Diastematomyelia
What is Diastematomyelia?
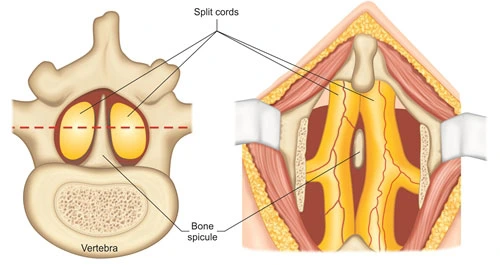
Diastematomyelia, also called a split cord malformation, leads to a variety of spinal dysraphism (spina bifida occulta) when there is a longitudinal separation in the spinal cord.
Women are involved much more generally than men. This disease happens in the presence of a cartilaginous, osseous, or fibrous septum in the central part of the spinal canal which then creates a complete or incomplete sagittal section of the spinal cord into two hemicords. When the separation does not reunite distally to the spur, the disease is guided to diplomyelia, which is a true replication of the spinal cord.
Epidemiology
Separated cord malformations are a hereditary abnormality and account for ~5% of all congenital spinal faults.
Symptoms of Diastematomyelia
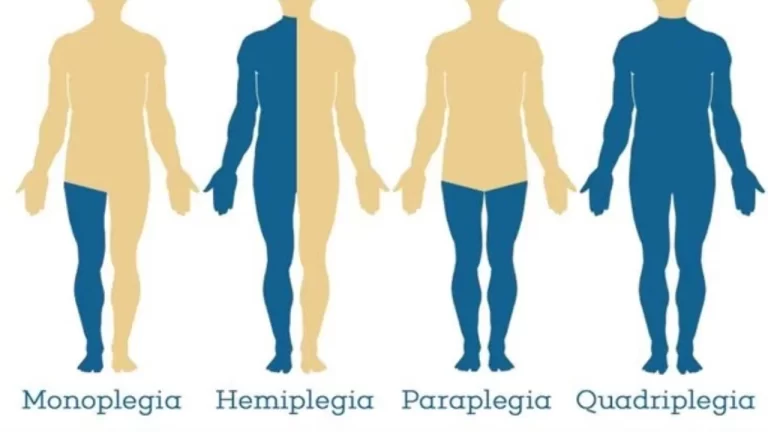
The prevalence of persons with diastematomyelia is symptomatic, demonstrating signs and symptoms of tethered cord, although a person with mild type II may be minimally involved or completely asymptomatic. Showing symptoms contain:
- leg weakness
- low back pain
- scoliosis
- Bladder – Bowel incontinence
Persons with diastematomyelia also often have further associated anomalies involving:
- meningocele
- neurenteric cyst
- dermoid cyst
- clubfoot
- spinal cord lipoma
- haemangioma overlying spine
Pathology
The disease is believed to happen during the gastrulation phase of development due to abnormal motion and the split of precursor cells. Particularly, it has been assumed that a persistent or abnormal adhesion between the ectoderm and endoderm forms an additional neurenteric canal which in turn conducts to the notochord evolving into two hemicords
Classification of Diastematomyelia
Split cord malformations are split into two varieties according to the presence of a dividing septum and single vs dual dural sac:
type I: duplicated dural sac, with typical midline spur (osseous or fibrous) and generally symptomatic
type II: single dural sac including both hemicords, impairment less significant
Type I
Type I is the classic diastematomyelia, represented by 1-6:
duplicated dural sac
hydromyelia- Common
midline spur frequently present (osseous or osteocartilaginous)
vertebral abnormalities- butterfly vertebrae, hemivertebrae, a fusion of laminae of adjacent levels, spina bifida,
haemangioma, skin pigmentation, and hypertrichosis (hair patch) are familiar
persons are generally symptomatic presenting with scoliosis and tethered cord syndrome
Type II
Type II is milder than type I, and lacks many of the characteristics of the latter:
single dural sac and no spur/septum
cord separated, occasionally incompletely so
hydromyelia may be present
spina bifida may be present, but further vertebral anomalies are far less familiar
a person is less symptomatic or may even be asymptomatic
Differential diagnosis
Generally, there is a small in the way of a differential diagnosis when the cord has been sufficiently imaged and characteristics are familiar (particularly now that diplomyelia is considered a region of the exact spectrum by many authors.
