Spinal cord
What is the spinal cord?
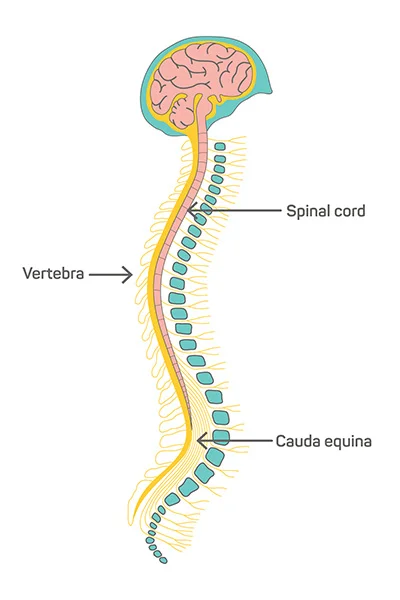
- The spinal cord is a long, tube-like band of tissue. It connects the brain to the lower back. the spinal cord carries nerve signals from the brain to the body & vice versa. These nerve signals help you feel sensations & move the body. Any injury or disease to the spinal cord can affect movement or function.
- Your spinal cord is a cylindrical structure that runs through the center of the spine, from the brainstem to the low back. It’s a delicate structure that contains nerve bundles & cells that carry messages from the brain to the rest of the body. Your spinal cord is one of the main parts of the nervous system.
What is the difference between the spinal cord & the vertebral column?
- People often refer to the spinal cord & vertebral column together as the spine. the spinal cord is a band of tissues, nerves & cells. A protective layer of bone called the vertebral column covers & protects the spinal cord.
- The bones in the vertebral column are called vertebrae (plural of one spine bone, a vertebra). the vertebrae stack on top of each other, from your pelvic bones to your skull. Between each pair of vertebrae, there is a spinal disc. Discs have a tough outer shell & a gel-like interior. They act as shock absorption & cushion for the vertebrae & spinal cord.
What is the purpose of the spinal cord?
- The spinal cord’s main purpose is to carry nerve signals throughout the body. These nerve messages have three crucial functions. They include Control of body movements & functions. Signals from the brain to other body parts control the movements. They also direct autonomic (involuntary) functions like the breathing rate & heartbeat, as well as bowel & bladder function.
- Report senses to your brain. Signals from other parts of the body help the brain record & process sensations like pressure or pain.
- Manage the reflexes. the spinal cord controls some reflexes (involuntary movements) without involving the brain. For example, the spinal cord manages the patellar reflex (involuntarily moving your leg when someone taps your shin in a certain spot).
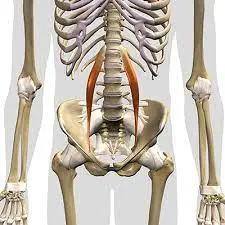
What are the main parts of the spinal cord?
The spinal cord has three main parts:
- Cervical (neck).
- Thoracic (chest).
- Lumbar (lower back).
- What tissues & fluids invent the spinal cord?
- Like the brain, layers of tissue called meninges cover the spinal cord. These protective tissues include:
Dura mater. The outer layer protects the spinal cord from injury.
Arachnoid mater. is The middle layer which presents between the epidural & subarachnoid space.
Pia mater. The inner layer covers your spinal cord.
What are the epidural & arachnoid spaces?
- The epidural space is present between the dura mater & arachnoid mater. This space is where medical care providers insert anesthesia during childbirth, known as epidurals.
- The subarachnoid space is present between the arachnoid mater & the pia mater. Here, cerebrospinal fluid (CSF) provides extra cushioning & protection for the spinal cord.
- Sometimes, providers need to insert a needle into the subarachnoid space to test CSF for definite infections. This procedure is called a spinal tap. Both the epidural & arachnoid spaces provide extra shock absorption for the spine.
What nerves are in the spinal cord?
You have 31 pairs of nerves & nerve roots in the spinal cord. These include:
- Eight cervical nerve pairs (nerves starting in the neck & running mostly to the face & head).
- Twelve thoracic nerve pairs (nerves in the upper body that extend to the chest, upper back & abdomen).
- Five lumbar nerve pairs (nerves in the low back that run to the legs & feet).
- Five sacral nerve pairs (nerves in the low back continue into the pelvis).
- You also have a nerve bundle at the base of the spinal cord called the cauda equina. The cauda equina comes from the Latin word for “horse’s tail,” because early anatomists thought the nerve collection looked like a horsetail. The cauda equina includes nerves that provide sensation to the lower body.
- the spinal nerves send electrical signals between the brain, spinal cord & the rest of the body. These electrical nerve signals help you feel sensations (sensory nerve) & move the body (motor nerves)
- The spinal cord begins at the bottom part of the brainstem, called the medulla oblongata. At the lower back, the spinal cord forms a cone shape called the conus medullaris
- In most adults, the spinal cord is about 18 inches (45 centimeters) long.
