Enthesitis
What is Enthesitis?
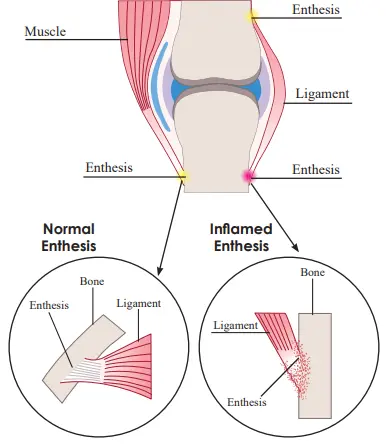
The skeletal system consists of different components, including bones, tendons, and ligaments. Together, these tissues give support to the body and permit motion. An enthesis forms at the point where a tendon or ligament connects to a bone. There are more than a hundred entheses in the human body. Enthesitis happens when an enthesis evolves inflamed and painful.
For instance, Achilles tendinitis is a state of enthesitis. Plantar fasciitis is also a state of enthesitis. Enthesopathy is the medical name for any condition or disease involving an enthesis. Doctors or physicians may use the words enthesopathy and enthesitis interchangeably itis means inflammation of the enthesis.
Synonyms
enthesopathy
polyenthesitis
What are Entheses?
there are two kinds of enthesis: fibrous and fibrocartilaginous fibrous tissue of the tendon or ligament expands up to the bone, but at the latter, there is a small spigot of fibrocartilage at the attachment area itself most entheses of rheumatological importance are fibrocartilaginous existence of this tissue at an enthesis hardens the tendon/ligament and thus allows to create of a more gradual evolution in mechanical effects between soft and hard tissues
particularly an enthesis provides that any bending of the tendon/ligament fibers during joint or junction actions is spread gently out from the bone – thus dispersing tension concentration
When is enthesitis inflammatory and mechanically induced?
mechanically-related tendinopathy or enthesopathy may happen from damage, involving sports-related movement. Imaging examinations may verify the actuality of entheseal pathology but the impressions, whether at the annulus or bone-disc interfaces in the spine or the plantar fascia, may be equal in both mechanical and inflammatory disorder
in the point of the Achilles tendon, degenerative tendon condition generally happens 2-6 cm proximal to the enthesis itself, whereas inflammatory condition is based on the insertion and adjoining bone
both inflammatory and degenerative enthesopathy share general features
entheses are areas of elevated mechanical stressing and with age, normal entheses are subject to wear and tear; thus degenerative differences happen at their fibrocartilages that are equal to those seen in osteoarthritic articular cartilage
Symptoms and locations
Enthesitis is generally associated with stiffness, pain, and tenderness at the insertion area, occasionally without much swelling. Yet, where there is the involvement of the big insertions of lower limbs, swelling can be effective and noticeable. If swelling is absent, enthesitis can be hard to identify or suppose during a physical inspection. it most generally happens in entheses in the following locations:
the backbone
the hips
the knees
the heels
the undersides of the feet
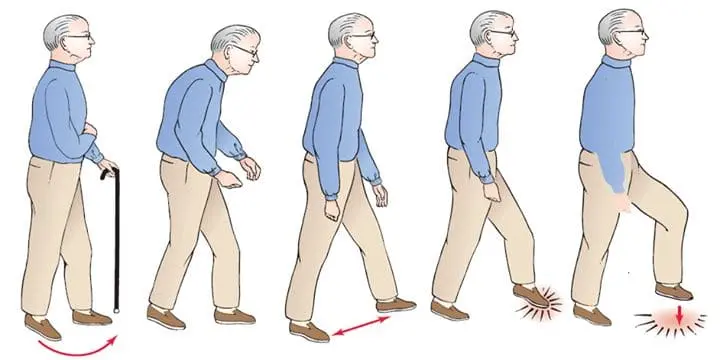
Physical movement may aggravate symptoms of enthesitis. A patient may have problem jogging, running, or ascending stairs because of the pain.
Long-time enthesitis may lead to permanent changes that involve body motion and function. One of these likely differences is ossification, which is the construction of new bone tissue. For eg., a heel spur is an extra bone that extends from the heel.
Another likely difference is fibrosis, a situation in which soft body tissues evolve thickened and scarred, involving motion.
What are the Causes of Enthesitis?
Enthesitis can happen as a consequence of damage, overuse, or underlying condition.
Overuse
Enthesitis can evolve as an effect of prolonged pressure on the joints or junctions. This can be done as a measure of the following:
having overweight or obesity
playing sports
conducting activities that include repetitive motions
Damage
Enthesitis can also form after an injury to the ligaments, tendons, and other connective tissue. Instances of these injuries involve:
Achilles tendinitis: An overuse damage of the Achilles tendon, which attaches to the calf muscle and heel bone.
