontrol, range of motion, nerve gliding techniques, strengthening and stretching.
Stage 1:
- The aim of the initial stage is to decrease the patient’s symptoms. This may be achieved by patient education, in which TOS, bad postures, the prognosis and the importance of therapy compliance are explained.
- Furthermore some patients who sleep with the arms in an overhead, abducted position should get some information about their sleeping posture to avoid waking up at night. These patients should sleep on their uninvolved side or in supine, potentially by pinning down the sleeves.
- The Cyriax release test may be used if a ‘release phenomenon’ is present. This technique completely unloads the neurovascular structures in the thoracic outlet before going to bed.
Cyriax Release Maneuver :
- Elbows flexed to 90°
- Towels create a passive shoulder girdle elevation
- Supported spine and the head in neutral
- The position is held until peripheral symptoms are produced. The patient is encouraged to allow symptoms to occur as long as can be tolerated up to 30 minutes, observing for a symptom decrescendo as time passes.
- The patient’s breathing techniques need to be evaluated as the scalenes and other accessory muscles often compensate to elevate the ribcage during inspiration.
- Encouraging diaphragmatic breathing will lessen the workload on already overused or tight scalenes and can possibly reduce symptoms.
Scapula Settings and Control
- In the treatment, you first have to start with scapula settings and control.
- This is important to establishing normal scapula muscle recruitment and control in the resting position. Once this is achieved then the program is progressed to maintaining scapula control while both motion and load are applied.
- The program begins in lower ranges of abduction and is gradually progressed further up into abduction and flexion range until muscles are being retrained in functional movement patterns at higher ranges of elevation.
Control the Humeral Head Position :
- It is also important to control the humeral head position. Specific drills are given to facilitate humeral head control. The most common aberrant position of the humeral head is an increase in anterior placement of the humeral head.
- A useful strategy to help facilitate co-contraction of the rotator cuff to help stabilize and centralize the humeral head is to facilitate a mid-level isometric contraction of the rotator cuff by applying resistance to the humeral head.
- Further on in the treatment, this may be integrated into movement patterns. First in slow controlled concentric/eccentric motion drills, later isolated muscle strengthening drills.
Serratus Anterior Recruitment and Control :
- Abduction external rotation strategies described above are often sufficient to trigger serratus anterior recruitment and control without the risk of over-activating pectoral minor muscle
Stage 2:
- Once the patient has control over his/her symptoms, the patient can move to this stage of treatment. The goal of this stage is to directly address the tissues that create structural limitations of motion and compression.
- How this should be done is one of the most discussed topics of this pathology. Some examples of methods that are used in the literature are.
Massage
- Strengthening of the levator scapulae, sternocleidomastoid and upper trapezius (This group of muscles open the thoracic outlet by raising the shoulder girdle and opening the costoclavicular space)
- Stretching of the pectoralis, lower trapezius and scalene muscles (These muscles close the thoracic outlet)
- Postural correction exercises
- Relaxation of shortened muscles
- Aerobic exercises in a daily home exercise program:
Exercises
- Shoulder exercises to restore the range of motion and so provide more space for the neurovascular structures.
- Exercise: Lift your shoulders backwards and up, flex your upper thoracic spine and move the shoulders forward and down. Then straightened the back and repeat 5 to 10 times.
- ROM of the upper cervical spine
- Exercise: Lower your chin 5 to 10 times against your chest, while you are standing with the back of your head against a wall. The effectiveness of this exercise can be enlarged by pressing the head down by hands.
- Activation of the scalene muscles are the most important exercises. These exercises help to normalize the function of the thoracic aperture as well as all the malfunctions of the first rib.
- Exercises are Anterior scalene (Press your forehead 5 times against the palm of your hand for a duration of 5 seconds, without creating any movement), Middle scalene (Press your head sidewards against your palm), Posterior scalene (Press your head backwards against your palm
- Stretching exercises
- Other Interventions
- Repositioning/mobilization of the shoulder girdle and pelvis joints: cervicothoracic, sternoclavicular, acromionclavicular, and costotransverse joints
- Glenohumeral mobilizations in end-range elevation with the elbow supported in extension
- Taping: some patients with severe symptoms respond to additional taping, adhesive bandages or braces that elevate or retract the shoulder girdle.
- Manipulative Treatment to Mobilize the First Rib
- These should be carried out with caution and only after a thorough assessment as they can provoke irritation and pain symptoms in some patients
Posterior Glenohumeral Glide with Arm Flexion:
- The patient is supine. The mobilizisation hand contacts the proximal humerus avoiding corocoid process. The force is directed posterolaterally (direction of thumb).
Anterior Glenohumeral Glide with Arm Scaption:
- The patient is prone. The mobilization hand contacts the proximal humerus avoiding acromion process. The force is directed anteromedially.
Inferior Glenohumeral Glide:
- The patient is prone. The stabilizing hand holds the proximal humerus the humerus distal to the lateral acromion process.
- The mobilization hand contacts the axillary border of the scapula. Mobilize the scapula in a craniomedial direction along the ribcage.






11 Comments