What conditions & disorders affect the spinal cord?
- Many disorders or injuries can affect the spinal cord. Spinal cord injuries & disorders are serious. Any injury to your spinal cord can cause severe symptoms in the parts of the body below the injury.
- Severe symptoms that can result from spinal cord damage can cause loss of bladder control or paralysis. For some disorders, getting treatment quickly can lower the risk of long-term or permanent symptoms.
- Acute transverse myelitis. Inflammation in one or more parts of the spinal cord.
- Cervical spondylosis. Progressive wear-& tear of the spinal disks in your neck (cervical disks) that can press on the spinal cord (cervical myelopathy).
- Herniated disks. when a spinal disk slips out of place & moves into the space around the spinal cord, pressing on nearby nerves.
- Spinal fractures. When one or more vertebrae are crushed (compression fracture) or broken (burst fracture) & put pressure on the spinal cord.
- Spinal muscular atrophy. A rare genetic condition where people lose motor nerve cells in the spinal cord, causing muscle weakness & atrophy (wasting away).
- Spinal stenosis. Narrowing of the spinal column, leading to pinched nerves & spinal cord irritation.
Common conditions that can affect the spinal cord include:
- Spinal tumors. Masses — which may be cancerous or not (benign) — that start in the spinal column & can put pressure on the spinal cord.
- Spinal infections. When the pressure of an expanding abscess or collapse of an infected vertebra or disc puts pressure on the spinal cord.
CARE
- Eat a nutritious diet with fruits, vegetables, whole grains, healthy fats & lean proteins.
- Exercise constantly, with a combination of aerobic activities, strengthening & stretching.
- Practice maintaining a good posture & avoid hunching while sitting or standing.
- Quit smoking & using other tobacco products.
- Sleep in positions that support the natural curve of your neck & lower back.
- Walk often & take breaks throughout the day.
- Limit alcohol use & avoid using recreational drugs
- You can keep your spinal cord, vertebral column & entire back healthier by practicing healthy habits.
Spinal cord injury
What is spinal cord injury?
- A spinal cord injury damage to any part of the spinal cord or nerves at the end of the spinal canal (cauda equina) also causes permanent changes in strength, and sensation & it can affect other body functions below the site of the injury.
- If you’ve recently injured the spinal cord, it might seem like every aspect of your life has been affected. You might feel the effects of the injury mentally, emotionally & socially.
- Many scientists are assured that advances in research will someday make the repair of spinal cord injuries possible. Research studies are ongoing around the world. In the meantime, treatments & rehabilitation allow many people with spinal cord injuries to lead productive, independent lives.
What are the Symptoms of spinal cord injury?
- The part of the body affected by paraplegia & quadriplegia
- Spinal cord injuries open a pop-up dialog box
- Your ability to control the limbs after a spinal cord injury depends on two factors: where the injury occurred on your spinal cord & the severity
The lowest part of your spinal cord that remains undamaged after an injury is referred to as the neurological level of the injury. The severity of the injury is also called “completeness” & is classified as either of the following:
- Complete. If all feeling (sensory) & all ability to control movement (motor function) are lost below the spinal cord injury, your injury is called complete.
Incomplete. If you have some motor or sensory function below the affected area, the injury is known as incomplete. There are individual degrees of incomplete injury
further, paralysis from a spinal cord injury can be referred to as: - Tetraplegia. Also known as quadriplegia, this means that your arms, hands, trunk, legs & pelvic organs are all affected by the spinal cord injury.
Paraplegia. This paralysis affects all or part of the trunk, legs & pelvic organs.
Your healthcare team will perform a series of tests to determine the neurological level & completeness of the injury.
Spinal cord injuries can cause one or more of the following signs & symptoms:
- Loss of movement
- Loss of or altered sensation, including the ability to feel heat, cold & touch
- Loss of bowel or bladder control
- Exaggerated reflex activities or spasms
- Swap in sexual function, sexual sensitivity & fertility
- Pain or an intense stinging sensation caused by the damage to the nerve fibers in the spinal cord
- Difficulty in breathing, coughing, and clearing secretions from the lungs
Emergency signs or symptoms
Emergency signs or symptoms of a spinal cord injury after an accident include:
- Extreme low back pain & pressure in the neck, head, & back
- Weakness, incoordination, and paralysis in any portion of the body
- Numbness, tingling, and loss of sensation in the hands, fingers, feet, or toes
- Loss of bladder or bowel control
- Difficulty with balance & walking
- Impaired breathing after injury
- An oddly positioned or twisted neck or back
When to visit a doctor?
- Anyone who has crucial trauma to the head or neck required immediate medical evaluation for a spinal injury. In fact, it’s safest to assume that trauma sufferers have a spinal injury until proven otherwise because:
- A serious spinal injury isn’t always immediately obvious. If it isn’t known, a more severe injury can occur.