Rotator cuff syndrome: An damage or degenerative disease involving the rotator cuff, which is a group of muscles and tendons that keep the upper arm bone inside the shoulder socket.
Plantar fasciitis: Inflammation of the plantar fascia.The ligament that attaches the heel bone to the toes.
Bursitis of the hip: Inflammation of the fluid-filled sacs or bursa that protect the hip joints or junctions.
Disease
Enthesitis can occur because of underlying inflammatory disorders and autoimmune diseases, where the immune system strikes tissues within the joints or junctions. Examples involve:
Psoriatic arthritis: A variety of arthritis that may impact patients with the skin disease psoriasis.
Gout: A variety of arthritis in which a buildup of uric acid in the body starts sudden and severe joint or junction pain.
Juvenile idiopathic arthritis: Arthritis that involves kids and teenagers.
Ankylosing spondylitis: An inflammatory disease that causes the vertebrae of the spine to merge.
Doctors or physicians do not understand exactly how many patients with the above conditions will go on to create enthesitis.
Conditions Associated With Enthesitis
Enthesitis may be related to inflammatory diseases or it may be mechanically generated by damage. Peripheral enthesitis is characteristic of all spondyloarthropathies, ankylosing spondylitis, involving undifferentiated spondyloarthritis, enteropathic arthritis, psoriatic arthritis, and reactive arthritis.
Reactive arthritis is a condition of arthritis that results from infection. The swelling of reactive arthritis is frequently activated by an infection in a more distant body region, like the intestines, the urinary tract, or the genitals. Generally, the joints or junctions of the feet, knees, and ankles are marks of inflammation secondary to reactive arthritis. Additionally particularly, enthesitis in a patient with reactive arthritis usually happens in the pelvic bones, the plantar fascia, or the Achilles tendon. Reactive arthritis is unusual and usually goes out in most patients within a year after beginning.
Ankylosing spondylitis is an inflammatory disease that is numerous dominant in males. The inflammation of ankylosing spondylitis involves the vertebrae and causes them to merge. Chronic enthesitis of the tendons and ligaments of the vertebrae is the foremost action in the eventual fusion of vertebrae, which is the main part of ankylosing spondylitis. Someone with ankylosing spondylitis can also feel enthesitis of the costochondral joints or junctions or joints of the ribs.
Other diseases associated with enthesitis involve rheumatoid arthritis, Achilles tendinitis, osteoarthritis, and diffuse idiopathic skeletal hyperostosis (DISH). It may be degenerative enthesopathy that grows with osteoarthritis. The degenerative differences that happen with wear-and-tear osteoarthritis also involve fibrocartilages.
Enthesopathy can happen at the elbow, shoulder, wrist, hip, carpus, knee, tarsus, ankle, or heel bone, among other areas. Enthesopathy may assume the state of spondyloarthropathies (joint or junction conditions of the spine) like plantar fasciitis, ankylosing spondylitis, and Achilles tendinitis. Other examples involve:
- Adhesive capsulitis of the shoulder
- Rotator cuff syndrome of the shoulder and associated diseases
- Periarthritis of shoulder
- Scapulohumeral fibrositis
- Synovitis of the hand or wrist
- Periarthritis of wrist
- Gluteal tendinitis
- Iliac crest spur
- Psoas tendinitis
- Trochanteric tendinitis
Differential Diagnosis
The differential diagnosis of enthesopathy can involve:
- avulsions fractures
- ligament or tendon rupture
- localized infection
- contusions
- muscle strains
- malignancy
How to Diagnose Enthesitis?
To diagnose enthesitis, a doctor or physician will ask about a patient’s symptoms and medical record, involving whether the patient has a family record of the disease. They will also study the involved locations for signs of swelling and tenderness.
