Elbow Pain: Physiotherapy Management
What is an Elbow Pain?
Elbow pain mostly occurs due to overuse of your muscles around the elbow joints such as Many sports, hobbies and jobs require repetitive hand, wrist or arm movements.
- Elbow pain usually isn’t serious, because you use your elbow in so many ways, elbow pain can be very frustrating but recover within few days with the help of Physiotherapy treatment and exercise..
- Your elbow joint is a complex joint; it allows you to both extend and flex, as well as rotate your hand and forearm. Since most movements are a combination of these actions, you may sometimes find it difficult to describe exactly which movement
- Brings on the pain.
Elbow disorders may involve any of the following:–
1.arm muscles
2.elbow ligaments
3.tendons
4.bones in the arm
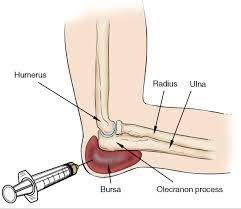
5.bursae
Anatomy of Elbow Joint:
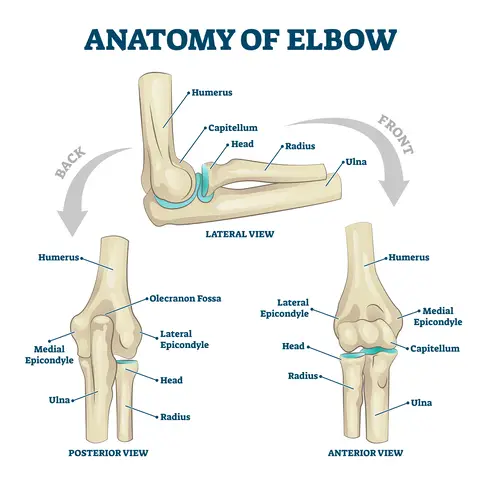
- The elbow joint is where the long bone at the top of your arm, known as the humerus, meets the two bones in your
- Forearm – called the radius and the ulna. It’s a hinge joint, and it allows you to bend your arm. The upper part of the radius can rotate so you can twist your forearm.
- The end of the humerus has two bony parts that you can feel at either side of your elbow. These are:
- The lateral epicondyle on the outside of your arm
- The medial epicondyle on the inside of your arm.
- Muscles attached to the outside of the humerus help you straighten your wrist and fingers. These are connected to the brain and nervous system through the radial nerve, which travels on the outside of the elbow.
- Muscles attached to the inside of the humerus help you bend your wrist and fingers, and let you grasp objects. These-muscles are connected to the brain and nervous system through the median nerve, which runs in front of the elbow.
- The ulnar nerve, which is on the inside of the elbow is mainly responsible for the movements of the small muscles of the hand. These are useful for precise and delicate hand movements. The feeling of hitting your funny bone is caused by the ulnar nerve being pinched.
- There are also strong cords in the elbow that help to hold the joint in place. Tendons attach muscles to bones and ligaments link bones together.
Causes and Symptoms of Elbow Pain :
Elbow pain is often caused by overuse. Many sports, hobbies and jobs require repetitive hand, wrist or arm movements.
Elbow pain may occasionally be due to arthritis, but in general, your elbow joint is much less prone to wear-and-tear damage than are many other joints.
Common causes of elbow pain include:-
- Broken arm
- Bursitis (joint inflammation)
- Dislocated elbow
- Golfer’s elbow
- Osteoarthritis (disease causing the breakdown of joints)
- Osteochondritis dissecans
- Rheumatoid arthritis (inflammatory joint disease)
- Sprains
- Stress fractures
- Tendinitis
- Tennis elbow
- Throwing injuries
- Trapped nerves
There are at least ten different types of elbow disorders. Read on to learn about their symptoms and causes
Medial Epicondylitis:
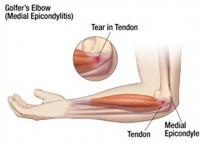
- It is commonly called golfer’s elbow and little leaguer’s elbow.
- Medial epicondylitis is inflammation at the point where the tendons of the forearm attach to the bony prominence of the inner elbow. As an example, this tendon can become strained in a golf swing, but many other repetitive motions can injure the tendon.
Symptoms
- The patient usually complains about pain of the elbow distal to the medial epicondyle of the humerus with radiation up and down the arm, most common on the ulnar side of the forearm, the wrist and occasionally in the fingers.
- Local tenderness over the medial epicondyle and the conjoined tendon of the flexor group, without evidence of swelling or erythema, are also characteristics that can occur. Other symptoms are stiffness of the elbow, weakness in the hand and the wrist and a numb or tingling feeling in the fingers (mostly ring and little finger).
- The pain is evoked by resisted flexion of the wrist and by pronation. The pain is usually accompanied by a weakness of hand grip. Pain can begin suddenly or can develop gradually over time.
Lateral Epicondylitis:
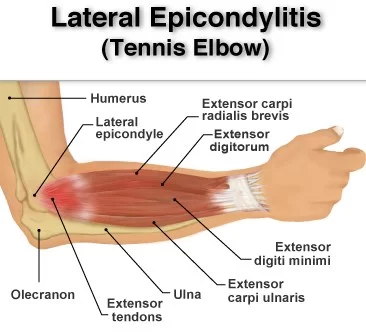
- Another name for lateral elbow tendinopathy is tennis elbow.
- The lateral epicondyle is the outside bony portion of the elbow where large tendons attach to the elbow from the muscles of the forearm. These tendons can be injured, especially with repetitive motions of the forearm, such as using a manual screwdriver, washing windows, or hitting a backhand in tennis play.
- Professionals who commonly experience lateral epicondylitis include:-
Cook, Painters
Carpenters
Autoworkers
Plumber
Symptoms
- Symptoms such as pain or burning occur along the outside of the elbow. You also may experience problems with gripping.
- Tennis elbow then leads to inflammation of the tendons, causing pain over the outside of the elbow, occasionally with warmth and swelling but always with local tenderness. The elbow maintains its full range of motion, as the inner joint is not affected, and the pain can be particularly noticed toward the end of the day.
- Repeated twisting motions or activities that strain the tendon typically elicit increased pain. These include lifting and throwing.
These symptoms usually improve with:
- The most prominent symptom of epicondylitis lateralis is pain, this pain can be produced by palpation on the extensor muscles origin on the lateral epicondyle. The pain can radiate upwards along the upper arm and downwards along the outside of the forearm and in rare cases even to the third and fourth fingers. Furthermore it is also often seen that the flexibility and strength in the wrist extensor and posterior shoulder muscles are deficient.
According to Warren, there are four stages on the development of this injury with regard to the intensity of the symptoms.
- Faint pain a couple of hours after the provoking activity.
- Pain at the end of or immediately after the provoking activity.
- Pain during the provoking activity, which intensifies after ceasing that activity.
- Constant pain, which prohibits any activity.
- Furthermore it is also often seen that the flexibility and strength in the wrist extensor and posterior shoulder muscles are deficient. At least patients report weakness in their grip strength or difficulty carrying objects in their hand, especially with the elbow extended. This weakness is due to finger extensor and supinator weakness. Some people have a sense of paralysis but this is rare.
- Symptoms last, on average, from 2 weeks to 2 years. 89% of the patients recover within 1 year without any treatment except perhaps avoidance of the painful movements.
Elbow Bursitis:
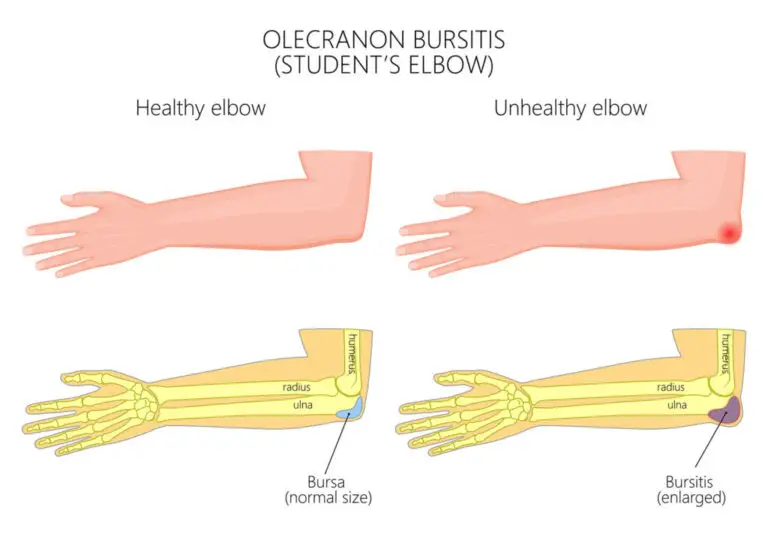
- Student’s elbow, miner’s elbow, draftsman’s elbow
- Bursitis affects bursae, small sacs of fluid that help protect the joints. Olecranon bursitis affects the bursae protecting the pointy bone of the elbow.
It may be caused by:
1.a blow to the elbow
2.leaning on the elbow for a prolonged period of time
3.infection
4.medical conditions such as arthritis
Symptoms include:
- Patients usually remark a focal swelling at the posterior elbow, the swelling is sometimes painless.
- Pressure, like leaning on the elbow or rubbing against a table while writing with the ipsilateral hand, are factors that can often exacerbate the pain.
- Chronic recurrent swelling is usually not tender.
- A typical symptom of olecranon bursitis is the frequent bumping of the swollen elbow because it protrudes further than it usually would.
- It is possible that the patient reports a history of isolated trauma or repetitive microtrauma. The start may be sudden when it is secondary to infection or acute trauma. When olecranon bursitis is secondary to chronic irritation, the onset will be more gradual.
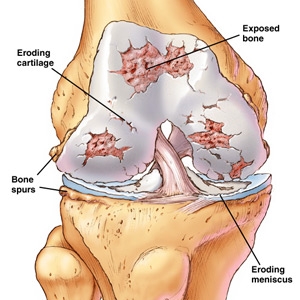
Osteoarthritis of Elbow:

- Osteoarthritis (OA) is a condition that affects the cartilage, a type of connective tissue found in the joints. OA causes this tissue to wear down and become damaged. Elbow OA may be caused by an elbow injury, or wear and tear on the joints.
- Inflammation of the elbow joint (arthritis) can occur as a result of many systemic forms of arthritis, including rheumatoid arthritis, osteoarthritis, gouty arthritis, psoriatic arthritis, ankylosing spondylitis, and reactive arthritis (formerly called Reiter’s disease).
Symptoms:
- Pain
- Heat
- Tenderness
- Warmth
- Difficulty bending the elbow
- A locking sensation in the elbow
- A grating sound during movement
- Swelling
- Decreased range of motion.
Dislocation or Fracture of the Elbow:
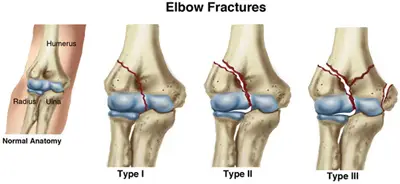
- An injury to the elbow, such as a fall on an outstretched arm or elbow, can cause dislocation or a fracture. Dislocation occurs when a bone moves from its usual position. A fracture occurs when a bone cracks or breaks.
Symptoms include:
- Instability
- Popping sensation on immediate injury
- Pain
- -Weakness
- Reduced AROM
- Swelling – the olecranon may be prominent creating a divot over distal triceps
- Joint line tenderness on palpation
- Recurrent dislocations can occur if a ligament injury is also sustained.
Ligament Sprain and Strain:

- Ligament problems can occur in any of the ligaments located in the elbow joint. Ligament sprains may be the result of trauma or repeated stress.
- A sprain is a stretch or tear injury to a ligament. One or more ligaments can be injured during a sprain. This might occur when the elbow is hyper extended or simply jammed, such as in a “stiff arm” collision. The severity of the injury will depend on the extent of injury to a single ligament (whether the tear is partial or complete) and the number of ligaments involved.
The ligament may be:
- Stretched
- Partially torn
- Completely torn
- Sometimes you’ll hear a popping noise upon injury.
Symptoms include:
- Elbow Pain
- Joint instability
- Swelling around Elbow joint
- Problems with range of motion
- Treatment may include:
Osteochondritis Dissecans:
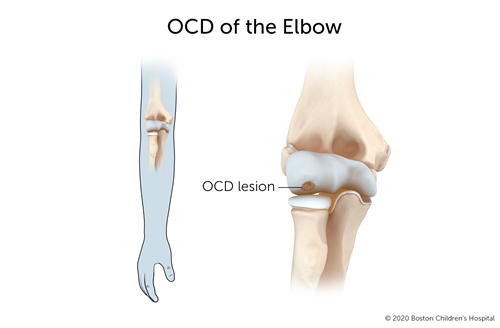
- Osteochondritis dissecans, also called Panner’s disease, occurs when small pieces of cartilage and bone become dislodged in the elbow joint. It’s often the result of a sports injury to the elbow and is most often seen in young men.
symptoms :
- Lateral Pain over the joint
- Stiffness
- Feeling of instability
- Stiffness after resting
- Locking
- Giving way
- Popping/clicking
- Tenderness on the outside of the elbow .
- Trouble extending the arm .
Cellulitis:

- Inflammation of the skin related to infection (cellulitis) commonly occurs as a result of abrasions of the skin. When abrasions or puncture wounds occur, bacteria on the surface of the skin can invade the deeper layers of the skin.
- The most common bacteria that cause cellulitis include Staphylococcus and Streptococcus. Patients can have an associated low-grade fever
- Cellulitis can lead to infection of the olecranon bursa, causing olecranon bursitis
Symptoms :
- Typical symptoms include acute poorly demarcated and spreading erythema along with pain, swelling, and warmth of The lower extremity but can occur on any area of skin or underlying subcutaneous tissue.
- Symptoms may include fever, nausea, vomiting, and rigors.
- Other features include proximal dilated and edematous skin lymphatics and bulla formation.
- Cellulitis predominantly has a unilateral presentation.
Septic Arthritis:
Infection of the elbow joint with bacteria (septic arthritis) is uncommon. It is most often seen in patients with suppressed immune systems or diabetes, those taking cortisone medications, or intravenous drug abusers. The most common bacteria that cause infection of the elbow joint are Staphylococcus and Streptococcus.
Symptoms :
- Heat
- Swelling
- Redness
- Pain
- Limited range of motion of the elbow joint
- Septic arthritis is often associated with fever, sweats, and chills .
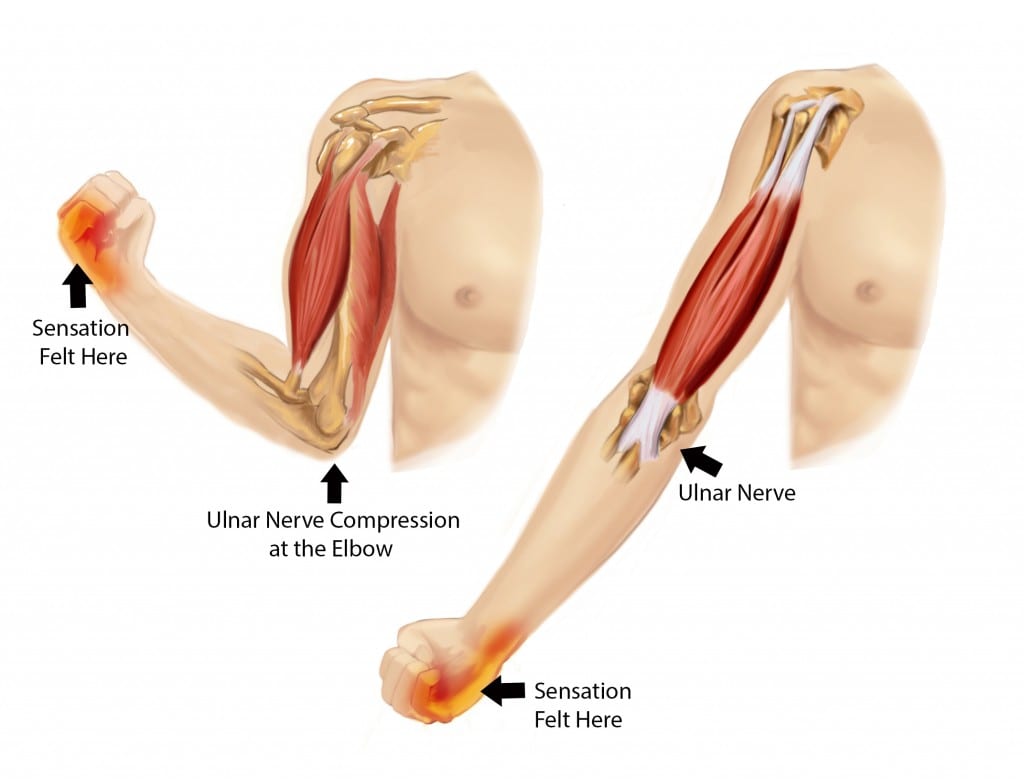
Ulnar nerve Entrapment:
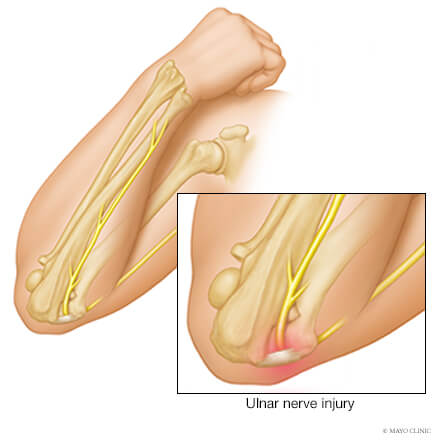
- The ulnar nerve is the “funny bone” nerve which travels between the tip of the elbow and the inner elbow bone. At this site it can be “pinched” by normal structures or swollen structures after injury. This pinching is referred to as entrapment.
- In rare cases, it can be due to arthritis. Other causes can include a fracture around the nerve which has healed into a different position or new bone growing when the fracture heals.
Symptoms :
- Symptoms of ulnar nerve entrapment include tingling in fingers 4 and 5, weak grip strength, pain and sensitivity on the
- ulnar side of the forearm, wrist and hand, muscle atrophy, clawing of digits 4 and 5 (sign of benediction).
Cubital Tunnel Syndrome can present in different grades of severity:
Grade I: Mild symptoms including:
- Intermittent paresthesia
- Minor hypoesthesia of the dorsal and palmar surfaces of the fifth and medial aspect of fourth digits
- No motor changes
Grade II: Moderate and persistent symptoms including:
- Paresthesia
- Hypoesthesia of the dorsal and palmar surfaces of the fifth and medial aspect of fourth digits
- Mild weakness of ulnar innervated muscles
- Early signs of muscular atrophy
Grade III: Severe symptoms including:
- Paresthesia
- Obvious loss of sensation of the dorsal and palmar surfaces of the fifth and medial aspect of fourth digits.
- Significant functional and motor impairment
- Muscle atrophy of the hand intrinsics
- Possible digital clawing of fourth and fifth digits (Sign of Benediction)
Guyon’s Canal Syndrome symptoms include:

- Muscular atrophy – Primarily the hypothenar muscles and interossei with muscle-sparing of the thenar group:
- 1.weakened finger abduction and adduction (interossei)
- 2.weakened thumb adductor (adductor pollicis)
- Sensory loss and pain which may involve the palmar surface of the fifth digit and medial aspect of the fourth digit & the
- dorsum of medial aspect of the fourth finger and the dorsum of the fifth finger don’t have sensory loss.
- Ulnar Claw may present (sign of Benediction)
How Diagnosis are done in Elbow Pain?
Your doctor can diagnose elbow disorders through X-ray, Sonography
MEDIAL EPICONDYLITIS:
X-rays
- for epicondylitis are usually normal but can indicate calcification of the tendons if the tendinitis has persisted for extended periods of time.
Ultrasound:-
- May be identified as outward bowing, heterogeneous echogenicity, or thickening of the common tendon, with subspace .
- fluid collection and intratendinous calcification. Discrete tears appear as hypo echoic regions with adjacent tendon discontinuity. Color Doppler may show tendon hyperemia. Dynamic assessment can also be performed to delineate Instability.
MRI :
- Described features on MRI include:-
- Thickening and increased signal intensity on both T1 and T2 weighted sequences of the common flexor tendon
- Soft tissue edema around the common flexor tendon – peritendonitis
- Marrow edema in the medial epicondyle
- Muscle atrophy may occur in longstanding cases
LATERAL EPICONDYLITIS:-
Investigations are usually not performed in the straightforward case of lateral elbow pain.
Ultrasound examination :
- May prove to be a useful diagnostic tool in the investigation of patients with lateral elbow pain.
- Ultrasound may demonstrate the degree of tendon damage as well as the presence of a bursa.
X-rays :
- These may be taken to rule out arthritis of the elbow. 16% calcification along lateral epicondyle.
- However, in longstanding cases, plain X-ray (AP and lateral views) of the elbow may show osteochondritis dissecans,degenerative joint changes or evidence of heterotopic calcification.
Magnetic Resonance Imaging (MRI):
- If the symptoms are related to a neck problem, an MRI scan may be ordered. This will show if there is a possible herniated disk or arthritis in your neck. Both of these conditions often produce arm pain.
- MRI- 100% thickening
Electromyography (EMG) :
- An EMG is used to rule out nerve compression. Many nerves travel around the elbow, and the symptoms of nerve compression are similar to those of tennis elbow.
BURSITIS :

Lateral radiograph of the elbow reveals soft tissue swelling superficial to the olecranon. Traumatic fracture or calcification in gout or CPPD may be evident.
CT:
- Fluid density at the subcutaneous tissue superficial to the elbow.
MRI:-
Bursal fluid collection has the following features:
- T1: hypointense
- T2: mainly hyperintense
- C+ (Gd): enhancement of bursal margins
Laboratory tests :
- Laboratory tests are essential to differentiate septic from non-septic bursitis when doubt remains after clinical examination, so the aspirate should be sent for microscopy and culture.
Blood tests :
- Blood tests are not usually helpful. If there is any doubt about the diagnosis then treatment should be given as for septic case until culture results are available.
OSTEOARTHRITIS :
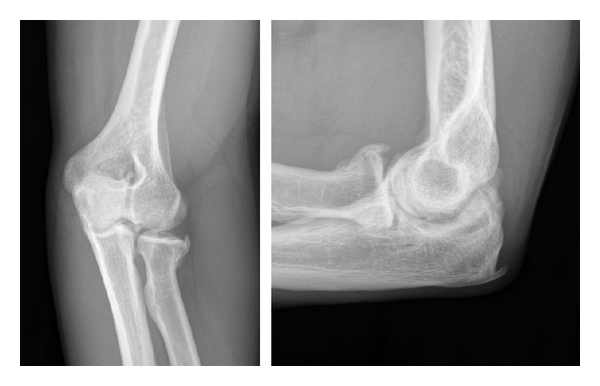
X-ray :
- It is most commonly used when imaging the elbow joint. Expect to see projections for anteroposterior, lateral and oblique directions.
- On viewing an x-ray the central joint space is usually preserved with osteophytes typically located at the anterior and posterior aspects. It is important to review previous images especially when there is a history of trauma. With such a history, clinicians should look out for malalignment, incongurency of the joints, or evidence of heterotopic ossification. Stress radiographs are sometimes used when there is a history of instability.
CT :
- It is useful in complex cases such as heterotopic ossification, intra-articular loose bodies, bony deformity or malunion is suspected in the setting of previous fracture.
MRI :
- It has a limited role in diagnosis and is used only in rare occasions.
DISLOCATION OR FRACTURE :

- If an elbow dislocation is associated with a fracture (fracture-dislocation), it is called “complex.” An isolated dislocation without fracture is “simple.”
- The most common associated fracture in adults is a radial head fracture, although coronoid process fracture is also common. When all of these occur together in a severe posterior dislocation, it is known as the terrible triad of the elbow .
- Other elbow fracture dislocation patterns include the trans-olecranon fracture-dislocation and anteromedial coronoid fractures with associated varus posteromedial instability.
- The most common associated fracture in children is a medial epicondyle fracture .
*CT :
- Computed tomography (CT) is frequently used in the acute setting to evaluate for fractures.
- It is particularly useful demonstrating intraarticular extension of fractures, the distribution of small fracture fragments within and adjacent to the joint space, as well as any associated bony malalignment. For example, CT might best depict a “terrible triad” fracture-dislocation (radial head fracture, coronoid fracture, LUCL injury following dislocation), which might require surgery.
- Similarly, CT can precisely demonstrate the degree of displacement of an articular fracture (> 2 mm step-off or gap), which would indicate the need for internal fixation.
- Although rarely required in practice, a line drawn along the anterior margin of the humerus (anterior humeral line) and one along the long axis of the radius should intersect near the center of the capitellum .
ELBOW SPRAIN AND STRAIN:
X-rays :
- It is use high-energy beams of light to create pictures of the body. Your doctor may recommend an X-ray to examine the bones of the elbow and rule out another cause of the pain, such as a fracture or a dislocation. This test can also determine if an abnormality in the bones or loose pieces of bone are causing your symptoms.
- An X-ray may also reveal an accumulation of fluid around the elbow, which is a sign of a sprain or strain.
Ultrasound :
- In an ultrasound, high-frequency sound waves produce clear images of soft tissue, such as muscles and ligaments.
- Doctors at NYU Langone use ultrasound to check the tendons for swelling, which can be a sign of tendinitis.
- This test can also reveal small tears or stretched ligaments, which helps the doctor determine if an elbow injury is the result of chronic overuse.
- Many specialists at NYU Langone’s Center for Musculoskeletal Care have ultrasound machines in their offices.
- Alternatively, your doctor may refer you to a musculoskeletal radiologist at our imaging services.
MRI :
- In MRI, a powerful magnetic field and radio waves create images of soft tissues inside the body. MRI can detect injuries to deep soft tissue and bones that might not be visible on an ultrasound or X-ray.
CT :
- Intraarticular contrast material can be injected for improved visualization of joint bodies and cartilage.
- Osseous manifestations of secondary degenerative change are also well evaluated with CT.
- Less often, CT arthrography is performed for evaluation of ligamentous integrity in patients with contraindications to MR imaging .
OSTEOCHONDRITIS DISSECANS:

- Non-specific findings,mostly normal,may show irregularities and fragmentation of capitellum.
Magnetic Resonance Imaging :
- (MRI) will show any accumulation of fluid in the area and can detect any loose fragments. MRI should be considered when symptomatic patients have a normal X-Ray.
Computerised Tomography :
- (CT) can detect any bony fragments, pinpoint their location and determine whether they have settled in the joint space.
CELLULITIS :
- Cultures are typically not beneficial in making a cellulitis diagnosis.
- It is most commonly diagnosed by history an physical examination alone.
laboratory tests :
- It can indicate the presence of infection, but are not specific to cellulitis alone.
MRI :
- Studies can identify more severe infections to differentiate from cellulitis, but are not a reliable diagnostic tool for cellulitis itself.
- Identification of the cause of the infection through blood, needle aspiration or punch biopsy are not recommended unless the patient has a complication or abnormal exposure history eg immunosuppressants, a diagnosis of chronic liver disease, aquatic soft tissue injury, animal and human bites, or being in contact with various bacterias.
- If a biopsy and culture are warranted, a histopathologic evaluation will be performed on the sample.
SEPTIC ARTHRITIS :

Joint Aspiration :
- Needle joint aspiration can be used as both a diagnostic tool and a treatment. A portion of the fluid can be taken out by aspiration needle to determine the type of bacteria causing the infection thus determining further course of treatment.
Other Diagnostic Lab Values :
1.Arthrocentesis with synovial fluid examination and culture
2.Increased White blood cell count
3.Increased Erythrocyte sedimentation rate (ESR)
4.Increased Temperature
5.Increased C-Reactive Protein (CRP)
6.Imaging studies are used to rule out other conditions
ULNAR NERVE ENTRAPMENT :
Diagnostic Tests for Ulnar Nerve Entrapment :
- Imaging for OA, bone spurs, or bone cysts .
- Nerve Conduction Studies (EMG).
- If fracture/dislocation is suspected, plain film x-ray.
PHYSIOTHERAPY EXAMINATION :
MEDIAL EPICONDYLITIS :
Subjective Assessment :
- Tenderness to palpation (usually over pronator teres and flexor carpi radialis) .
- Local swelling and warmth.
Objective Assessment :
- Range of motion in the beginning of the disease can be full, but later on there is a possibility of a decreased range of motion
- .An evaluation of the entire upper extremity kinetic chain can be needed.
- A particular focus goes to the shoulder and the scapular strength, motion and stabilisation.
- Overuse injuries in the elbow often occur with shoulder or scapular dysfunction.
Medial epicondylopathy test :
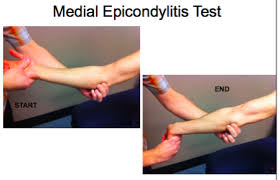
Technique :
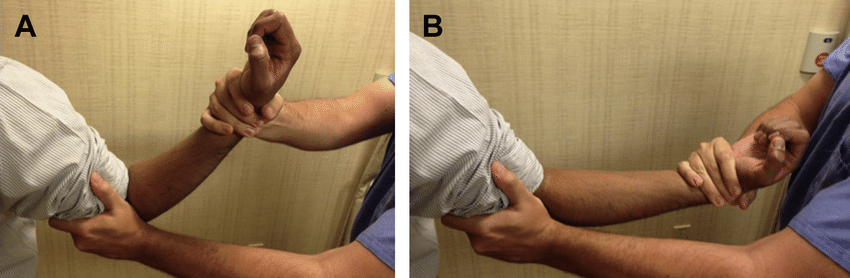
Passive Technique :
- Position: The patient can be seated or standing for this test.
- Procedure: The therapist palpates the medial epicondyle and supports the elbow with one hand, while the other hand passively supinates the patient’s forearm and fully extends the elbow, wrist and fingers.
- Interpretation: If sudden pain or discomfort is reproduced along the medial aspect of the elbow in the region of the medial epicondyle, then this test is considered positive.
*Active Technique :
- Position: The patient seated for this test.
- Procedure: Patient flex the elbow, turns the hand palm up (forearm supination). The examiner then grasps the patient’s wrist and elbow and attempts to straighten out the elbow (forced extension) against the patient’s resistance (resisted elbow-wrist flexion).
- Interpretation: If sudden pain or discomfort is reproduced along the medial aspect of the elbow in the region of the medial epicondyle, then this test is considered positive.
LATERAL EPICONDYLITIS :
Subjective Assessment :
- Onset of pain 24-72 hours after provocative activity involving wrist extension .
- Pain may radiate down forearm as far as the wrist and hand .
- Difficulty with lift and grip (Pain+/- weakness) .
- Changes in biomechanical factors- new tennis racquet, wet ball, over training, poor technique, shoulder injury .
Objective Assessment :
- Pain and point tenderness over lateral epicondyle and/or 1-2 cm distal to epicondyle.
- Pain and weakness on resisted wrist extension.
- Weakness on grip strength testing (Dynamo-meter).
- Pain and/or decreased movement on passive elbow extension, wrist flexion and ulnar deviation and pronation.
- Weak elbow extensors and flexors.
Cozen’s test :
- Cozen’s test is also known as the resisted wrist extension test.
- The elbow is stabilized in 90° flexion. The therapist palpates the lateral epicondyle and the other hand positions the patient’s hand into radial deviation and forearm pronation. Then the patient is asked to resist wrist extension.
- The test is positive if the patient experiences a sharp, sudden, severe pain over the lateral epicondyle.
Chair test :
- The patient grasps the back of the chair while standing behind it and attempts to lift the chair by using a three finger pinch (thumb, index long fingers) and the elbow fully extended.
- The test is positive when pain occurs at the lateral epicondyle.
Mill’s Test :

- The patient is seated with the upper extremity relaxed at side and the elbow extended.
- The examiner passively stretches the wrist in flexion and pronation.
- Pain at the lateral epicondyle or proximal musculotendinous junction of wrist extensors is positive for lateral epicondylitis.
Maudsley’s test :
- The examiner resist extension of the third digit of the hand, while palpating the lateral epicondyle.
- A positive test is indicated by pain over the lateral epicondyle.
The coffee cup test (by Coonrad and Hooper) :
- While doing a specific activity such as picking up a full cup of coffee or a milk bottle. The patient is asked to rate their pain on a scale of zero to ten.
BURSITIS :
Bursal inflammation’s most classic finding is a swelling, at the posterior elbow.
- This swelling is clearly marked off by its appearance as a goose egg over the olecranon process.
- There may be a tenderness for palpation at the affected site. Cases in which infection is present may show a warm and red affected area.
- If the trauma has recently occurred, the inspection of the skin may reveal abrasion or contusion.
- Generally a patient with advanced infection, can have fever.
- The Range of motion (ROM) of the affected elbow is usually normal but now and then it is possible that the end-range of elbow flexion is slightly limited due to pain.
- Patients suffering from systematic inflammatory processes (like rheumatoid arthritis) or crystal – deposition disease (like gout or pseudogout) may reveal evidence of focal inflammation at other sites.
- When you exam a patient who has rheumatoid arthritis, it is possible that you can see rheumatoid nodules during inspection of the elbow.
- If the patient reports elbow pain during active or passive ROM and if a history of trauma exists, this may increase the clinical suspicion of an olecranon process fracture.
OSTEOARTHRITIS :
Observation of the upper extremity with comparisons to contralateral side. Look out for deformity, swelling, and muscle atrophy.
Range of motion, Conisder joints above and below.
Neurovascular examinaton, the ulnar nerve is commonly effected.
Ligamentous stability, varus, and valgus test of collateral ligaments are commonly performed.
VALGUS STRESS TEST :
Purpose :
The elbow valgus stress test is used to assess the integrity of the medial collateral ligament, also known as the ulnar collateral ligament.
Technique :
- This test can be performed with the patient supine, sitting, or in the standing position.
- The therapist places the patients elbow in approximately 20 degrees of flexion while palpating the medial joint line and stabilizing the distal humerus with one hand and applying a valgus stress to the elbow with the other hand.
- The test is considered positive if the patient experiences pain or excessive laxity is noted compared to the contralateral side.
- As with the varus stress test, this test can be repeated in varying degrees of elbow extension to test different portions of the MCL.
VARUS STRESS TEST :

Purpose :
The purpose of the varus stress test of the elbow is to assess the integrity of lateral collateral ligament.
Technique :
- With the patient is standing, the therapist places the patient’s elbow in slight flexion while palpating the humeroulnar joint line. and the therapist then applies a varus force to the elbow.
- This test is considered positive if the patient experiences pain or excessive laxity is noted and compared to the contralateral side.
- The test can be repeated in varying degrees of elbow flexion, but generally it is positioned between 5 and 30 degrees.
DISLOCATION OR FRACTURE :
- Observation – specifically deformities.
- Vascular screen – palpation of brachial, radial and ulnar arteries.
- Neuromuscular screen – dermatomes, myotomes and reflexes including upper limb neuro-tension tests (if tolerated by patient).
- Palpation – It is essential to palpate for associated fractures in the elbow complex.
- The elbow extension sign can be used to rule out a fracture.
- ROM
- Muscle testing
- Ligament integrity tests – varus and valgus stress test, the lateral pivot-shift test/ apprehension test (Posterolateral Rotational Instability Test).
Posterolateral Rotary Drawer Test :
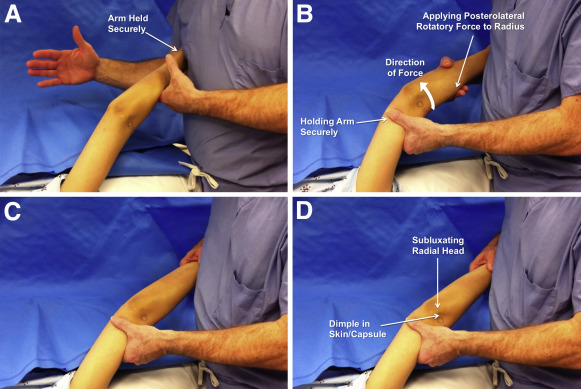
- Supine with arm overhead. Elbow is flexed to 400.
- Clinician applies an anterior to posterior force to the radial and ulna with the forearm in external rotation.
- Positive Test:-
- Under anesthesia- visible radial head dislocation; Dislocation occurs as the forearm subluxes away from humerus on the lateral side
Awake- Apprehension :
- *Alternate Descriptions of Posterolateral Drawer Test .
- Patient is in a seated position with elbow flexed slightly and clinician gives a posterolateral drawer and supination force to the proximal forearm.
- The test is done at 300 and 900 of elbow flexion. Clinician stabilizes the humerus and gives a superior and inferior force to the forearm.
- NOTE: This test is not as sensitive as the pivot shift test for diagnosing PLRI .
ELBOW SPRAIN AND STRAIN :
- Although ligamentous injuries are rare, patients may present with varus or valgus laxity due to overuse or trauma. –
- Lateral Collateral Ligament injury is often associated with trauma and forceful motion into varus.
- These injuries are commonly associated with a fracture or subluxation at the elbow joint.
- An Ulnar Collateral Ligament tear or sprain could occur with valgus overload or stress movement from pitching or throwing.
- Typically seen in younger male pitchers, a UCL tear or sprain could also be found in athletes involved in repetitive overhead activities like tennis or volleyball.
OSTEOCHONDRITIS DISSECANS :
Subjective assessment :
- Complaints of aching post exercise or activity
- Gradually worsening symptoms
- Reported crepitus or popping
- Increase in sport recently
Objective assessment :
- Swelling posterior-laterally
- Loss of full extension
- Lateral elbow joint pain
- Positive response to valgus overload
- Crepitus or popping (indicating osteochondral defects)
Positive radio-capitellar compression test:

- full extension with active pronation and supination.
- Positive test will reproduce lateral pain
CELLULITIS :
- Patients with cellulitis will reveal an affected skin area typically with a poorly demarcated area of erythema.
- The erythematous area is often warm to the touch with associated swelling and tenderness to palpation.
- The patient may present with constitutional symptoms of generalized malaise, fatigue, and fevers.
- Ask for a complete history of the presenting illness, focusing on the context in which the patient noticed the skin changes or how the cellulitis began to occur.
- It is essential to ask patients if they: recently traveled, experienced any trauma or injuries, have a history of intravenous drug use, and/or have had insect or animal bites to the affected area.
- A complete and thorough past medical history should additionally be conducted to evaluate for possible chronic medical conditions that predispose patients to cellulitis, such as diabetes mellitus, venous stasis, peripheral vascular disease, chronic tinea pedis, and lymphedema.
- Diabetes Mellitus is one of most common comorbidities among those hospitalized for acute bacterial infections including cellulitis.
- Following a cellulitis infection, those with diabetes require a longer course of antibiotic therapy and more likely to have an outpatient follow-up visit.
- Inspected area to look for any area of skin breakdown. The area should be demarcated with a marker to monitor for continuous spread.
- The area should be palpated to feel for fluctuate that could indicate the formation of a possible abscess.
- Gently palpate the affected area, be sure to note any presence of warmth, tenderness, or purulent drainage.
- Cellulitis can present on any area of the body. It is rarely bilateral.
- Check for proper sensation and verify pulses are intact to monitor closely for compartment syndrome.
- Note if there are developing vesicles, bullae, or the presence of peau d’orange and lymphadenopathy.
ULNAR NERVE ENTRAPMENT :
Guyon’s Canal Syndrome:
- It is important t rule out other diagnoses which could refer to the elbow.
Physical examination :
- ROM of the wrist and digits.
- MMT of ulnar nerve muscles innervated distal to Guyon’s Canal .
- Sensory exam of the ulnar nerve cutaneous distribution distal to Guyon’s Canal.
- Muscle wasting of intrinsic hand muscles.
Special Tests :
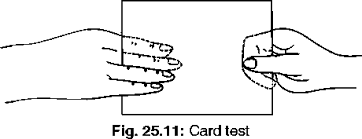
Card test :
Froment’s Sign
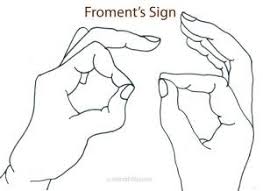
Purpose :
- Froment’s sign is a physical examination of the hand to test for palsy of the ulnar nerve which results in reduced functionality and muscle weakness of the pinch grip.
- It tests the strength of the adductor pollicus of the thumb, which is innervated by the ulnar nerve and is weakened in ulnar nerve palsy.
- Froment’s sign presents after damage to the ulnar nerve, which innervates the adductor pollicis and interossei muscles, which provide adduction of the thumb and extension of the interphalangeal joint.
- The flexor pollicis longus (innervated by the median nerve), will substitute for the adductor pollicis (innervated by the ulnar nerve) and cause the thumb to go into hyperflexion. Ulnar nerve palsy can be as a result of dysfunction at the cervical spine, elbow (cubital tunnel syndrome) or at the wrist (Guyons canal syndrome).
Technique :
- The patient is asked to make a strong pinch between the thumb and index finger and grip a flat object such as a piece of paper between the thumb and index finger.
- The examiner then attempts to pull the object out of the subject’s hands.
- There is weakness of the adductor pollicus innervated by the ulnar nerve which would keep the IP joint relatively straight; instead, the FPL muscle which is innervated by the median nerve is substituted for the AP and will cause the IP joint to go into a hyperflexed position.
- Similar to Froment’s sign, Jeanne’s sign indicates ulnar nerve palsy and is also seen in response to pinch forces. Instead of isolated thumb IP flexion, the IP flexion is accompanied by MP joint hyperextension.
Tinnel’s sign at Guyon’s canal :

Purpose :
Tinel’s sign is a way to detect irritated nerve .
Technique :
- It is performed by lightly tapping (percussion) over the nerve to elicit a sensation of tingling or “pins and needles” in the distribution of the nerve.
- It takes its name from French neurologist Jules Tinel (1879-1952).
- The test is positive when there is pressure neuropathy of the nerve, like in the foot or ankle, or in the hand.
- When the nerve is not trap behind a structure there will be a negative test and the patient will feel no pain.
- On the opposite when the nerve is trap the patient will feel tingling’s in the distal area.
- When the nerve is trap in the tarsal tunnel the sign can be called by tapping whit a reflex hammer just behind the medial malleolus.
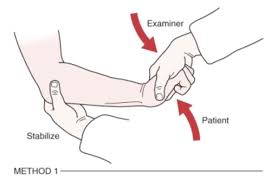
Ulnar neurodynamic test (ULTT3) :
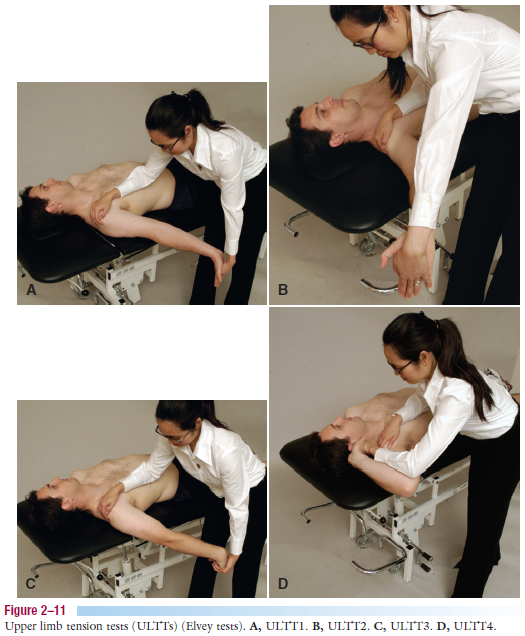
- The Upper Limb Tension Tests (ULTTs) are also known as Brachial Plexus Tension or Elvey Test.
- These tests are designed to put stress on neurological structures of upper limb.
- These tests were first described by Elvey and hence also known as Elvey test but most commonly called ULTT.
- The shoulder, elbow, forearm, wrist and fingers are kept in specific position to put stress on particular nerve (nerve bias) and further modification in position of each joint is done as “sensitiser”.
- The ULTT’s are equivalent to the straight leg raise designed for the lumbar spine.
Purpose :
- These tension tests are performed to check the peripheral nerve compression or as a part of neurodynamic assessment.
- The main reason for using a ULTT is to check cervical radiculopathy. These tests are both diagnostic and therapeutic.
- Once the diagnosis of cervical radiculopathy is made the tests are done to mobilise the entrapped nerve.
Method :
- Each test is done on the normal/asymptomatic side first.
- Traditionally for the upper limb, the order of joint positioning is shoulder followed by forearm, wrist, fingers, and lastly elbow.
- Each joint positioning component is added until the pain is provoked or symptoms are reproduced. To further sensitive the upper limb tests, side flexion of cervical spine can be added.
- If pain is provoked in the very initial position, then there is no need to add further sensitisers.
- If pain or sensations of tingling or numbness are experienced at any stage during movement into the test position or during addition of sensitisation manoeuvres, particularly reproduction of neck, shoulder or arm symptoms .
- The test is positive; this confirms a degree of mechanical interference affecting neural structures.
Upper Limb Tension Test 3 (ULTT3, Ulnar nerve bias) :
- Shoulder girdle depression
- Shoulder abduction
- Shoulder external rotation
- Wrist and Finger extension
- Elbow flexion
- Shoulder abduction
TREATMENT :
Once you begin, keep the following tips in mind:-
- Be gentle and stop if you feel sharp pain.
- Avoid overstretching or exercising too much when recovering from an injury.
- Talk to your healthcare provider if your pain doesn’t improve or gets worse, or if there’s increased swelling or redness around your elbow.
MEDICAL MANAGEMENT :
MEDIAL EPICONDYLITIS :
Steroid Injections :

- The indication for injection therapy for epicondylopathy is usually chronic pain and disability not relieved by more conservative means, or severe acute pain with functional impairment that calls for a more rapid intervention.
- These injections seem to have a short term effect (2-6 weeks) and effective in providing early symptom relief .
- The injection must be in the proper location for maximal benefit to the patient.
*Autologous Blood Injection :
- The combined treatment of dry needling and ultrasound guided autologous blood injection is described as an effective way to treat patients with refractory lateral and medial epicondylopathy.
- There was a significant decrease in the VAS pain scores.
- The hypothesis of the mechanism is that the transforming growth factor-ß and basic fibroblast growth factor carried in the blood act as humoral mediators to induce the healing cascade.
Extracorporeal Shock Wave Therapy :