Numbness & paralysis can be immediate or come on gradually.
The time between injury & treatment can be critical in determining the extent & severity of complications & the possible extent of expected recovery.
If you guess that someone has a back or neck injury:
Don’t move the injured person permanent paralysis & other serious complications can result
- Place heavy towels on both sides of the neck or hold the head & neck to prevent them from moving until emergency care arrives
- supply basic first aid, like stopping bleeding & making the person comfortable, without moving the head or neck
What are the causes of spinal cord injury?
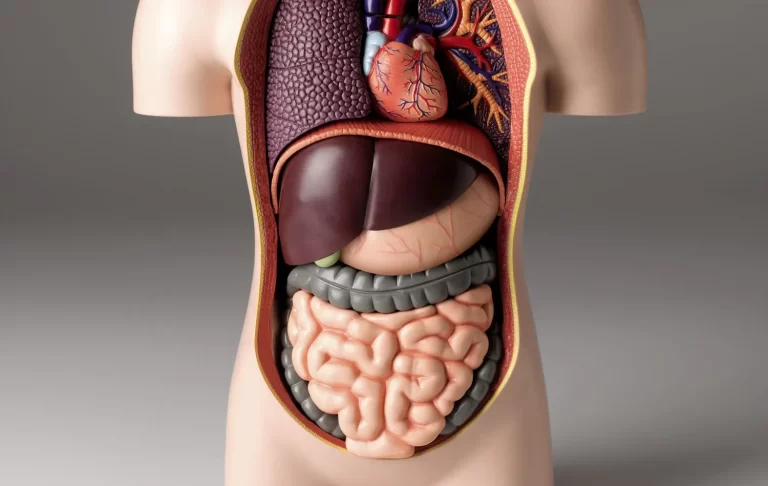
- The anatomy of the central nervous system.
- Spinal cord injuries can occur from damage to the vertebrae, ligaments & disks of the spinal column & the spinal cord itself.
- A traumatic spinal cord injury can stem from a sudden, traumatic blow to your spine that fractures, dislocates, crushes & compresses one or more of the vertebrae. It can also occur from a gunshot or knife wound that penetrates & cuts the spinal cord.
- Additional damage usually occurs over days or weeks because of bleeding, swelling, inflammation & fluid accumulation in & around the spinal cord.
- A nontraumatic spinal cord injury can be caused by arthritis, cancer, inflammation, infections & disc degeneration of the spine.
- Your brain & central nervous system
The central nervous system contains the brain & spinal cord. The spinal cord is made of soft tissue & surrounded by bones (vertebrae). It extends down from the base of your brain & contains nerve cells & groups of nerves called tracts, which go to different parts of the body. - The lower end of the spinal cord stops a little above the waist in the region called the conus medullaris. Below this region, there is a presence of a group of nerve roots called the cauda equina.
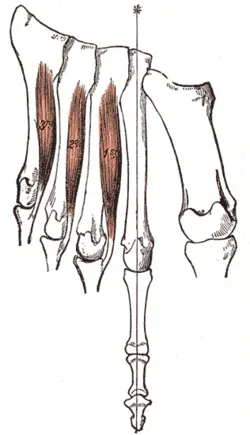
- Tracts in the spinal cord carry messages between the brain & the rest of the body. Motor tracts carry signals from the brain to maintain muscle movement. Sensory tracts carry signals from body parts to the brain relating to heat, cold, pressure, pain & the position of the limbs.
- Damage to nerve fibers
Whether the cause is traumatic or nontraumatic, the damage affects the nerve fibers passing through the injured area and can impair part of or all the muscles & nerves below the injury site. - A chest (thoracic) or lower back (lumbar) injury can affect the torso, legs, bowel & bladder control, & sexual function. A neck (cervical) injury affects the same areas in addition to affecting movements of the arms & possibly, your ability to breathe.
Common causes of spinal cord injuries
The most ordinary causes of spinal cord injuries in the United States are:
- Motor vehicle accidents. Auto & motorcycle accidents are the leading cause of spinal cord injuries, accounting for almost half of the new spinal cord injuries each year.
- Falls. A spinal cord injury after age 65 is most frequently caused by a fall.
- Acts of violence. About 12% of spinal cord injuries result from violent encounters, usually from gunshot wounds. Knife wounds also are common.
- Sports & recreation injuries. Athletic activities, such as impact sports & diving in shallow water, cause about 10% of spinal cord injuries.
- Diseases. Cancer, arthritis, osteoporosis & inflammation of the spinal cord also can cause spinal cord injuries.
What are the risk factors for spinal cord injury?
Although a spinal cord injury is usually the result of an accident & can happen to anyone, certain factors can predispose you to be at higher risk of having a spinal cord injury, including:
- Being male. Spinal cord injuries affect an excessive number of men. In fact, females account for only about 20% of traumatic spinal cord injuries in the United States.