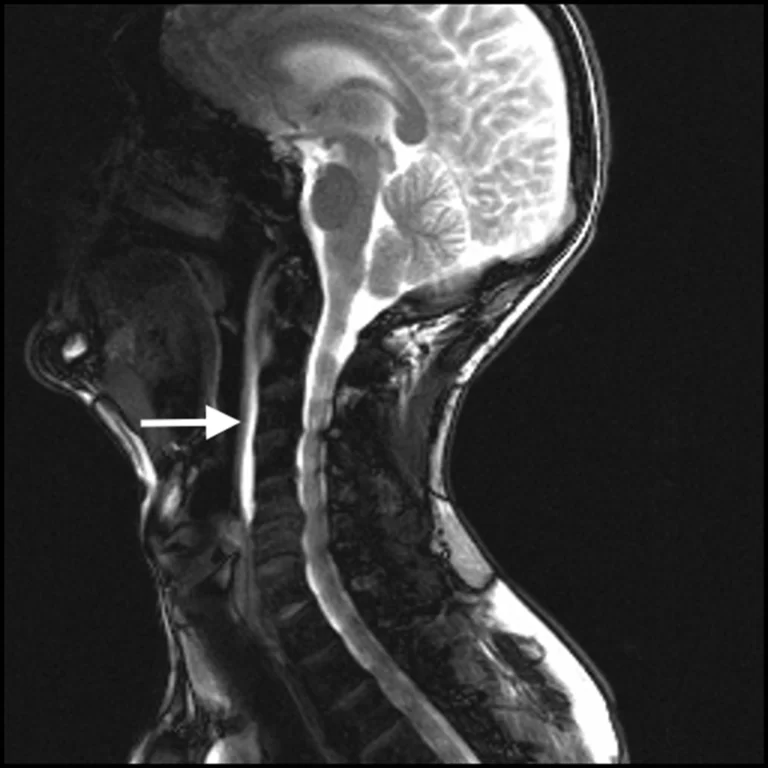
In a few patients, a doctor or physician may suggest medical examinations to rule out further diseases like rheumatoid arthritis. Tests may involve:
blood tests
ultrasound scans
MRI scans
Depending on the measures of the medical examinations, the doctor or physician may recommend the patient to a rheumatologist for a more in-depth analysis.
Treatment of Enthesitis
Medical Treatment
The treatment for enthesitis depends on different aspects, involving:
the cause of the disease
the symptoms a patient incidents
how long has the patient felt symptoms
One likely treatment choice is nonsteroidal anti-inflammatory drugs (NSAIDs). Medications like ibuprofen and piroxicam can assist in the relief of inflammation and pain.
Another therapy choice is steroids. Medications that can assist in relieving inflammation and relieve joint or junction pain and stiffness. If enthesitis involves a typical joint or junction, a doctor or physician may suggest a corticosteroid injection into the joint or junction to reduce symptoms.
A rheumatologist doctor may recommend biological medicines to treat enthesitis resulting from autoimmune arthritis. Biological medicines derive from living references, like bacteria and plants. These medications can assist sluggish or control inflammation by targeting exact steps in the inflammatory procedure.
Another treatment choice is disease-modifying antirheumatic medicines (DMARDs). These medications assist to delay the progression of autoimmune arthritis by targeting parts of the immune system itself.
A patient may also satisfy by the following:
resting the involved junctions or joints
avoiding movements that aggravate symptoms
practicing physiotherapy to assist restore usual joint or junction role and mobility
Enthesitis can be caused by psoriatic arthritis, gout, reactive arthritis, diffuse idiopathic skeletal hyperostosis (DISH), ankylosing spondylitis (spondyloarthropathy), and rheumatoid arthritis.
Physiotherapy Treatment
Physical therapy can decrease pain and stiffness in the joints or junctions and nearby places. Most physical therapy concentrates on boosting and relaxing tight muscles, along with enhancing flexibility near the enthesis. For example, someone with Achilles tendon enthesopathy may help from calf muscle stretches conducted 2-3 times per day.
Accomplishing these activities on both sides, and not only the side involved by enthesopathy can control muscle inequalities, troubles with posture, and aggravate pain.
Physical therapy can assist patients with enthesopathy to work around their damage without making the ache more harmful.
The purposes of physiotherapy and activities for the disease are the following :
Boost the muscle of the spine and muscles of the lower back, buttocks, abdomen, and hip.
Boost core muscles’ power
Stretch stiff and tense muscles, like the calf muscle
Promote the interaction of fluids and nutrients in the body via light aerobic activities like swimming, walking, or pool therapy.
Knee-to-chest stretch
The knee-to-chest stretch can assist to extend your lower back, reducing stress and pain.
Lie on your back in a supine position with your knees flexed and your feet flat on the ground.
Operating both hands, grasp or grip your right lower leg and twist your fingers, or hold your wrists slightly under the knee joint.
While maintaining your left foot flat on the bottom, slowly drag your right knee joint to your chest until you sense a little stretch in your lower back.
Keep your right knee joint against your chest for 3060 seconds, making it foolproof to rest your hips, legs, and lower back.
Withdraw your right knee joint and return to the beginning position.
Reproduction of step 24 with your opposite leg.
Replay 3 times per leg.
To complete this stretch more complex, simultaneously obtain your knee joints to your chest for 1520 seconds. Accomplish this 3 times, with per repetition divided by 30 seconds of downtime.