- Extracorporeal shock wave therapy is effective for the patients with newly diagnosed as lateral or medial epicondylopathy.
- This can be another option when local steroid injection is contraindicated in the treatment of the patient .
- The pressure-focused pulses may cause tissue regeneration at the specific site.
- This method can also be used when there is presence of recalcitrant chronic epicondylopathy.
LATERAL EPICONDYLITIS
- Non-Operative medical management of lateral epicondylitis is initially based on the following principles: relieving pain and controlling inflammation.
- Relieving pain can be countered by rest and avoiding painful activities.
- Inflammation on the other hand can be prevented by NSAIDs in the acute cases.
- The use of ice three times per day for 15 minutes is also recommended because it reduces the inflammatory response by decreasing the level of chemical activity and by vasoconstriction, which reduces the swelling.
- Elevation of the extremity is also indicated if an oedema of the wrist or fingers is present.
Elbow counterforce brace :
- The use of an elbow counterforce brace can be helpful because it plays the role of a secondary muscle attachment site and relieves tension on the insertion at the lateral epicondyle.
- The brace is applied around the forearm (below the head of the radius) and is tightened enough so that, when the patient contracts the wrist extensors, he or she does not fully contract the muscles.
Injection :
- Injections should be given subperiosteally to the extensor brevis origin. These injections have an early and beneficial effect.
- During the initial 24-28 hours, increased pain be experienced. A steroid injection should be followed by 1-2 weeks’ rest and should not be repeated more than 2 times. Steroid injection seems to be effective for about 3 months, indicating that the patient must continue with the exercise program.
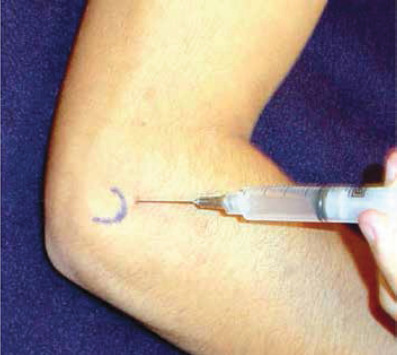
BURSITIS :
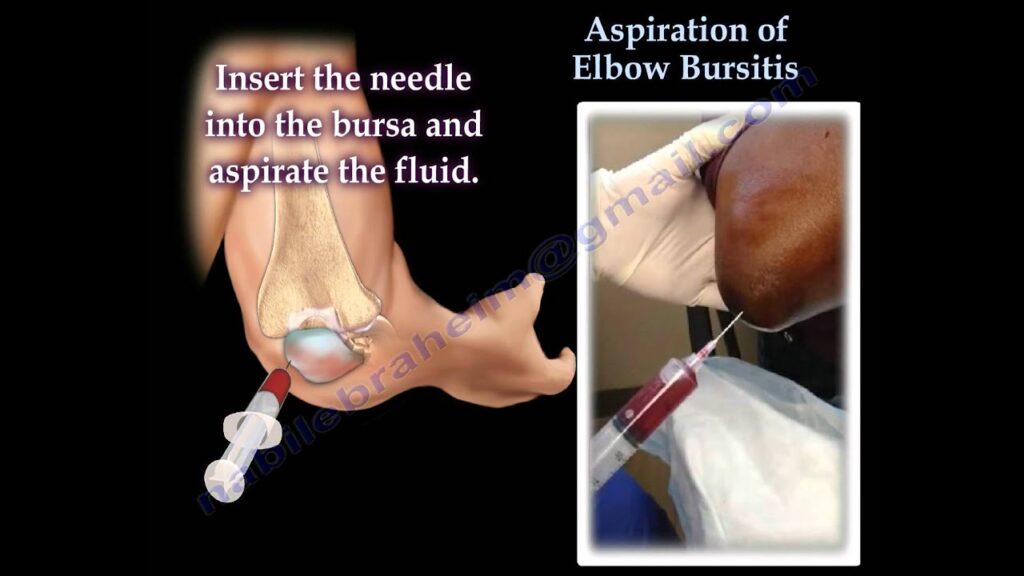
- Step 1 : involves aspiration of the bursa with an 18-gauge needle.
- Step 2 : a mixture of 80-mg methylprednisolone and 2% lidocaine (specifically 1 mL of methylprednisolone and 1.5 mL of lidocaine without adrenaline) is injected into the elbow joint from a lateral approach.
- Step 3 : involves the application of a dry gauze dressing, followed by the application of a tensor bandage or elbow brace for a period of 3 to 6 months.
- The technique was discovered over 3 to 4 years, with 4 or 5 cases being treated per month. Follow-up with each patient occurred at 2 weeks, 3 months, and 6 months.
- At each follow-up visit, side effects, pain assessment, and limitation of function (including warmth, degree of swelling, and tenderness) were assessed and recorded.
- The typical pain, skin atrophy, and corticosteroid-induced side effects mentioned by some authors 1–5 were not observed in any of these cases.
- In addition, none of my patients who used this technique developed septic bursitis or tendon rupture.
*Other treatments that have been suggested in the past for nonseptic olecranon bursitis include the following:
- Bursal aspiration alone, with or without compressive dressings;
- Conservative approach;
- Nonsteroidal anti-inflammatory drugs for 10 to 14 days;
- Corticosteroid injections alone, after aspiration;
- A “blood patch” injection;
- The temporary 3-day use of a percutaneous-intrabursal drainage catheter;
- Holding a needle in place with a hemostat, if aspirating and injecting;
- Intrabursal injections of tetracycline and talcum powder.
OSTEOARTHRITIS :
- Non-operative management is the predominant initial treatment for both forms of osteoarthritis of the elbow.
- Medicines management can include nonsteroidal anti-inflammatory analgesia and intra-articular corticosteroid injections.
- Patients may find sleeves or compression bandages useful for comfort.
- There is a paucity of literature regarding physiotherapy management of elbow OA.
- However, principles of OA rehabilitation used at other joints are likely to be effective with the elbow.
- The most common approach is a combination of exercise therapy and education.
- Manual therapy could be considered.
- On failing conservative management surgery can be considered.
DISLOCATION AND FRACTURE OF ELBOW :
- Before surgery is considered, research indicates reduction under local or general anaesthetic as the primary treatment for PED.
- Radiographs are indicated when there is no response to care after four weeks of conservative treatment, significant activity restriction for more than four weeks, or non-mechanical pain is present.
LIGAMENT SPRAIN AND STRAIN :
- Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used for relief of pain and inflammation.
- If pain is severe, a mild narcotic or corticosteroid injections may be prescribed.
- Common impairments to assess in examination could include decreased elbow or shoulder range of motion, joint effusion, and decreased strength of the upper extremity musculature.
- Glenohumeral internal rotation deficits are typically seen with pitchers and athletes performing repetitive overhead activities.
- Studies have shown a direct correlation with decreased internal rotation and excessive external rotation in baseball pitchers and UCL injuries.
- It is recommended that individuals with these conditions remain active, while protecting the ligament from stress.
- Activities that aggravate the symptoms should initially be minimized in order to allow for ligaments healing.
- Activity level can thereafter be increased gradually.
- Pain and swelling may be relieved through the intermittent application of ice during the acute stages.
OSTEOCHONDRITIS DISSECANS :
- Analgesia and NSAIDs
- Bracing to offload the joint. In a hinged brace set to pain free range of movement (ROM)
- Ceasing sports or activities that aggravate symptoms for 6-12 week
- Activity modification
- Physiotherapy
- Conservative management may not always be successful even in Grade I lesions and should be re-assessed regularly.
CELLULITIS :
- Patients presenting with mild cellulitis and displaying no systemic signs of infection should be covered with antibiotics that target the treatment of streptococcal species.
- The duration of oral antibiotic therapy should be for a minimum duration of 5 days.
- In nonpurulent cellulitis, patients should receive cephalexin 500 mg every 6 hours.
- If they have a severe allergic reaction to beta-lactamase inhibitors, treat with clindamycin 300 mg to 450 mg every 6 hours.
- In patients with purulent cellulitis, methicillin-resistant staph aureus colonization, cellulitis associated with an abscess or extensive puncture wounds, or a history of intravenous drug use, patients should receive antibiotics that cover against methicillin-resistant staph aureus as well.
- Hospitalization with the induction of systemic antibiotics may be necessary for patients who: present with systemic signs of infection, have failed outpatient treatment, are immunocompromised, exhibit rapidly progressing erythema, are unable to tolerate oral medications, or have cellulitis overlying or near an indwelling medical device.
- If patients have significant edema with a known cause for the edema, the underlying condition should receive proper treatment to decrease the amount of edema and prevent future episodes of cellulitis.
- Patients should be instructed to keep the affected area elevated
SEPTIC ARTHRITIS :
- The course of treatment for septic arthritis is case dependent.
- There is no conclusive evidence on the most effective way to begin.
- However, it is a combination of antibiotics, joint fluid removal, infection drainage, and/or total joint surgery.
- The course of treatment also depends on the type of joint invasion (bacterial, STD bacterial, viral etc..).
- The first round antibiotics can be directed at the most likely pathogen, then the joint can be tested to see what further treatment may be necessary such as needle joint aspiration or drainage to release the fluid.
- Another option is to perform joint aspiration before a round of antibiotics is chosen.
- If the infection is severe enough following a round of antibiotics and aspiration for fluid removal, surgery or even replacement of the entire joint may be necessary.
Antibiotic Treatment :
- Ceftriaxone (Rocephin)- Effective against gram-negative enteric rods
- Ciprofloxacin (Cipro) – Treat N gonorrhoeae and gram-negative enteric rods.
- Cefixime (Suprax) –Broad activity against gram-negative bacteria, by binding to one or more of the penicillin-binding –
- proteins. Arrests bacterial cell wall synthesis and inhibits bacterial growth.
- Management regarding antibiotic choice, dosage, route of administration, and duration of treatment is unknown in the treatment of septic arthritis.
- In addition, no evidence has shown if closed aspiration or open arthroscopy is better at removing materials from a joint that’s infected.
SURGICAL TREATMENT :
MEDIAL EPICONDYLITIS :
Mini-open Muscle Resection Procedure Under Local Anesthesia :
- For medial epicondylopathy the degenerative tissue at the origin of the flexor carpi radialis brevis is removed during mini-open muscle resection procedure.
- This procedure produces low levels of postoperative pain, a short hospital stay and rehabilitation period and early return to daily activities.
- The limitations of and open flexor carpi radialis brevis release include late return to work and sporting activities due to a prolongation of the postoperative recovery time, a risk of posterolateral instability, and the formation of neuroma after surgery.
*Fascial Elevation and Tendon Origin Resection :
- Fascial elevation and tendon origin resection (FETOR) facilitates the complete visualization and resection of the CFP (Chronic Flexor Palmar Origin) with limited soft tissue dissection. FETOR decreases the average pain, pain at rest, and pain during hard work or heavy lifting.
- There is also an improvement of the mean pain-free grip strength.
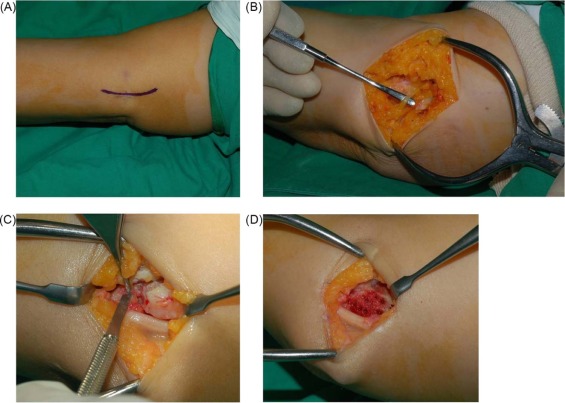
LATERAL EPICONDYLITIS :
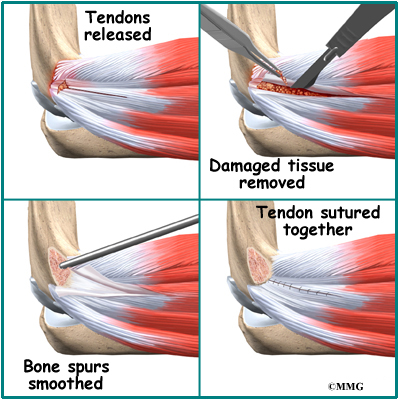
- If the symptoms of epicondylitis lateralis will prove to be resistant surgical treatment is indicated.
- Usually this is after a failed conservative treatment for more than 6 months.
- Most surgical procedures for tennis elbow involve removing diseased muscle and reattaching healthy muscle back to bone.
- The right surgical approach for you will depend on a range of factors. These include the scope of your injury, your general health, and your personal needs.
Open surgery:
- The most common approach to tennis elbow repair is open surgery. This involves making an incision over the elbow. Open surgery is usually performed as an outpatient surgery.
- It rarely requires an overnight stay at the hospital.
Arthroscopic surgery:
- Tennis elbow can also be repaired using tiny instruments and small incisions.
- Like open surgery, this is a same-day or outpatient procedure.
BURSITIS :
Surgery for Infected Bursa :
- If the bursa is infected and it does not improve with antibiotics or by removing fluid from the elbow, surgery to remove the entire bursa may be needed.
- This is often an inpatient procedure, meaning you will need to stay overnight in the hospital.
- This surgery may be combined with further use of oral or intravenous antibiotics.
- The bursa usually grows back as a non-inflamed, normally functioning bursa over a period of several months.
Surgery for Non-Infected Bursa :
- If elbow bursitis is not a result of infection, surgery may still be needed if nonsurgical treatments do not work.
- In this case, surgery to remove the bursa is usually performed as an outpatient procedure.
- The surgery does not disturb any muscle, ligament, or joint structures.
- Although formal physical therapy after surgery is not usually needed, there are specific exercises to improve your range of motion.
- These are typically permitted within a few days of the surgery.
OSTEOARTHRITIS :
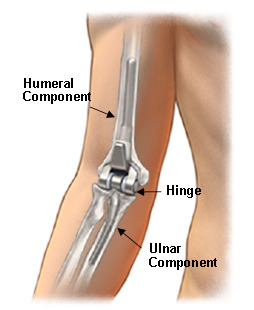
- Surgical debridement .
- Total elbow arthroplasty .
- Arthroscopic radial head resection
- Radiocapitellar arthroplasty .
DISLOCATION AND FRACTURE OF ELBOW :
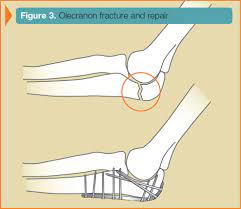
- The most common surgical options include an open procedure, and excision or closed arthroplasty.
- An open procedure, more likely when fractures are involved, can include:
- Ulnar nerve release,
- Humeroulnar reduction
- Humeroradial reduction,
- Triceps lengthening using Speed’s procedure
- Wires and/or screws placed in the olecranon for stabilising the joint.
- Ligamentus repairs with sutures
- Once surgery is complete, the patient is typically immobilised with time frames varying based on the individual and the surgeon’s protocol.
- Some patients may be allowed to actively move the elbow immediately post op, however this will depend on the surgeon.
LIGAMENT SPRAIN AND STRAIN :
Surgery for the UCL :