- Being between the ages of 16 and 30. More than half of spinal cord injuries take place in people in this age range.
- Being 65 & older. Another projection in spinal cord injuries occurs at age 65. Falls cause the most harm in older adults.
- Alcohol use. Alcohol use is involved in about 25 % of traumatic spinal cord injuries.
- Engaging in risky behavior. Diving into too shallow water & playing sports without wearing the proper safety gear & taking proper precautions can lead to spinal cord injuries. Motor vehicle accidents are the leading cause of spinal cord injuries for people under 65.
- Having certain diseases. A relatively minor injury can cause a spinal cord injury if you have another disorder that affects the joints or bones, like osteoporosis.
What are the Complications of spinal cord injury?
At first, changes in the way the body functions can be overwhelming. However, the rehabilitation team will help you develop tools to address the changes caused by the spinal cord injury, in addition to recommending equipment & resources to promote quality of life & independence. Areas often affected include:
- Bladder control. the bladder will carry on with storing urine from the kidneys. However, the brain might not control the bladder as well because the message carrier (the spinal cord) has been injured.
- The substitute in bladder control increases the risk of urinary tract infections. The changes might also cause kidney infections & kidney or bladder stones. During rehabilitation, you’ll learn ways to help empty the bladder.
- Bowel control. Although the stomach & intestines work much as they did before the injury, control of the bowel movements is often altered. A high-fiber diet might help regulate the bowels, & you’ll learn ways to help control the bowel during rehabilitation.
Pressure injuries. Below the neurological level of the injury, you might have lost some or all skin sensations. Therefore, the skin can’t send a message to the brain when it’s injured by certain things such as prolonged pressure. - This can make you more prone to pressure sores, but changing positions frequently with help, if needed can help prevent these sores. You’ll learn proper skin care during rehabilitation, which can help the patient to avoid these problems.
- Circulatory control. A spinal cord injury can cause circulatory problems ranging from low blood pressure when you rise (orthostatic hypotension) to swelling of the extremities. These circulation changes can also increase the risk of developing blood clots, such as deep vein thrombosis or a pulmonary embolus.
- Another problem with the circulatory system or circulatory control is a potentially life-threatening rise in blood pressure (autonomic dysreflexia). the rehabilitation team will teach the patient how to address these problems if they affect you.
- Respiratory system. the injury might make it more difficult to breathe & cough if the abdominal & chest muscles are affected.
- the neurological level of injury will determine what kind of breathing problems you have. If a patient has a cervical & thoracic spinal cord injury, they might have an increased risk of pneumonia
& other lung problems. Medications & therapy can help prevent & treat these problems.
- Bone density. After spinal cord injury, there’s an increase in the risk of osteoporosis & fractures below the level of injury.
Muscle tone. Some people with spinal cord injuries have one of two types of muscle tone problems: uncontrolled tightening & motion in the muscles (spasticity) or soft & limp muscles lacking muscle tone (flaccidity).
Fitness and wellness. Weight loss & muscle atrophy are common soon after a spinal cord injury. Limited mobility can lead to a more sedentary lifestyle, placing you at risk of obesity, cardiovascular disease & diabetes. - A dietitian can help the patient to eat a nutritious diet to sustain an adequate weight. Physical & occupational therapists can help you develop a fitness & exercise program.
- Sexual health. Men might observe changes in erection & ejaculation; women might notice changes in lubrication after a spinal cord injury. Physicians specializing in urology & fertility can offer options, especially for sexual functioning & fertility.
Pain. Some people have pain, like muscle & joint pain, from overuse of particular muscle groups. Nerve pain can occur after a spinal cord injury, especially in someone who is with an incomplete injury.
Depression. get through the changes a spinal cord injury brings & living with pain causes depression in some people.
How is a spinal cord injury diagnosed?
In an emergency, a healthcare provider makes sure a spinal cord injury is not affecting the breathing or heart rate. Next, they will assess how well the nerves are working. The provider checks:
- Motor function, or the ability to move parts of the body.
- Sensory function, or the ability to feel touch.
- Some imaging tests can help diagnose a spinal cord injury:
- CT scan, to see the broken bones, blood clots & blood vessel damage.
- MRI, to see the spinal cord & soft tissues.
- X-ray, to show broken bones & dislocations (bones knocked out of place).
- A healthcare provider may also use an electromyogram to check the electrical activity in muscles and nerve cells if there are co-existing peripheral nerve injuries. An electromyogram is usually not necessary in a spinal cord injury.
What is the treatment for a spinal cord injury?
Instant treatment:
- You may need emergency surgery for a spinal cord injury if there’s trauma to another part of the body surface. Surgery can also address spinal cord damage from broken bones, blood clots & damaged tissue.
- Some exploration suggests that a corticosteroid injection may help spinal cord injuries. The medication should be given within eight hours after the injury takes place. This treatment may:
- Improve blood flow.