Trunk rotation
The trunk rotation can assist to ease pressure in your lower back. It also performs your core muscles, involving your back muscles, abdominals, and the muscles near your pelvis.
Lie on your back in a supine position and obtain your knee joints up toward your chest, so your body is placed as if you’re sitting in a chair.
Fully lengthen your arms out to the sides, with your palms lying on the bottom. Maintaining your knee joints jointly and hands on the bottom, gently move both flexed knee joints over to your right side and maintain for 1520 seconds.
Return to the beginning position and replicate step 3 on your opposite side, also maintaining for 1520 seconds.
Recount 510 times per side.

Cat-Cow
The Cat-Cow assists to improve flexibility and relieve stress in your lower back muscles and core muscles.
Bring onto your hands and knee joints with your knee joints hip-width separated. This is your beginning position.
Flex your back by dragging your belly button up toward your spine, allowing your head to fall forward. This is the first part of the stretch.
Keep for 510 seconds. You should sense a mild stretch in your lower back.
Return to the beginning position.
Lift your head and allow your pelvis to drop forward, bending your back down toward the bottom. This is the second part of the stretch.
Keep for 510 seconds, then return to the beginning position.
Replicate the Cat-Cow stretch 1520 times.
You can also complete this activity in a chair with your feet flat on the bottom and your hands on your knee joints. This transformation is an excellent method to sneak in a rare stretch at a job.