- Surgery for the UCL is indicated in complete tears and for athletes wanting to resume previous level of activity.
- The most common surgical procedure, Tommy John surgery, is when the UCL is replaced with a tendon from elsewhere in the body [often from forearm, hamstring, knee or foot of the same patient).
- This procedure is most common with athletes from several sports, most notably baseball.
Surgery to repair the LCL :
- Surgery to repair the LCL alone is rare and is typically associated with a fracture, dislocation, or subluxation of the elbow.
- Due to the decreased structural stability of the joint and ORIF may be considered at the discretion of the surgeon.
OSTEOCHONDRITIS DISSECANS :
Arthroscopic surgery :
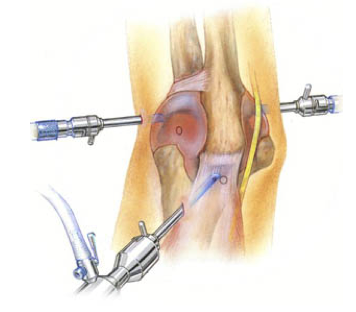
AIM :
- Assess the anterior elbow
- Remove loose bodies and fragments
- Debride any necrotic bone
- Mirco-fracture the site to stimulate increased blood flow
- In some cases a large fragment may need to be re-attached to the capitellum which will be done via K wire or screw fixation .
- In severe cases osteochondral grafting may be required.
SEPTIC ARTHRITIS :
- Joint Drainage and Surgical options are often used in combination with antibiotic treatment.
- Much like antibiotics, the choice of whether to use joint aspiration, arthroscopy, or total joint replacement is case dependent.
- There is no current definitive evidence on whether one treatment is more effective than the other.
- However, the most positive outcomes, in general, come from using one of these options.
- The main goal of this treatment is to continuously remove the accumulation of pus within the joint until it no longer forms.
- This is most commonly used in combination with the antibiotics to remove the pus both from the joint itself and via the bloodstream.
ULNAR NERVE ENTRAPMENT :
Surgical treatments can be divided into two types: –
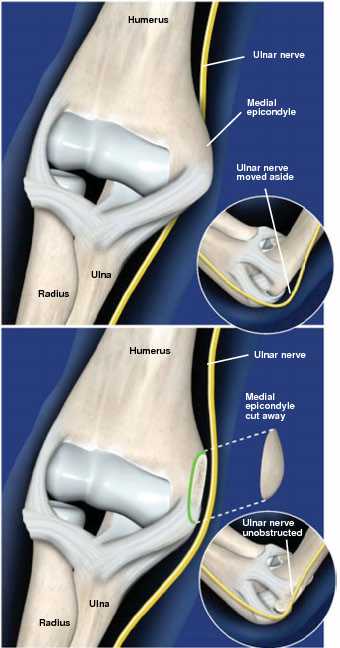
- Decompression without transposition (in-situ ulnar nerve decompression and medial epicondylectomy)
This outpatient procedure, performed under general or regional anesthesia, removes the medial epicondyle (the bony bump on the inner side of the elbow) to alleviate compression of the ulnar nerve. Medial epicondylectomy is used to treat cubital tunnel syndrome .
- Decompression with anterior transposition (subcutaneous, intramuscular, and submuscular).
Ulnar nerve transposition is a procedure performed to move the ulnar nerve from behind the medial epicondyle to a suitable position where it is not irritated or pinched by this bony prominence.
PHYSIOTHERAPY TREATMENT :
MEDIAL EPICONDYLITIS :
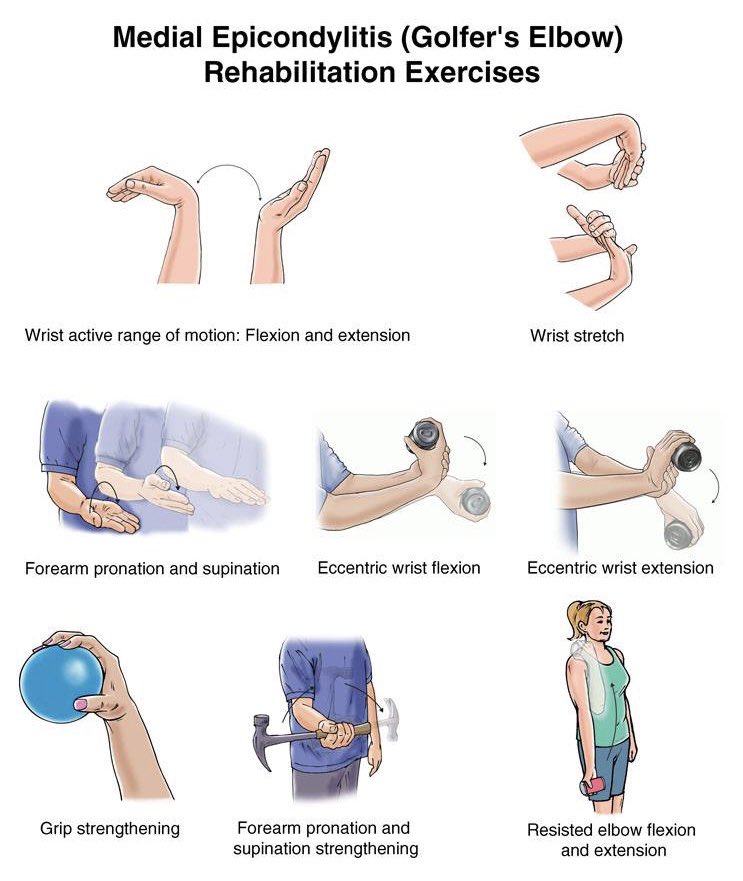
- The main goal of the conservative treatment is to relieve pain and reduce inflammation.
- These two things will help to achieve a proper rehabilitation and later, a return to usual activities.
- Nonsurgical treatment can be divided into three phases:
*Phase 1 :
- The patient immediately has to stop the offending activities.
- It’s not recommended to stop all activities or sports since that can cause atrophy of the muscles.
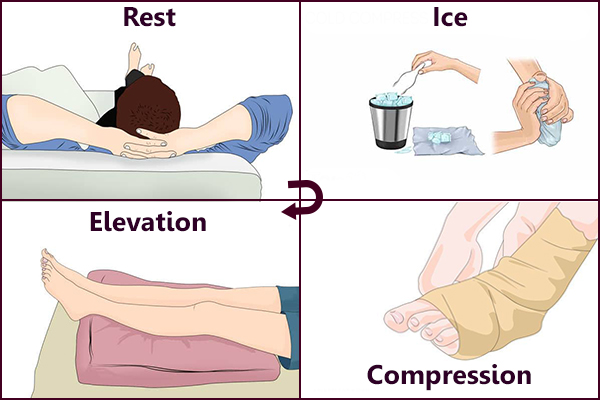
- The therapy starts with ‘PRICEMM’, which stands for ‘prevention/protection, rest, ice, compression, elevation, modalities and medication’.
- The affected elbow should be iced several times a day for about a quarter
- This improves the local vasoconstrictive and analgesic effects.
- As for medication the patient can take nonsteroidal anti-inflammatory medication (NSAID).
- If the patient’s condition doesn’t improve, a period of night splinting is adequate
- This is usually accompanied with a local corticosteroid injection around the origin of the wrist flexor group.
- Some examples of a physiotherapy modality are ultrasound and high-voltage galvanic stimulation (but there’s not yet a study that notes their efficacy).
- Counterforce bracing is recommended for athletes with symptoms of medial epicondylopathy .
- It can also aid when the patient is returning to sport.
*Phase 2 :
- As soon as we see an improvement of phase 1, a well guided rehabilitation can be started.
- The first goal of the second phase is to establish full, painless, wrist and elbow range of motion.
- This is soon followed by stretching and progressive isometric exercises.
- These exercises first should be done with a flexed elbow to minimize the pain.
- Although not yet conclusive, is the belief that strength training decreases symptoms in tendinosis.
- The short-term analgesic effect of manipulation techniques may allow more vigorous stretching and strengthening exercises resulting in a better and faster recovery process of the affected tendon in Medial epicondylopathy.
- As soon as the patient has made some progress the flexion of the elbow can be decreased.
- As the flexibility and the strength of the elbow area return, concentric and eccentric resistive exercises are added to the rehabilitation program.
- The final part of this phase is a simulation of sport or occupation of the patient.
- There is an evidence that supports the usage of Muscle Energy Techniques (METs) to improve ROM .
- METs are relatively pain-free techniques that could be used in clinical practice for restricted range of motion (ROM).
*Phase 3 :
- When the patient is able to return to his sport it is necessary to take a look at his equipment and/or technique.
- The precautions ought to be taken to allow a safe return to activities.
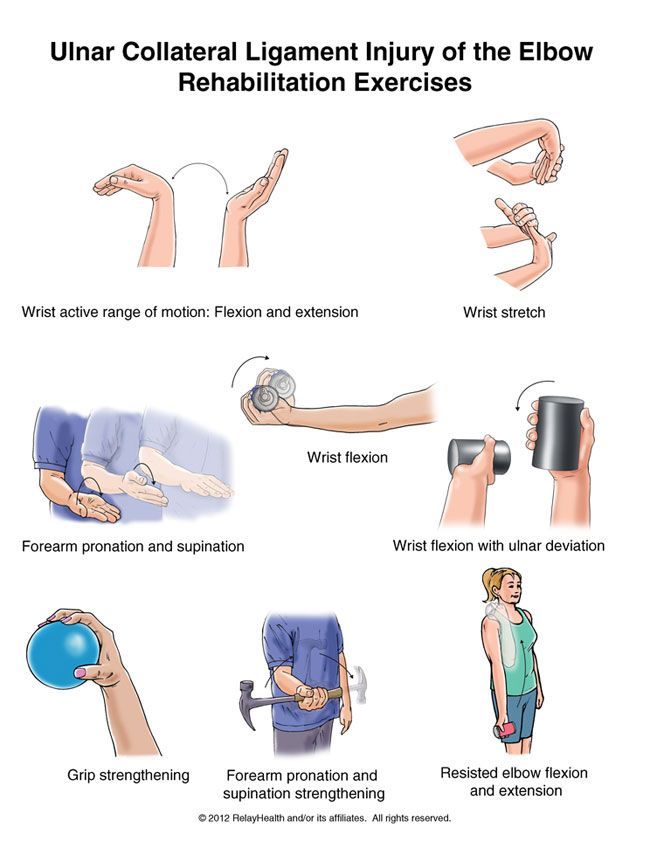
*Postoperative Management :
- Seven to ten days after the operation, the splint and skin sutures are removed.
- At this point the physical therapy can start.
- The beginning of the treatment is characterized by gentle passive and active hand, wrist and elbow exercises.
- 3 to 4 weeks later gentle isometrics can be done and at 6 weeks the patient can start with more resistive exercises.
- At last a progressive strengthening program has to be followed.
- In normal cases the patient can return to activities 3 to 6 months after the operation.
- short-term effectiveness was found in favour of stretching plus strengthening exercises versus ultrasound plus friction massage.
- Moderate evidence for short-term and mid-term effectiveness was found for the manipulation of the cervical and thoracic spine as add-on therapy to concentric and eccentric stretching plus mobilisation of wrist and forearm.
LATERAL EPICONDYLITIS :
- There are different types of therapies to treat lateral epicondylitis, all with the same aim: reduce pain and improve function.
General physiotherapy management includes:
- Education/Advice- on pain control and/or modification of activities
- Manual therapy- Mulligan – Mobilisation with movement
- Exercises- Strengthening and Stretching
- Modalities- Ultrasound, Transcutaneous electrical nerve stimulation (TENS)
- Braces/Splints/Straps- No clear evidence
- Medications- NSAIDs offer a short term benefit (3-4 weeks pain relief)
- Corticosteroids injection- Short term effect (<6 weeks)
- Sport/Occupation Specific Rehabilitation
Extracorporeal Shockwave therapy :

- Shockwave Therapy is a method of treatment for multiple tendonopathies that can be used for the treatment of lateral epicondylitis.
- ESTW is a treatment technique in which patients are exposed to a strong mechanical wave impulses which can be used on a fairly accurate position , the effects of extracorporeal shockwave on lateral epicondylitis.
- Statistical analysis of visual analogue scale (VAS), disabilities of the arm, shoulder, and hand (DASH) questionnaire and pain-free grip strength test scores has shown, both after treatment and to the follow-up at 6 months.
- The use of RSWT allowed a decrease of pain, and functional impairment, and an increase of the pain-free grip strength test, in patients with tennis elbow.
Deep Transverse Frictions :
- Deep transverse friction is a specific type of connective tissue massage applied precisely to the soft tissue structures.

