Facioscapulohumeral muscular dystrophy (FSHD)
What is Facioscapulohumeral muscular dystrophy (FSHD)?
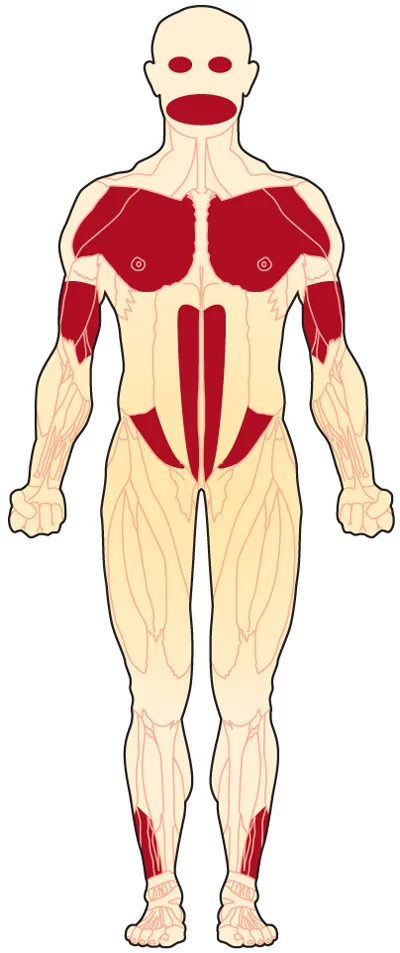
Facioscapulohumeral muscular dystrophy (FSHD) is a genetic muscle disorder in which the muscles of the face, shoulder blades, and upper arms are among the most affected. that initially affects the skeletal muscles of the face (facial), scapula, and upper arms (humeral). FSHD is the third most common genetic disease of skeletal muscle.
Symptoms of Facioscapulohumeral muscular dystrophy:
→ Facial muscle weakness (eyelid drooping, inability to whistle, decreased facial expression, depressed or angry facial expression, difficulty pronouncing the letters M, B, and P)
→ Shoulder weakness (difficulty working with the arms raised, sloping shoulder)

→ Hearing loss
→ Abnormal heart rhythm
→ Unequal weakening of the biceps, triceps, deltoids, and lower arm muscles
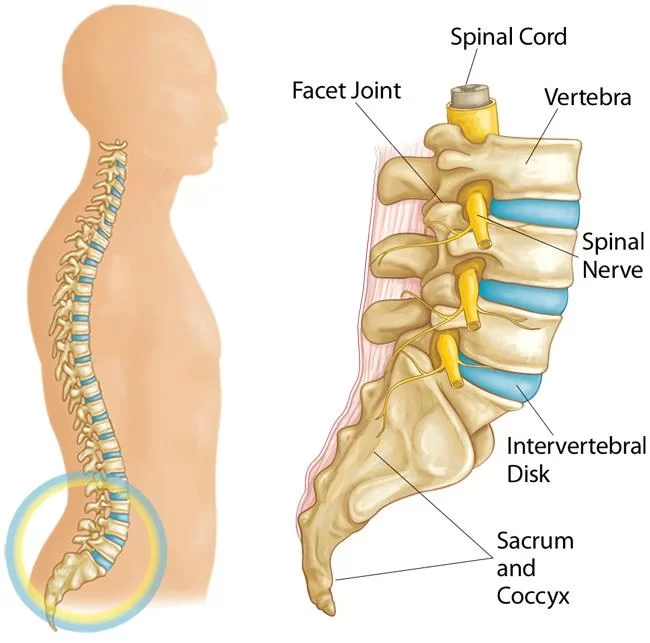
→ Loss of strength in abdominal muscles (causing a protuberant abdomen and lumbar lordosis) and eventual progression to the legs
→ Foot drop
→ Abnormalities of the retina
→ Unequal (nonsymmetrical) weakness

Causes of Facioscapulohumeral muscular dystrophy:
→ FSHD may be inherited through either the father or the mother, or it may occur without a family history. It is almost always associated with a genetic flaw (mutation) that leads to a shorter than usual segment of DNA on chromosome 4. The segment isn’t part of any particular gene, but it nevertheless seems to interfere with the correct processing of genetic material.
Diagnosis:
→ Creatine kinase (CK) level: This test measures the Creatine kinase enzyme in the blood. Elevated levels of CK are related to muscle atrophy.
→ Electromyogram (EMG): This test measures the electrical activity in the muscle
nerve conduction velocity (NCV): This test measures the how fast signals travel from one part of a nerve to another. The nerve signals are measured with surface electrodes (similar to those used for an electrocardiogram), and the test is only slightly uncomfortable.
→ Muscle biopsy: Through outpatient surgery a small piece of muscle is removed (usually from the arm or leg) and evaluated with a variety of biochemical tests. Researchers are attempting to match results of muscle biopsies with DNA tests to better understand how variations in the genome present themselves in tissue anomalies.
Treatment of Facioscapulohumeral muscular dystrophy:
→ Custom-made ankle-foot orthosis (AFO) may help patients with prominent foot drop. Sometimes AFO may worsen the gait in the presence of knee extensor weakness and these patients may benefit from floor reaction AFO (FRAFO) or newer knee-ankle-foot-orthosis (KAFO).
→ Corticosteroids failed to improve muscle strength or muscle mass.
→ A pilot trial of sustained-release albuterol taken PO (16 mg/d) for 3 months increased lean body mass. A modest 12% increase in muscle strength was noted.
Physiotherapy treatment in Facioscapulohumeral muscular dystrophy:
• GOAL
→ Maintaining highest possible health.
→ Improving or maximizing of the person’s functional abilities.
→ Preventing or delaying complications that may arise from the progression of the condition.
→ Improving or maintaining quality of life.
→ Patient and family education regarding FSHD.
• PLAN
→ Ice/heat application
→ Electrotherapeutic modalities (e.g. TENS)
→ Range of motion (ROM) exercises
→ Strengthening exercises
→ Hydrotherapy (Water) Therapy
→ Recommend
Orthotics/braces if needed
Assistive devices
Adaptive devices
→ Gait training
→ Home or workplace modification
→ Patient Education
What is the progression of FSHD?
This disease progresses mostly gradually and rarely affects the heart or lungs. Most people with FSHD have a near-normal life span. However, disease severity may be variable.
What is the status of the latest research in FSHD?
In 2009, MDA-funded researchers discovered that DUX4 gene fragments in FSHD-affected cells are abnormally activated, resulting in the production of potentially harmful proteins. A likely pathway for the eventual treatment of FSHD appears to be blocking the incorrectly activated genes or the proteins produced from them.
Prognosis
Prognosis can be predicted in part by genetics. Large D4Z4 repeat deletions increase the risk of severe and early disease, as well as non-muscular symptoms (remaining D4Z4 repeat array size: 10-20 kbp, or 1-4 repeats). Severe disease is more likely in people who carry both the FSHD1 and FSHD2 genetic mutations.
Additionally, it has been found that, in contrast to a new mutation, disease manifestation is milder when a strong family history is present. In some large families, 30% of those with the mutation are symptomless, and 30% of those who do exhibit symptoms do not progress past weakness in the shoulders and the face. Women exhibit symptoms less frequently and, when they do, do so with milder manifestations.
Unknown environmental factors are blamed for any remaining variations in disease progression. One study discovered that alcohol and tobacco use—common risk factors for other diseases—do not worsen the disease’s course.



2 Comments