Seated hamstring stretch
Tense hamstrings are supposed to be a familiar supporter to lower back pain and damage. This exercise stretches the hamstring muscles to reduce tightness and remove stress in your spine.
Sit on the bottom in a sitting position with one leg straight out in front of you.
Connect a standard bath towel near the base of your foot at the heel.
Gently flex ahead at your hips, getting your belly down to your thighs.
Maintaining your back straight, hold the towel to assist you to obtain your belly nearer to your legs.
Stretch until you sense mild pressure in your lower back and the back of your leg.
Maintain for 10 seconds, relax for 30 seconds, and reprise 3 times.
You can improve or reduce the stress of this stretch by holding the towel nearer to or distance out from your feet.
As you evolve more flexibly over the period, you can improve how long you maintain the stretch or decrease the time between repetitions.

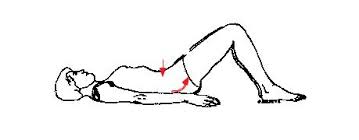
Pelvic tilt
The pelvic tilt is a straightforward yet useful way to free tense back muscles and keep their flexibility.
Lie on your back in a supine position with your knee joints flexed and feet flat. Your hands can be around the bottom of your head (as if you’re around to complete a situp), or you can keep your arms by your flanks. The unassuming curvature of your spine will raise your lower back barely off the bottom.
Gently flex your lower back and force your stomach out, stabilizing your core muscle.
Keep for 510 seconds, then rest.
Move your pelvis up barely toward the roof while tensing your abdominal muscles and buttock muscles. In accomplishing so, you should sense your lower back pushing into the bottom. (Your pelvis should not escape the bottom.)
Keep for 510 seconds, then rest.
Begin with 1015 repetitions every day, producing up to 2530 repetitions.
Flexion rotation
The flexion rotation allows stretching of your lower back muscles and buttocks muscles.
Lie on your right side in a side-lying position with both legs straight.
Flex your left leg, attaching your foot after your right knee joint.
Grab your left knee joint with your right arm.
Put your left hand after your neck.
Gradually turn your upper body backward by touching your left shoulder edge to the bottom. You should sense a gentle stretch in your lower back.
Reprise the cycle 10 times, maintaining per stretch for 13 seconds before gradually moving out of the process.
Replication steps 16 on your opposite side.

Supported bridge
You’ll use a foam roller or firm pillow to complete the supported bridge. This activity allows relaxing your lower back via supported elevation.
Lie on your back in a supine position with your knee joint flexed and feet flat on the bottom.
Raise your hips and put a foam roller or firm pillow under them.
Thoroughly calm your body with the help of the bottom and the foam roller or firm pillow.
Keep for 3060 seconds and replicate 35 times, relaxing for 3060 seconds between sets.

Belly flop
Like the supported bridge, the belly flop to relaxes your lower back via supported elevation. At this moment, you’ll utilize a rolled towel or blanket.
Proceed up a towel or blanket lengthwise, and put it horizontally in front of you.
Lie front-side down in a prone position over the towel or blanket so that your hip bones are pushing into it.
Calm your body. You can turn your head to one side.
Remain in this position for 12 minutes and reprise 13 times, relaxing for 3060 seconds between sets.
External hip rotation
Sit on the bottom in a sitting position with both legs out in front.
Flex the legs at the knee joints and push the soles of the feet jointly.
Put a hand on top of each knee joint and gently press them both down toward the bottom. Apply force to the knee joints until there is a stretch, but accomplish not push them distant than is satisfied.
Maintain the stretch for 10 seconds and then rest.
Reprise the stretch 510 times.
Double hip rotation
Lie flat on the back or achieve a supine position. Then, flex the knee joints and obtain them toward the body until the feet are flat on the bottom.
Slightly turn the knee joints to the left, dropping them toward the bottom. Turn the head to face the right while maintaining the shoulders against the bottom.
Keep this position for 2030 seconds.
Gradually return both the head and knee joints to the beginning position.
Reprise on the further side.
Hip and lower back stretch
Lying flat on the back in a supine position, flex the knee joints and obtain them toward the body until the feet are flat on the bottom.
Using the hands, drag both knee joints toward the chest.
Breathe deeply, dragging the knee joints closer to the shoulders with per exhalation.
Go as distant as is satisfied, then maintain the position for 2030 seconds. Breathe naturally.

Hip flexion
Stand erect.
Raise one arm out to the side and maintain on to a sturdy cover, like a table, a wall, or a chair, for help.
Gradually lift the right knee joint to the level of the hip or as distant as is satisfied while maintaining the left leg straight.
Only maintain this position for a second before putting the left foot back on the bottom.
Reprise with the further knee joint.
Accomplish 510 repetitions of this movement.
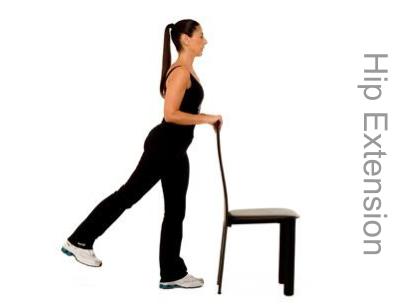
Hip extension
Stand erect with the legs straight and the feet shoulder-width separated.
Lengthen both arms out in front and keep on to a table, a chair, or a wall for help.
Maintaining the right leg straight, raise the left leg backward without flexing the knee joint.
Raise the leg as distant as possible without causing distress, then hold the buttock tightly and maintain the position for 5 seconds.
Reprise this stretch 510 times per leg. To raise the opposition, try connecting small weights to the legs.
Hip abduction
Stand erect.
Expand the left arm out to the side and maintain on to something stable, like a table, chair, or wall.
Beginning with the feet jointly, raise the right leg to escape to the right side. Hold the left leg straightforwardly and avoid turning the hips.
Keep the position for 5 seconds and then gradually return the leg to the beginning position.
Accomplish this activity 510 times on one leg, then reprise it on the further side.