- The therapist must try to reach an analgesic effect applying the DTF at the point of the lesion for 10 min till a numbing
- Effect has been reached, that all for preparing the tendon for Mill’s manipulations.
- Pain during the friction massage is considered as a wrong indication.
- In interval of 48 hours between two sessions is necessary.
- The purpose of the deep friction massage is to maintain the mobility within the soft tissue structures.
- It seems to have a pain relief function, due to modulation of the nociceptive impulses (gate control theory), a better alignment of connective tissue fibrils, softens the scar tissue, and blood flow increases.
- The patient should be positioned with arm fully supinated in 90° of elbow flexion, identify the area of tenderness on the lateral epicondyle and apply pressure (DTF), with the tip of the thumb on the lateral epicondyle, in a posterior direction on the teno-osseous junction.
- The other hand stabilized the patient’s wrist.
- This manipulation may produce mild discomfort at the instant of its performance.
- The clinician applies this procedure a 2-3 times a week until cure, with a range of 4-12 sessions.
Exercise therapy :
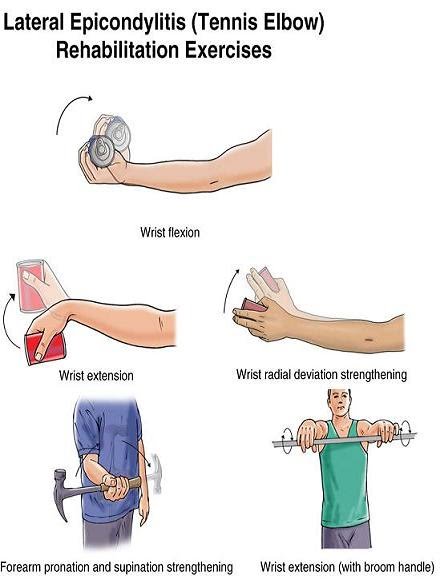
- Exercise therapy is a regimen or plan of physical activities designed and prescribed for specific therapeutic goals.
- Its purpose is to restore normal musculoskeletal function or to reduce pain caused by diseases or injuries.
- Strength, stamina and mobility should be improved by exercises once the pain and inflammation are under control.
Stretching :
- The literature on the treatment of a Lateral Epicondylitis suggests that strengthening and stretching exercises are the most important components of exercise programmes, for the reason that tendons should not only be strong but also flexible.
- The stretching exercises are intended to improve the flexibility of the extensor group of the wrist.
- These exercises ought to be instituted and continued until the range of motion of the wrist is the same as that of the uninvolved side
- The underlying principle of the stretching phase is that , by lengthening the tendon during relaxation, we can reduce its stretching during offending movements.
- The best stretching position for the Extensor Carpi Radialis Brevis tendon, is reached with the elbow in extension, forearm in pronation, wrist in flexion and with ulnar deviation of the wrist, according to the patient’s tolerance.
- This stretching should be held for 30- 45 s and 3 times before and after the eccentric exercises, during each treatment session with a 30 s rest interval.
- Other programs says that stretching exercises for the extensor muscles of the wrist and fingers should be performed in
- the following manner: fully extend the elbow and palmary flex the wrist.
- Remain in the point of maximum non painful extension for a period of 15 to 25s.
- This exercises is repeated four to five times a day with two series of ten exercises in each session: the patient should always stop at the first sign of pain. In this phase of therapy, the patient should also perform isotonic exercises, once a day, according to the following plan:
- Stretching exercises = repeat 10 times (15-25 seconds)
- Isotonic exercises = repeat 15 times (3 series)
- Stretching exercises = repeat 10 times (15-25 seconds)
- Icing = massage the tender area with ice or crushed ice for 10-15 minutes
Eccentric exercises :
- There are three principles of eccentric exercises. These are load ( resistance), speed (velocity) and frequency of contractions.
- Load ( resistance): Increasing the load ensures the tendon is subjected to greater stress and forms the fundamental basis of the progression of the exercise programme.
- The basis of all physical training programmes is formed by this principle of progressive overloading.
- According to the patient’s symptoms, it is important that the load of these eccentric exercises should be increased.
- If it’s not increased then the possibility of re-injury will be high.
- *Speed ( velocity): The speed (velocity) of contractions is also a fundamental principle of successful eccentric exercises.
- In each treatment session the speed of the eccentric training should be increased. Hence the load on the tendon increases to stimulate the mechanism of the injury. However the therapists must ensure that the patients perform the eccentric
- exercises slowly to avoid pain.
- *Frequency of contractions: The frequency of contractions is the third principle of eccentric exercises.
- There can be variations of sets and repetitions in the literature.
- According to the therapists 3 sets of 10 repetitions can normally be performed without overloading the injured tendon, as determined by the tolerance of the patient.
- The elbow is in full extension, forearm in pronation and the arm is supported. The greatest strengthening result for the extensor tendons of the wrist is reached in this position.
- This is a recommendation and the frequency must be patient specific.
Theraband Exercise:
- Theraband exercises (or exercises with a small weight) are performed each day for 3 sets of 10. You fix one side of the theraband under you feet or another place and you take the other side in your hand or you have a small weight in your hand.
- The patient starts the exercise in wrist flexion, then he/she does a wrist extension and comes back to the start position very slowly.
- This exercise is an concentric en eccentric exercise for the wrist extensors.
- They concluded that supervised exercise consisting of static stretching and eccentric strengthening produced the largest effect in reducing pain, strenght and improving function. Once the patients can do this, they can progress to another colour of theraband or you increase the weight.
BURSITIS :
- Most of the time physical and occupational therapy are not necessary, but are often indicated to reduce recovery time.
- Patients who have often olecranon bursitis are recommend to apply the RICE method of treatment.
- Rice stands for Rest, Ice, Compression and Elevation. There are also other physical therapy modalities that could be helpful for reducing pain and inflammation.
- For example phonophoresis, electrical stimulation. However, most patients with olecranon bursitis don’t necessary need those modalities.
- The physical therapist can also take care of the patient education and present compensatory strategies for resting the involved upper extremity while healing takes place. When the patient shows no response to conservative treatment and his condition deteriorates, then surgery may be indicated.
- When a patient undergoes a bursal excision (bursectomy), there might be a recommendation for physical therapy after the operation for regaining or maintaining the ROM and strength of the elbow.
OSTEOARTHRITIS :
- Elbow arthritis treatment will often include physical therapy and aims to help you move better and relived pain.
- It can also help restore physical function and your fitness level. Physical therapy is a great addition to any recovery treatment and helps to make daily tasks and activities easier.
- Physical therapy for elbow arthritis often addresses the following issues :
Pain :
- Commonly done with the use of heat to increase circulation in the area promoting movement.
- Some ways physical therapist achieves this is via electric heating pads, paraffin, or warm water soaks.
- The use of dry rice in long sock microwaved and then placed on the affected joint.
Swelling :
- Ice is often the treatment of choice for addressing swelling as you can get ice packs that conform to various shapes making getting one that wraps around the unique contours of your elbow much easier.
- Most people, however, will find that a frozen bag of peas is satisfactory.
- An elastic compression sleeve, called a Tubigrip can also be effective for reducing pain and swelling.
Joint protection :
- This knowledge is important for prolonging the life of your joints. It often involves modifying the way an activity is performed or using an adaptive piece of equipment.
- The following principals can help protect not only your elbow joint but any joint of the body
Listen to your pain :
- When there is damage to your joint pain is often a sign of your body to stop doing that particular action.
- This may prompt you to change positions or change a particular tool .
- Use the largest joint available for the task: Larger joints are known to have more surface area to distribute pressure and handle increased loads.
- Examples of this may be, to use the side of your body to open a door instead of an extended arm or carry bags on your shoulder instead of in your hands.
Avoid staying in one position for extended periods of time :
- This can increase stiffness and pain. it is recommended to try alternating rest with activity.
- It important to keep in consideration that just as too much activity can cause pain, so can too much rest.
Elbow arthritis exercises :
- Putting your forearm on a table with your wrist and palm facing down, hold a canned food for weight in your hand.
- Now bend your wrist downwards and bring it up past parallel to the floor.
- It is recommended to perform 3 sets of 15 whiletaking 45-second breaks in between Bend your elbow at a rightangle. Hold a light weight(e.g. a tin of beans), palmup.
- Bend your wrist slowly towards you.
- Hold for 5 seconds, and then slowly release.
- Do 3 sets of 10 repetitions.
- Placing your wrist and arm on the edge of a table with palms facing upward, hold a canned food for within your hand, letting your wrist fall down towards the floor. Now bring it back up past parallel to the flow. Perform this exercise in 3 set of 15 repetitions .
Hand Extension :
- A great exercise for improving arthritis symptoms.
- It can be done by simply standing and stretching your hands forward, then turning the palms in a way so that your fingers are pointing to the sky and you look directly at your palms .
- Now make a fist by closing all your fingers into a fist and then open them as wide as possible, points all your fingers apart.
- Do this exercise at least 10 times with both hands.
Chest Press :
- Choosing a weight that is about 15 pounds or less, hold them at shoulder level.
- Now press the weight out towards your front and then back to starting position.
- Repeat 10 times
Arms Stretching in a Sitting Position :
- Using a yoga mat, sit comfortably stretching your arms over your head, then interlock the fingers with your palms facing forwards.
- Now take a deep breath, holding it for a couple of seconds, then exhale.
- Lower your arms until they come back to the level of the shoulders and repeat.
6]Arm Stretch for Relief in the Standing Position :
- Lift up your right arm, bend the elbow and put your palm on your upper back. Now try to bring the back side of the left hand towards the back, attempting to grasp the fingers of both hands firmly.
- How this position for about 30 seconds.
- If you are unable to connect both hands, using a towel can also be useful for attempting the stretch.
7]Elbow Arthritis Yoga Exercises :
While it is true that yoga can put you in many different exercise positions, many people believe that it may further damage the arthritic joints. However, yoga is something recommended by doctors for improving overall health and strengthening the joints. Yoga is known for providing relief from pain and stiffness.
DISLOCATION AND FRACTURE OF ELBOW :
- While conservative treatment approaches to PED can vary depending on the level of tissue involvement, there are key
- elements to consider throughout the clinical decision-making process.
- PED can occur on a continuum of severity; therefore, the treatment must be diverse as well.
- Treatment can vary from aggressive immediate AROM to traditional plaster immobilisation for several days depending on orthopaedic intervention.
- If a fracture occurs secondary to dislocation, intra-articular bone fragments and fracture position may dictate treatment.
- Following a typical reduction with no fracture:
- Immobilisation: typically involves the use of a posterior splint at 45-90 of elbow flexion for three days to three weeks.
- Throughout the immobilisation phase, wrist and shoulder function should be maintained through ROM and strengthening exercises.
- Inflammation is a common following PED and can be addressed using PRICE protocols.
- After the immobilisation phase physiotherapy begins with gentle AROM and PROM exercises in a pain-free range targeting the entire upper limb.
- When pain is no longer a barrier to treatment, functional progressive resistance exercises should be implemented to improve total upper limb muscle strength and endurance.
- Therapeutic goals in the later phase of rehabilitation include attaining full ROM and strength capabilities of the entire affected arm, suppression of pain, and restoration of functional abilities to pre-injury level.
- A patient is able to return to functional activities around twelve weeks and sports around six months.
LIGAMENT SPRAIN AND STRAIN :
- Damage to the medial collateral ligament of the elbow from an instability episode usually heals with non-operative treatment.
- In some cases, residual instability may occur, leading to a functional impairment.
- Non-operative management can be successful when bracing, taping and therapy are used to stabilise the elbow
- A recent report detailing the efficacy of platelet-rich plasma in effectively treating medial collateral ligament injuries in throwers has shown promise.
- However, there remain specific groups that should be considered for repair or reconstruction.
- These may include throwing athletes, wrestlers and some individuals involved in highly active physical activity which demands stability of the elbow.
- The results of surgical repair and reconstruction allowing a return to sports are quite good, ranging from 84% to 94%. Complications are generally low and mostly centered around ulnar nerve injuries.
- Rehabilitation program following ligament reconstruction using the docking procedure:
*Postoperative Phase 1: Weeks 1-4 :
Goals:
- Promote healing: reduce pain, inflammation, and swelling
- Begin to restore range of motion to 30-90°
- Independent home exercise program.
Precautions:
- Brace should be worn at all times
- No passive range of motion of the elbow
Treatment strategies:
- Brace set at 30° to 90° of flexion
- Elbow, active range of motion in brace
- Wrist, active range of motion
- Scapula isometrics
- Gripping exercises
- Cryotherapy
- Home exercise program
Criteria for advancement:
- Elbow, range of motion: 30°-90°
- Minimal pain or swelling
Postoperative Phase 2: Weeks 4-6
Goals:
- Range of motion: 15°-115°
- Minimal pain and swelling
Precautions:
- Continue to wear brace at all times
- Avoid passive range of motion
- Avoid valgus stress
Treatment strategies:
- Continue active range of motion in brace
- Begin pain-free isometrics in brace (deltoid, wrist flexion/extension, elbow flexion/extension)
- Manual scapula stabilization exercises with proximal resistance
- Modalities as needed
- Modify home exercise program
Criteria for advancement:
- Range of motion: 15°-115°
- Minimal pain and swelling
Postoperative Phase 3: Weeks 6-12
Goals:
- Restore full range of motion
- All upper extremity strength: 5/5
- Begin to restore upper extremity endurance
Precautions:
- Minimize valgus stress
- Avoid passive range of motion by the clinician
- Avoid pain with therapeutic exercise
Treatment strategies:
- Continue active range of motion
- Low-intensity/long-duration stretch for extension
- Isotonics for scapula, shoulder, elbow, forearm, wrist
- Begin internal/external rotation strengthening at 8 weeks
- Begin forearm pronation/supination strengthening at 8 weeks
- Upper body ergometer (if adequate range of motion)
- Neuromuscular drills
- Proprioceptive neuromuscular facilitation patterns when strength is adequate
- Incorporate eccentric training when strength is adequate
- Modalities as needed
- Modify home exercise program
Criteria for advancement:
- Pain-free
- Full elbow range of motion
- All upper extremity strength 5/5
Postoperative Phase 4: Weeks 12-16
Goals:
- Restore full strength and flexibility
- Restore normal neuromuscular function
- Prepare for return to activity
Precautions:
- Pain-free plyometrics
Treatment strategies:
- Advance internal/external to 90/90 position
- Full upper extremity flexibility program
- Neuromuscular drills
- Plyometric program
- Continue endurance training
- Address trunk and lower extremities
- Modify home exercise program
Criteria for advancement:
Complete plyometrics program without symptoms
- Normal upper extremity flexibility
Postoperative Phase 5: Months 4-9
Goals:
- Return to activity
- Prevent reinjury
Precautions:
- Significant pain with throwing or hitting
- Avoid loss of strength or flexibility
Treatment strategies:
- Begin interval throwing program at 4 months
- Begin hitting program at 5 months
- Continue flexibility exercises
- Continue strengthening program (incorporate training principles)
Criteria for discharge:
- Pain-free
- Independent home exercise program
- Independent throwing/hitting program
OSTEOCHONDRITIS DISSECANS :
Conservative :
- The initial stage should be focused on advice, education and pain management.
- This can be through use of NSAIDs, activity modification, cessation of sports and/or bracing for 6-12 weeks.
- Hinged elbow brace
- A hinged brace can be used to help offload the joint and any valgus pressure.
- This can be set to any pain free ROM and gradually increased as swelling and symptoms decrease.
- When pain has settled, management would be to gradually introduce full ROM and strengthening exercises out of a painful range.
- The patient can start return to play exercises as long as symptoms are not an issue.
Post-operative :
- Initially post operatively the patient would likely be on a continuous passive movement machine until put in a hinge brace.
- Gentle circulation and residual joint ROM exercises can be started (fingers, wrist and shoulder).
- At three weeks post operatively ROM and gradual strengthening may be commenced however; this may vary depending on consultant preference. Some post operative protocols state no strengthening exercises until three months.
- Return to play will depend on sport and pain. Athletes have the potential to return to their pre-injury level if motivation and compliance with rehabilitation allows.
CELLULITIS :
- While there is lack of evidence that discusses specific physical therapy interventions for cellulitis, therapists should be aware of the signs and symptoms in order to refer the patient appropriately.
- Physical therapists should have awareness of risk factors and various causes of cellulitis, in addition to signs and symptoms.
Modalities that physical therapists can use for a patient with cellulitis include :
- Rest and elevation of the affected limb is important and can help alleviate pain.
- The application of cool, wet, sterile bandages is also recommended for pain relief, and ice can be used as well.
- Preventative Measures
- Massage to promote lymphatic drainage, may help prevent cellulitis (not be used during an active cellulitis infection).
- Compression stockings
- Exercise promotion and specific exercises eg- elbow flexion and extension.
- Educate patients of the importance of maintaining good hand hygiene and adequately clean any future abrasions in their skin.
SEPTIC ARTHRITIS :
- The initial treatment of infectious arthritis is outside of the scope of physical therapy.
- It is important, first, for the physical therapist to recognize the signs and symptoms of the infection and refer out for other medical treatment.
- Subjective history, in combination with the physical therapist’s objective findings, is important in order to recognize the risk factors that make septic arthritis the likely diagnosis.
- It is important to immobilize the joint in this stage to best manage the patient’s pain and to decrease the likelihood of doing further damage to the joint until proper treatment can occur.
- Once the patient receives a round of antibiotic treatment in combination with either joint aspiration, debridement, or arthroscopy, the patient may then be referred back to physical therapy including educate on how to properly protect the affected joint.
- Gentle mobilization of the infected joint can begin if the patient is responding well following 5 days of medical treatment.
- Once the infection is well-managed, current evidence states the patient will usually respond best to aggressive physiotherapy to allow maximum post-infection functioning.
- Physiotherapy needs to consist of allowing the joint to be in its functional position and positioning the joint to allow
- passive range of motion activities.
ULNAR NERVE ENTRAPMENT :
- The Impairment-based approach can be used to address deficits in strength, ROM, and the attainment of functional goals .
- The source of the pain should be treated in conjunction with the impairments.
- Following treatment, reassess the functional task that produced pain to determine effective treatment outcome.
- Administer a home exercise program that aims to treat the same impairments and function tasks.
- In a study conducted by Svernlov and colleagues, three treatments were compared for individuals with cubital tunnel syndrome.
- All three groups had positive outcomes, with the control group improving just as much as the intervention groups .
Splint group protocol :
- An elbow brace was worn every night for a period of three months and the brace prevented elbow flexion beyond 45 degrees.
Nerve gliding protocol :
- Patients were instructed to complete nerve gliding exercises two times per day in six different. positions and hold them for 30 seconds for three repetitions with a 1-minute break in between each repetition.
- Patients were instructed to complete these exercises until the next visit, which occurred 1-2 weeks later.
- The frequency of the exercises were increased to three times per day, holding the exercise for one minute each day for a period of three months if there were no symptoms at the next visit.
Control group protocol :
- The control group only received education ,
- According to a case report by Coppieters and colleagues, joint mobilizations of the elbow, thoracic spine and rib thrust manipulations, and ulnar nerve sliding/tension techniques for six sessions were associated with improvements of decreased elbow pain and considerable improvement scores on a neck questionnaire up to a ten month follow-up.
Exercise 1 :
- Start with your arm extended straight and your palm up.
- Curl your fingers inward.
- Bend your elbow, bringing your curled fist up toward your shoulder.
- Return to your starting position.
- Repeat the exercise 3 to 5 times, 2 to 3 times a day.
Exercise 2 :
- Extend your arm out to the side at shoulder level, with your palm facing the floor.
- Flex your hand upward, pulling your fingers toward the ceiling
- Bend your elbow, bringing your hand toward your shoulders.
- Repeat the exercise slowly 5 times.
Nerve Gliding Exercises :
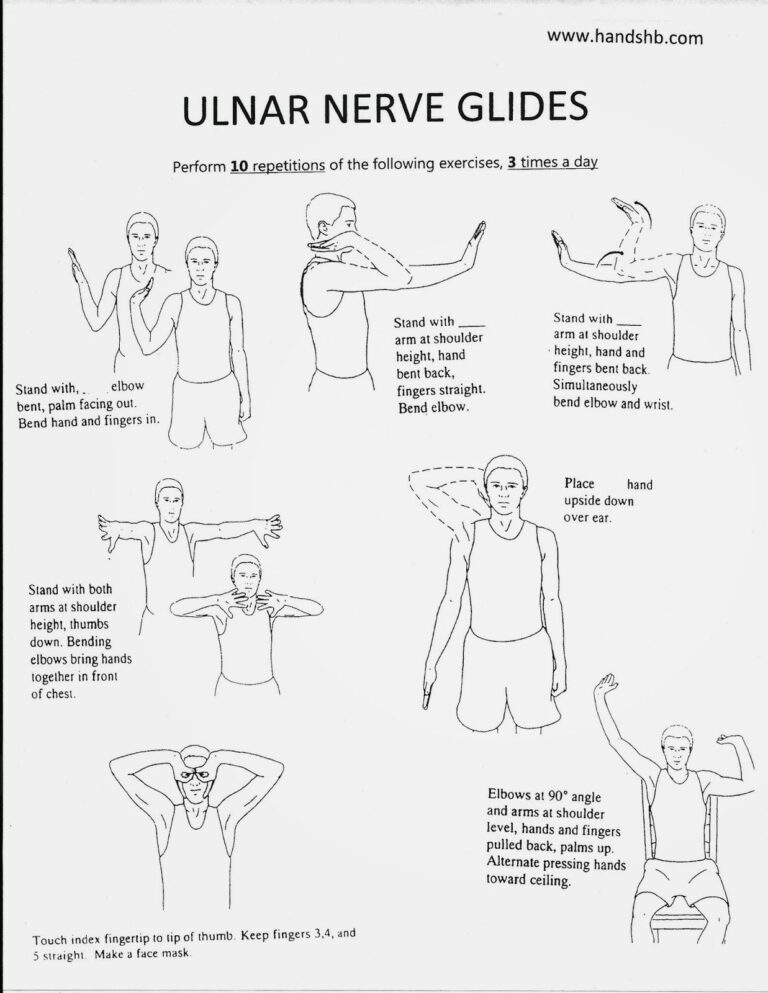
- Inflammation or adhesions anywhere along the ulnar nerve path can cause the nerve to have limited mobility and essentially get stuck in one place.
- These exercises help stretch the ulnar nerve and encourage movement through the cubital tunnel.
Elbow Flexion and Wrist Extension :
- Equipment needed: none
- Nerve targeted: ulnar nerve
- Sit tall and reach the affected arm out to the side, level with your shoulder, with the hand facing the floor.
- Flex your hand and pull your fingers up toward the ceiling.
- Bend your arm and bring your hand toward your shoulders.
- Repeat slowly 5 times.
Head Tilt :
- Equipment needed: none
- Nerve targeted: ulnar nerve
- Sit tall and reach the affected arm out to the side with elbow straight and arm level with your shoulder.
- Turn your hand up toward the ceiling.
- Tilt your head away from your hand until you feel a stretch.
- To increase the stretch, extend your fingers toward the floor.
- Return to starting position and repeat slowly 5 times.
Arm Flexion in Front of Body :
- Equipment needed: none
- Nerve targeted: ulnar nerve
- Sit tall and reach the affected arm straight out in front of you with your elbow straight and arm level with your shoulder.
- Extend your hand away from you, pointing your fingers toward the ground.
- Bend your elbow and bring your wrist toward your face.
- Repeat slowly 5-10 times.
OK SIGN :
- Equipment needed: none
- Nerve targeted: ulnar nerve
- Sit tall and reach the affected arm out to the side, with elbow straight and arm level with your shoulder.
- Turn your hand up toward the ceiling.
- Touch your thumb to your first finger to make the “OK” sign.
- Bend your elbow and bring your hand toward your face, wrapping your fingers around your ear and jaw, placing your thumb and first finger over your eye like a mask.
- Hold for 3 seconds, then return to starting position and repeat 5 times.