- Preserve nerve function.
- Reduce inflammation.
long-term treatment
The long-term goals of spinal cord injury treatment are :
- Enhancing independence & quality of life.
- decreasing the risk of chronic (ongoing) health conditions.
- Restoring some nerve function in partial injuries.
Long-term complications of a spinal cord injury might include:
- Inability to regulate blood pressure & body temperature.
- Increased risk of heart or lung problems.
- Loss of bladder or bowel control.
- Paralysis in the arms or legs.
- Persistent pain.
- Spasticity, joint contracture.
- Sexual dysfunction.
Will I require rehabilitation after a spinal cord injury?
Most people with a spinal cord injury will require some form of physical rehabilitation or therapy. the person may need inpatient (during a hospital stay) or outpatient (after a hospital stay) rehabilitation. A rehabilitation team can help you:
- Learn to use assistive devices like walkers or wheelchairs.
- Regain strength & mobility in areas or parts of the body with nerve function.
- Recover the skills needed for activities of daily living (ADL), including dressing & using the toilet.
What are neural prostheses & how can they help a spinal cord injury?
- Neural prostheses (artificial body parts) are a prospective new treatment for spinal cord injuries. A neural prosthesis restore lost nerve function like how an arm or leg prosthesis replaces a lost limb. An electrical instrument connects to nerves that are still functioning. You use those nerves to control the prosthesis, which helps you move immobile parts of the body.
What is the physiotherapy treatment for spinal cord injury?
Important Concepts for Physiotherapy
It’s important that Physiotherapists understand the following concepts & their concepts to the management process.
- Vertebral column Injuries (acute phase affects the intensity of therapy)
- Spinal Shock (reflexes are briefly absent for 3 days to 3 months)
- Autonomic Dysreflexia (Spinal cord injury above T6 leads to increased sympathetic activity
- Orthostatic Hypotension (blood pressure-associated dizziness due to postural changes mobilizing from supine to sitting)
- Deep Venous Thrombosis (DVTs) & Pulmonary embolus (PE) (know the signs & symptoms of these conditions to ensure safe therapy)
- Bladder- & Bowel Dysfunction
- Pressure sores (prevention forms part of therapy sessions)
- consume Ossification (calcification of soft tissue that can lead to contractures)
- Psychological & Emotional Distress (notice signs & symptoms & refer to appropriate team members
The acute management & rehabilitation of Spinal cord injury depend on the level & type of injury to the spinal cord. Individuals with a Spinal cord injury often require initial treatment in an intensive care unit with the rehabilitation process typically starting in the acute care setting, followed by extended treatment in a specialized Spinal Injury Unit. Inpatient treatment can last from 8 – 24 weeks, with follow-up outpatient rehabilitation from 3 – 12 months, generally followed by yearly medical & functional reviews.
The management of an individual with Spinal cord injury is complex & lifelong requiring a multidisciplinary approach. A functional, goal-aligned, interdisciplinary, rehabilitation program should enable the individual with a spinal cord injury to live as full and independent a life as possible. Physiotherapy, occupational therapy, speech & language therapy, rehabilitation nurses, social workers, psychologists & other health & social care professionals work as a team work under the coordination of a Physiatrist or Rehabilitation Physician to decide on goals with the individual & develop a plan of discharge that is appropriate for the individuals level of injury and circumstances
Five key steps in the treatment of individuals with Spinal cord injury are;
Assessing impairments, activity limitations & participation restrictions
Setting goals relevant to activity limitations & participation restrictions
Identifying key impairments that are limiting the achievement of goals
Identifying & administering physiotherapy treatments (strengthening, joint mobility, motor skill development, cardiovascular fitness, respiratory functioning, pain management)
Measuring the outcome of treatments.
The treatment of individuals with a Spinal Cord Injury can be divided into 3 Phases;
Physiotherapy’s role in preventing respiratory complications:
Respiratory Function.
Common secondary complications include hypoventilation, atelectasis, secretion retention & pneumonia.
The respiratory function is affected due to disruption in the spinal cord relevant to the neurological level of the Spinal cord injury.
Levels of innervations are; C3-5 Diaphragm, C3-8 Scalenes, C5-T1 Pectoralis, T1-11 Intercostalis & T6-12 Abdominals.
Individuals with C1-3 tetraplegia require mechanical ventilation & most individuals with C4 tetraplegia will be able to breathe independently. Although individuals with spinal cord injury C4 to T12 can breathe independently, they might still have decreased vital capacity & difficulty in raising intra-abdominal pressure for an effective cough or other forced-expiratory techniques (FETs).
Physiotherapy interventions should always include secretion clearance & increased ventilatory techniques. Secretion clearance techniques include percussions, vibrations & shaking, as well as postural drainage & suctioning. Treatment to improve ventilation includes abdominal binders, positioning, deep breathing exercises, incentive spirometry & inspiratory muscle training. Other medical apparatus often used to improve ventilation are continuous positive airway pressure (CPAP) & bi-level positive airway pressure (BiPAP).