Heel-to-buttock exercise
Stand erect with the legs straight and the feet shoulder-width separated. For help, maintain on to a table, chair, or wall.
Flexing the left knee joint, obtain the heel up toward the left buttock with the top of the foot meeting the bottom. Be sure to maintain the right leg straightforwardly and align the knee joints.
Gradually lower the leg and return to the beginning position.
Reprise the activity on the further side.
Goal to do 510 repetitions per leg.

Mini squat
Stand erect with the feet shoulder-width separated.
If required, keep on to a table, chair, or wall for help.
Maintaining the back straight, gently reduce the body by flexing the knees joint until they are above the toes. The feet should stay flat on the bottom.
Maintain this position for a few seconds, then gradually straighten the legs to return to the beginning position.
Reprise these mini squats 510 times.

Short-arc quadriceps exercise
Lie flat on the back in a supine position with a cushion or rolled-up towel under the right knee joint.
Glide the left foot back toward the buttock, flexing the knee joint.
Gradually raise the right foot off the bottom while maintaining the back of the right knee joint pushed against the cushion or towel.
Maintain the position for 5 seconds and then slightly lower the right leg back to the beginning position.
Accomplish 510 thrills on one leg and then change to the further leg.

Quadriceps exercise
Lie flat on the back in a supine position and maintain the legs straighten throughout the movement.
Press the backs of both knee joints toward the bottom and bend both feet by dragging the toes toward the body.
Maintain the position for 5 seconds, then rest.
Accomplish 510 repetitions.
Chair stand
Position a chair so that its back is relaxing opposite to a wall.
Sitting on the front portion of the seat in a sitting position, flex the knee joints and put the feet flat on the bottom. Cross the arms, putting per hand on the opposite shoulder.
Swinging at the hips, slump back into the chair.
Bend the upper body forward similarly and then gradually stand up. Hold the shoulders, back, and head straight while doing this.
Gradually sit back down and return to the starting position.
Replicate this movement 46 times, to start with before slowly making up to 12 repetitions.
Quadriceps stretch
This stretch particularly targets your quadriceps muscles, the muscles situated at the front of your thighs. Completing this movement can assist to enhance the flexibility in your hip flexors muscles and quadricep muscles.
Stand next to a wall in a standing position or use a chair for assistance. Your feet should be shoulder-width separated.
Flex one knee joint so your foot moves up toward your glutes.
Grasp your ankle and slightly drag it toward your glutes as far as you can comfortably.
Maintain for 30 seconds.
Return to the beginning position and switch the legs.
Reprise 2 times on per side.
Leg extensions
Using your body weight, instead of a weighted device, to boost your quadriceps assists to support added stress off your knee joints.
Sit up straight in a chair in a sitting position.
Place your feet flat on the bottom, hip-width separated.
Look straight forward, tighten your thigh muscles, and lengthen one leg as tall as possible without lifting your buttocks off the chair.
Break, then lower to the beginning position.
Accomplish 2 to 3 sets of 10 repetitions per leg.
Straight leg raises
The straight leg raise boosts your quadriceps muscles as well as your hip flexor muscles. If you bend your foot at the end of the activity, you should also sense your shins tense.
As this movement gets more comfortable to do, you can add a 5-pound ankle poundage and slowly work up to a weightier weight as you create strength in your legs.
For this activity, you can use a mat to add softening under your back.
Lie down on the bottom in a supine position with one leg flexed and one leg directly out in front of you.
Tighten the quadricep of your straight leg and gradually lift it off the bottom until it’s the exact height of your flex knee joints.
Stay at the top for 5 seconds, then lower to the beginning position
Accomplish 2 to 3 sets of 10 repetitions per leg.
Side leg raises
This activity functions your hip abductor muscles as well as your glutes. Your hip abductor muscles, situated on the exterior of your hips, assist you to stand, walk and turn your legs with comfort. Boosting these muscles can assist control and managing pain in the hips and knee joints.
As this movement gets more comfortable to do, you can add a 5-pound ankle poundage and slowly work up to a weightier weight as you make strength in your leg muscles.