Diagnosis
Split cord malformations are more familiar in the lower cord but can occasionally happen at multiple levels.
50% happen between L1 and L3
25% happen between T7 and T12
An associated cartilaginous, bony, or fibrous spur projecting via the dura mater forwards from the neural arch is observable in 33% of patients.
Vertebral anomalies (butterfly, spina bifida, or hemivertebrae) are familiar. Laminar fusion associated with a neural arch defect is a fine predictor of diastematomyelia and happens at the level of the fault, or an adjoining level.
Antenatal ultrasound
The presence of additional echogenic stress in the midline between the fetal spinal posterior parts has been defined as a reliable sign.
Plain radiograph
- multilevel spina bifida
- broadening of interpedicular distance- but this may be hidden from the area of the spur
- associated scoliosis
- anteroposterior vertebral body narrowing
multilevel spina bifida
- broadening of interpedicular distance- but this may be hidden from the area of the spur
- associated scoliosis
- anteroposterior vertebral body narrowing
CT
CT scan nicely images many of the elements noticed on plain films and in extra may demonstrate the bony septum.
MRI
MRI is the modality of selection for evaluating kids with split cord malformations. As well as being capable of elegantly displaying the cord and presence of hydromyelia (if present), it can also evaluate for the presence of the multiple associated anomalies
Treatment of Diastematomyelia
Treatment is mostly symptomatic, if any symptoms are present, Doctors prescribe medicines according. If any deformity such as clubfoot, or scoliosis presents exercise under the guidance of a Physiotherapist is useful.
Surgery
Surgical intervention is required in persons who present with a new beginning of neurological signs and symptoms or have a record of progressive neurological representations that can be connected to this abnormality. The surgical method needed for the useful treatment of diastematomyelia contains decompression (surgery) of neural elements and subtraction of bony spur.
This may be performed with or without resection and fix of the repeated dural sacs. Resection and repair of the repeated dural sacs are selected since the dural abnormality may partially contribute to the tethering method liable for the symptoms of this disease.
Post-myelography CT scanning delivers individualized detailed maps that enable surgical therapy of cervical diastematomyelia, first conducted in 1983.
Observation
Observation
If Diastematomyelia is asymptomatic, there is no treatment is required. However, these kinds of patients should have regular neurological checkups since it is known that the condition can deteriorate anytime. If any symptoms worsen, then a resection surgery should be advised by Doctors.
FAQ
Is diastematomyelia the same as spina bifida?
Diastematomyelia, a variety of spina bifida, defines a congenital spinal dysraphism resulting in a split cord malformation. The spinal cord is longitudinally separated into two hemicords, covered by its dural tube and divided by a midline bony spur or cartilaginous or fibrous ridge or band.
What are the complications of diastematomyelia?
Generally, diastematomyelia generates numb sciatica, lumbago, or perianal dysesthesia in grown-ups. Few persons may have asymmetry in leg muscles, the buttocks, or gluteal folds
What is the prognosis of diastematomyelia?
When diastematomyelia is not associated with further spinal anomalies, the prediction is good. In seven of eight patients noted by Has et al.,106 faults had normal amniotic AFP and AChE levels and were believed isolated.
Is tethered cord curable?
The fine information is that tethered spinal cord is an extremely treatable disease, particularly when diagnosed and managed early. Surgery is the most familiar therapy to untether the spinal cord from the spinal tissue.
What is the difference between Type 1 and Type 2 diastematomyelia?
The type 1 deformity is represented by an extradural bony spur that delivers two different dural sacs with two arachnoid sacs per individual hemicord. This is the variety that generally delivers symptoms. Persons are said to have type 2 diastematomyelia if there is one dural sac covering the split cord.





One Comment