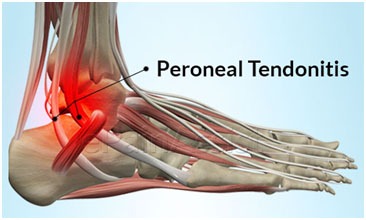

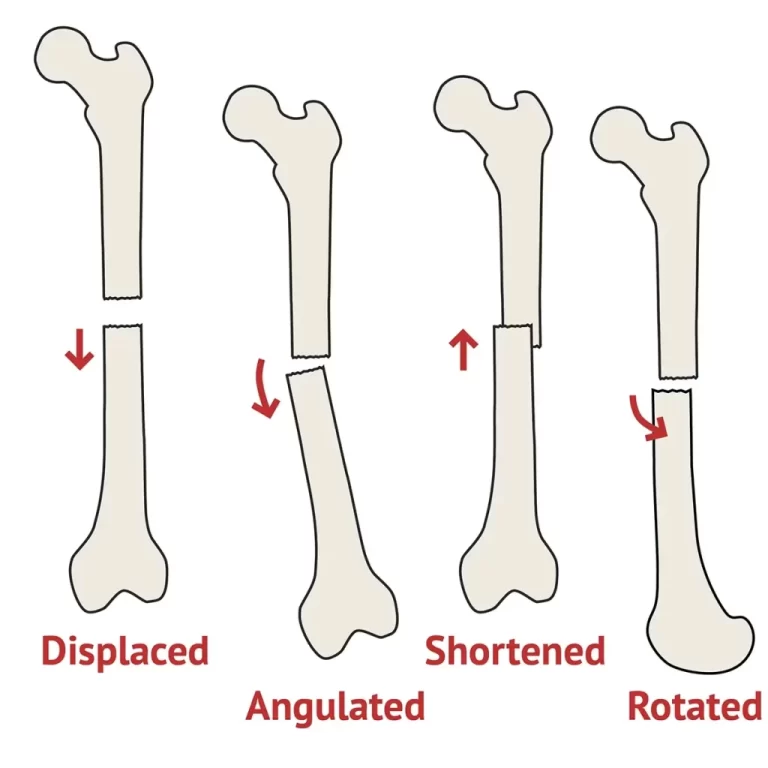
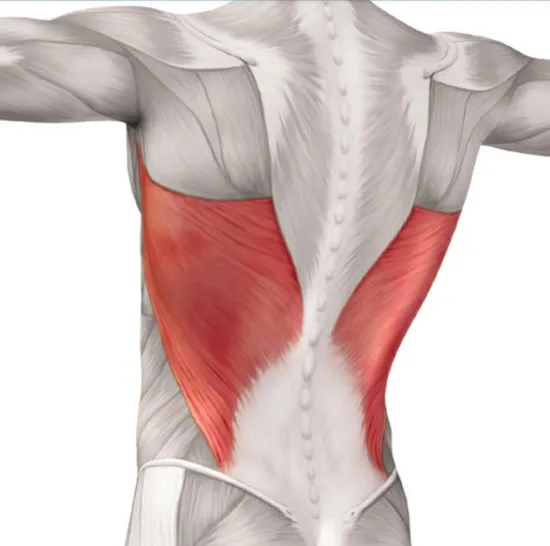


11 Comments