Plantar Fascia Massage
Note: You should not experience pain during this movement. Use enough force to sense a soft stretch, but not ache.
Sit in a chair in a sitting position or stand with one foot relaxing on a small ball or rigid water bottle. A rigid water bottle is helpful as the ice benefits decrease inflammation.
Slightly move the ball or water bottle ahead and back under your foot. Begin slightly below the ball of your foot and stop slightly before your heel.
Move the ball or bottle back and forth gradually 10 times per foot. Accomplish two sets on each foot.
Accomplish this movement once every day.
Heel Raise
Note: This activity should be done gradually and with controlled activities. Make sure to keep your equilibrium and maintain on to a bar or other help if required.
Stand or achieve a standing position with the balls of your feet at the border of the lowest step.
With your heels swinging off the border, gradually and slightly lower your heels slightly below the border of the step. You may sense a stretch in your calf muscle.
Gradually wake onto the balls of your feet.
Reprise this 10 times, then relax. Finished two sets of this activity.
Accomplish this activity once every day.

Floor Sitting Ankle Inversion With Resistance
Note: This activity needs an elastic exercise band.
Sit upright on the bottom with your legs straight out in front of you. Make confident to avoid any hip motion while doing this movement.
Put your left leg over your right leg with an opposition band attached near your upper foot and twisted near the base of your lower foot. Put the end of the band in your hand.
Gradually move your upper foot (the one with the opposition band near it) out from the lower foot. To accomplish this, turn your ankle inward and gradually return it to the beginning position.
Reprise 10 times and finished two sets in each foot.
Accomplish this activity once every day.

Seated Toe Towel Scrunches
Note: Make confident that your entire foot remains on the bottom and that only your toes do the work of this movement.
Sit erect in a chair in a sitting position with one foot relaxing on a towel and fanning your toes.
Bend your toes to crumple and pull the towel toward you 10 times. Accomplish two sets on each foot.
Accomplish this movement once every day.

Seated Plantar Fascia Stretch
Note: Finish this stretch in a gradual and regulated way.
Sit in a chair in a sitting position and cross one leg over the other knee joint, so your ankle is on top of your further leg.
With one hand keeping your ankle joint and the further keeping your toes, slightly drag your toes backward until you sense a stretch in the base of your foot.
Maintain this position for 20 seconds and reprise it three times for both feet.
Accomplish this movement once every day.

Wall-Facing Calf Stretch
Stand erect facing a wall at arm’s length and put your hands flat on the wall.
Maintaining both feet flat on the bottom, expand one leg straight backward, flexing your front leg until you sense a stretch in the calf of your back leg.
Maintain for 20 seconds and reprise three times for both legs.
Accomplish this activity once every day.

Toe raise, point, and curl
This activity has three phases and will assist boost all elements of the feet and toes.
Sit up straight in a chair in a sitting position, with your feet flat on the bottom.
Maintaining the toes on the bottom, lift the heels. Control when only the balls of the feet stay on the ground.
Maintain this position for 5 seconds before dropping the heels.
For the second step, lift the heels and indicate the toes so that only the ends of the big and second toes are touching the bottom.
Maintain for 5 seconds before dropping.
For the third step, lift the heels and bend the toes inward so that solely the ends of the toes are feeling the bottom. Maintain this position for 5 seconds.
Make flexibility and mobility by replicating per step 10 times.
Heat and ice treatment
Heat/ice therapy is very easy and easy to execute therapy. The therapy is generally applied to back ache which is caused by damage.
Cover ice in a towel or dense cloth and set it on the involved area. There are several heating pads available in the demand for this goal. The cause of aches overlooks the variety of therapy.
Use ice and then heat if the ache is acute, if chronic gentle heat should be used, and for soreness after the movement uses ice.