- Initiating respiratory muscle training
- Instruction on assisted coughing & nose blowing
- Providing active chest physiotherapy
- Diaphragm pacing is a new method to help patients with spinal cord injuries reduce their dependence on a mechanical ventilator. Other benefits include promoting neuromuscular plasticity, improvements in spontaneous diaphragm activation & respiratory function, & improvement in breathing, speech & quality of life for people with spinal cord injuries.
Physiotherapy’s role in preventing cardiovascular complications:
- Deep vein thrombosis (DVT) prophylaxis: early limb mobilization, intermittent compression
- Management of postural hypotension, bradycardia & autonomic dysreflexia
Physiotherapy’s role in preventing musculoskeletal complications:
- To prevent lower and upper extremities contracture consider ankle, knee, hip, :& shoulder joints to allow for: wheelchair positioning (ankles, knees), bed mobility, transfers, and dressing (shoulders, hips)
- Facilitate elbow extension in patients with a C5/6 Spinal cord injury & wrist extension in patients with a C6 Spinal cord injury.
- Educate on positions in bed & wheelchair that can decrease the spasticity
- Reinforce good posture using only one or no pillow under the neck in the supine position, early assessment for wheelchair seating & positioning
- Position for functional shortening of the long finger flexors to facilitate tenodesis grip (patients to be in pronation with finger flexion & wrist extension)
physiotherapy’s role in the Range of movement (FROM) of all joints
- Reduced ROM may lead to contractures due to immobility & poor positioning, as well as increased tone & spasticity.
- Treatment techniques should include passive stretches, positioning in the lengthened position & other common hypertonic treatment techniques such as compression, heat & sustained deep pressure.
Maintaining & strengthening innervated muscles
Progressive resistance training & functional strength training is clinically identified to achieve favorable results in maintaining & strengthening innervated muscle groups.
Prevention of Pressure Ulcers
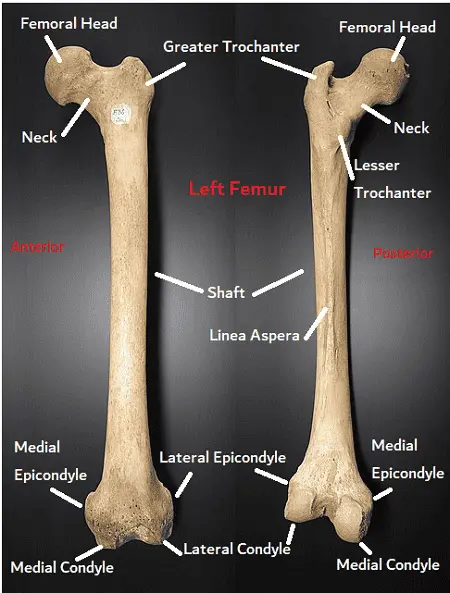
Areas prone to pressure ulcers include; the occiput, scapulas, sacrum & heels when lying supine. While the greater trochanter & malleoli are more prone to side lying.
In the acute phase, interventions include passive pressure care, such as frequent rolling regimes & mobilizing, as well as adequate skin moisturizing, nutrition & monitoring.
Later, in the sub-acute & long-term phases, individuals will be taught how to perform frequent self-lift techniques in order to relieve pressure.
physiotherapy role inBed mobility & transfers
C6 & lower level Spinal cord injury has the ability to attain 5 motor skills;
- rolling (using momentum)
- mobilizing from supine to long-sitting
- unsupported sitting (short- & long sitting)
- lifting vertically
- transfers
- C6 tetraplegia might have some challenges, but these 5 motor skills are still workable with some modifications. With rolling, C6 tetraplegia should externally rotate shoulders & swing arms beyond their body instead of over-head. During an unsupported sitting, C6 tetraplegia should externally rotate shoulders & lock elbows in extension to maintain balance. Vertical lifting for individuals with C6 tetraplegia can be possible by passively extending elbows, externally rotating shoulders & depressing shoulders to weight bear with hands placed anteriorly to the pelvis.
Physiotherapists can help prevent UTIs & bladder overfilling in patients with a spinal cord injury by
- Encouraging the patient to drink enough water
- functioning with an occupational therapist on the proper equipment to facilitate independent hydration (wheelchair cup holder with a cup & a long drinking straw)
- Following aseptic procedures with catheter care, keeping the catheter off the floor during a therapy
- Maintaining the schedule for timely catheterization
Wheelchair mobility
- Individuals with C1-4 tetraplegia require powered-WCs. These Wheelchairs may be controlled by chin movements, sip & puff & head array.
- particular with C5 tetraplegia most commonly use powered-WCs controlled by hand movement.