Massage therapy
Specialists are now seeing Massage as support for lower back aches. Massage therapy is generally suggested in the case of tight muscles. The best component of massage therapy is that you can feel the outcome even after the first session.
Orthotics
Orthotic instruments, like heel cup shoe inserts, can ease the pain of some varieties of enthesopathy. They may also control additional damage. A splint can assist to support the joint or junction and stretch surrounding muscles, especially at night.
Surgery
Surgery is generally noticed as a last resort. When it’s required, it’s frequently due to enthesopathy caused by an underlying disease.
Your doctor or physician may suggest a total joint or junction replacement. In this process, your doctor or physician surgically extracts your involved bone and places it in a plastic or metal prosthesis.
Is it possible to prevent enthesitis?
Enthesitis that is caused by damage can be controlled by steps that avoid damage. Occasionally help braces can be useful with specific athletic exercises.
Home Remedies for Enthesitis
A physical therapist can provide you with soft stretches to do at home to assist to reduce the ache of enthesitis. In addition, the doctors or physicians and patients we talked to offer:
- Use heat or ice at involved sites
- Keep a healthy weight. Weight loss can bring stress off the occupied areas.
- Rest and elevate the involved foot.
- Wear special shoes. Someone with plantar fasciitis can satisfy shoe inserts to soften the heel and may be supported.
- Wear compression braces, socks, wraps, or even a medical boot.
- Watch salt intake to control swelling. Salt input does create a dissimilarity.
- Over-the-counter remedies (check with your doctor or physician first).
Lifestyle changes
Your doctor or physician may suggest creating lifestyle modifications if overuse or extreme exercise has caused your enthesopathy or an underlying disease.
If you use the involved joint or junction area frequently for work or leisure actions, your doctor or physician may recommend that you decrease the quantity of work or action that may be making the pain or inflammation more harmful.
If you exercise daily and the activity is placing stress on your joints or junctions, your doctor or physician may assist you to develop a new movement plan that permits you to resume exercising daily while placing less stress on the involved joint or junction area.
Other therapies that can help contain:
- cold or hot packs, or rotating the two, to decrease inflammation
- massaging the involved joint or junction, or surrounding muscles
- cold laser therapy, a light therapy that may decrease inflammation and pain
- alternative therapies, like acupuncture
- corticosteroid injections for inflammatory enthesitis
- If a motion is painful, then a patient would be suggested to avoid it, as much as they can.
Prognosis
The prognosis of enthesopathy is typically profitable and provides the underlying etiology. With sufficient rest and rehabilitation, most patients of enthesopathy will settle over 2-4 weeks.
Enthesopathy from the diffuse inflammatory condition may result in extended healing times and is comparable to the severity and etiology of the underlying disorder.
FAQ
Does enthesitis improve with exercise?
Suggested model of exchange of mechanical strain elements, genetics, and environmental aspects in the pathogenesis of enthesitis in SpA. The therapy method with physical activity and exercise has been shown to enhance symptoms and signs of axSpA and to enhance function and quality of life
Will enthesopathy go away?
Many varieties of enthesopathy, like tendonitis and fasciitis, may ultimately go out, but others can be lifelong diseases. Therapy and physical therapy for enthesopathy can assist to relieve pain, improve flexibility and range of movement, and reduce the consequences of the disease.
Where is the enthesis located?
An enthesis is the area of attachment of the ligament, tendon, fascia, or capsule to the bone. There are two kinds of entheses: fibrous and fibrocartilaginous. Fibrous entheses are located at the extension of the tendon to the metaphysis or diaphysis and are comprised of thick fibrous tissue.
Can you have enthesitis without psoriatic arthritis?
Patients with PsA are more probable to create enthesitis, and it is more possible to be chronic in this class. Someone who is not living with PsA can feel enthesitis also. According to the Arthritis Foundation, tennis elbow can obtain inflammation and is one of the numerous familiar causes after PsA.
How long does enthesitis last?
Enthesitis also occurs in about 10% to 20% of kids with juvenile idiopathic arthritis, which can involve one or more joints or junctions and stays at least 6 weeks.