- Most individuals with C6-8 tetraplegia are able to independently mobilise with a manual WC, however, might use a hand-controlled WC as an alternative.
- particular with Spinal cord injury lower than C8 will be able to independently mobilize with a manual WC.
- Individuals with SCI should be orientated to their new way of mobilization. Turning, opening & closing doors, going up & down inclines, going around & over obstacles, as well as mobilizing indoors & outdoors are important activities to practice in order to ensure safe & independent mobility.
- The recent study concludes that participants with SCI predict the importance of fall prevention initiatives that extend beyond the offered strategies, suggesting a need for the structure & content of future fall prevention strategies for wheelchair users. Further research is required to examine the efficacy of specific fall prevention initiatives by collecting feedback from community-dwelling wheelchair users with Spinal cord injury
Gait & standing
- Gait training, strengthening, & balance exercises were the most prevalent physiotherapy activities in individuals with an AIS D spinal cord injury. Overall strengthening was the most common group therapy activity beyond all levels & types of spinal cord injury.
- The capability to stand & walk is dependent on various factors however, standing has many benefits even if independent standing might never be a possibility. Benefits include emotional well-being, orthostatic hypotension, bone mineral density, spasticity,& bladder & bowel function. Standing can be attained by using assistive devices such as; tilt tables, standing WCs &/ or standing frames. Individuals with paraplegia might be strong enough to stand in parallel bars using knee extension splints or orthoses.
- Gait training is possible among individuals with complete paraplegia to partially paralyzed lower extremities by using orthoses & walking aids such as; knee-ankle-foot & hip-knee-ankle-foot orthoses.
- Other important aspects of rehabilitation are;
- Cardiovascular fitness & pain management.
Sub-acute (Rehabilitation) Phase
- The rehabilitation needs of individuals with a Spinal cord injury are best at a specialized Spinal Cord Injury Unit, but often rehabilitation begins in the Acute & Trauma Hospital while the individual is expecting transfer to a Spinal Injuries Unit. Rehabilitation requires consideration of the whole person; their physical, psychological, vocational & social background. The rehabilitation process is a goal-directed, & time-limited process aimed at facilitating maximal independence & optimal reintegration back into the individual’s chosen community role & lifestyle.
- Physiotherapy is a key section during the rehabilitation process following spinal cord injury & includes a variety of interventions that address multiple domains in the International Classification of Functioning, Disability & Health (ICF) including body function & structure, activity limitation, & participation, with many interventions directed at preventing, rather than treating, impairments, activity limitation & participation restrictions. Quality of Life including community participation, gainful employment, interpersonal relationships, & leisure activities has become the overriding focus of management.
Long Term Phase
- Individuals with a spinal cord injury, depending on the level and type of lesion, may have many complex needs & face wide-ranging, long-term restrictions in their ability to live independently, drive or use public transport, return to work or education, & participate in leisure and social activities. To ensure successful long-term management coordinated community rehabilitation services and long-term support are required to meet the long-term & ongoing needs of individuals with a spinal cord injury. Best practice in long-term management includes active case management with case managers with the appropriate training, clinical expertise & knowledge of services to coordinate care post-initial rehabilitation & ensure ongoing personalized case management for patients with complex or ongoing needs. A prospective longitudinal study suggests the need for screening of the efficacy of patients and their family members to help prevent personal and family adjustment problems as low self-efficacy of the patients/family members appears to be a risk factor for accommodation problems in individuals with spinal cord injuries.
Treatment of the rehabilitation phase includes:
- to establish an interdisciplinary process that is patient-focused, comprehensive & co-ordinated
to address physical motor functional activities with early intervention & management to prevent further complications
to improve an individual’s independence in activities of daily living, such as bathing, eating, dressing, grooming, & Mobility
to reach functional independence, whether physical- or verbal equipment in order to facilitate this independence
to reach & maintain successful reintegration into the community.
The range of therapy activities used by physiotherapists during rehabilitation varies depending on the level & type of injury. The three most common various therapy activities for individuals with high-level tetraplegia were – range of motion/stretching, strengthening, & transfers; while for those with low tetraplegia, more time was spent on transfers than strengthening. Similarly, in individuals with paraplegia, the most common individual physiotherapy activities were transfers, followed by a range of movement/stretching, & strengthening. - Individuals with different levels of SCI perform different motor tasks differently & it’s important for physiotherapists to understand which functions are obtainable & relevant to the Spinal cord injury level. All motor tasks should be split into sub-tasks in order to perform activities perfectly. In order to perform motor tasks successfully individuals should have sufficient strength, balance, ROM & knowledge, or skill regarding the specific motor task. All these aspects can be reached through frequent progressive training.
The following are supplementary activities to help prevent gastrointestinal coexisting that the physiotherapist can be a part of:
- Assist with bowel regime to stave off constipation & prevent distension of the abdomen
- Educate on balancing activity level & Intake
- Educate patients on obesity prevention
- Follow up on calorie counts
Preparing for Function
Early introduction of physiotherapy interventions during the acute phase of rehabilitation after a spinal cord injury should focus on the functions:
- Teaching trick movements for individuals with a C5/6/7 spinal cord injury, including elbow extension without triceps, & tenodesis grip
- Strengthening innervated & partially innervated muscles for function
- Facilitation of weak & paralyzed muscles
- Maintaining full joint range of motion
- Educate patients on how to perform functional activities & why stretches, muscle strengthening, positioning & skills training are important to give them vision.
- Educate patients about their condition, complications, possible outcomes & length of stay & goals. This required constant repeating, as patients are not always ready to hear the information given.
- Make sure the patient has the cognitive capability for the level or task of education being given. Pictures should be provided for those who cannot read, consider language (mother tongue or competent translator) & education should match a patient’s educational level.
- Assisting with spasticity management
Functional Approach
When directing a patient’s functional ability, the clinician should consider the following principles:
- Treat the impairments
Don’t stick to normal functional levels (i.e. rolling before sitting up), but focus on the patient’s present abilities
Use activities as an exercise
Understand all the components of an activity a patient need for a specific function
Break activities into smaller components & work on them
Stretching, strengthening & maintaining range of motion is crucial for good function
Use peer supporters to inspire the patient
Make patients feel they have achieved something in a session, end with something they do well or enjoy - The following tools can be used to smoothen or increase the function:
- Tilt table, standing frame, parallel bars standing with long leg orthoses, treadmill, Lokomat to facilitate ambulation
Functional Electrical Stimulation (FES) to facilitate the restoration of muscle function
- Tilt table, standing frame, parallel bars standing with long leg orthoses, treadmill, Lokomat to facilitate ambulation
What is the Prevention of spinal cord injury?
Following this advice might reduce the risk of a spinal cord injury:
- Drive safely. Car crashes are one of the most common causes which can lead to spinal cord injuries. Wear a seat belt every time when you are in a moving vehicle.
- Make sure that your children wear a seat belt or use an age & weight-appropriate child safety seat. To guard them against airbag injuries, children under age 12 should always ride in the back seat.
- Check water depth before diving. Don’t dive into a pool unless it’s 12 feet (about 3.7 meters) or deeper, don’t dive into an aboveground pool & don’t dive into water if you don’t know how deep it is.
Prevent falls. Use a step stool with a grab bar to reach heightened objects. Add handrails along stairways. Put nonslip mats on tile floors & in the tub or shower. For young children, use safety gates to block stairs & consider installing window guards.
Take precautions when playing sports. Always wear recommended safety gear. Avoid leading with the head in sports. For example, don’t slide headfirst in baseball, & don’t tackle using the top of the helmet in football. Use a surveilling for new moves in gymnastics.
Don’t drink & drive. Don’t drive while intoxicated & under the influence of drugs. Don’t travel with a driver who has been drinking & driving.
FAQ
What is the most common spinal cord injury?
According to the National Spinal Cord Injury Statistical Center (NSCISC), the two most common types of spinal cord injuries are incomplete tetraplegia & paraplegia, with incomplete spinal cord injuries accounting for more than 65% of all SCIs.
What should you not do with a spinal injury?
Avoid moving the head & neck.
Provide as much first aid as possible without moving the person’s head & neck. If the person shows no signs of circulation such as(breathing, coughing & movement), begin CPR, but do not tilt the head back to open the airway.
What are the 5 signs of a spinal cord injury?
Emergency signs & symptoms
Extreme back pain or pressure in the neck, head & back.
Weakness, incoordination & paralysis in any part or any area of the body.
Numbness, tingling, & loss of sensation in the hands, fingers, feet, & toes.
Loss of bladder or bowel control.
Difficulty with balance & walking.
What are the top 3 causes of spinal cord injuries?
Some of the most common causes of spinal cord injury caused by motor vehicle accidents are falls, gunshot wounds, sports injuries & surgical complications.
What is the weakest part of the spine?
Biomechanical studies have shown the endplate to be the weakest component of the vertebral body under repetitive loading conditions.
How long does it take for maximum recovery for most spinal cord injuries?
Although most recovery occurs within the first 3-6 months following a spinal cord injury, recovery can continue well past that period. Consistently practicing affected movements & activities will help promote or enhance neuroplasticity
Why spinal cord injuries are permanent?
Spinal cord injuries are permanent because it’s direct damage or effect on the nerves that send signals to the brain that controls many of our functions. While modern medicine can help partially heal some of those wounds & allow some with spinal injuries to lead independent lives, there are some injuries that are permanent.
Can spinal cord injury be seen or diagnosed on MRI?
MRI is useful for the initial diagnosis of acute spinal cord injury & its prognostication for predicting neurological recovery.


22 Comments