Guillain-Barre syndrome (GBS)
What is Guillain-Barre syndrome (GBS)?
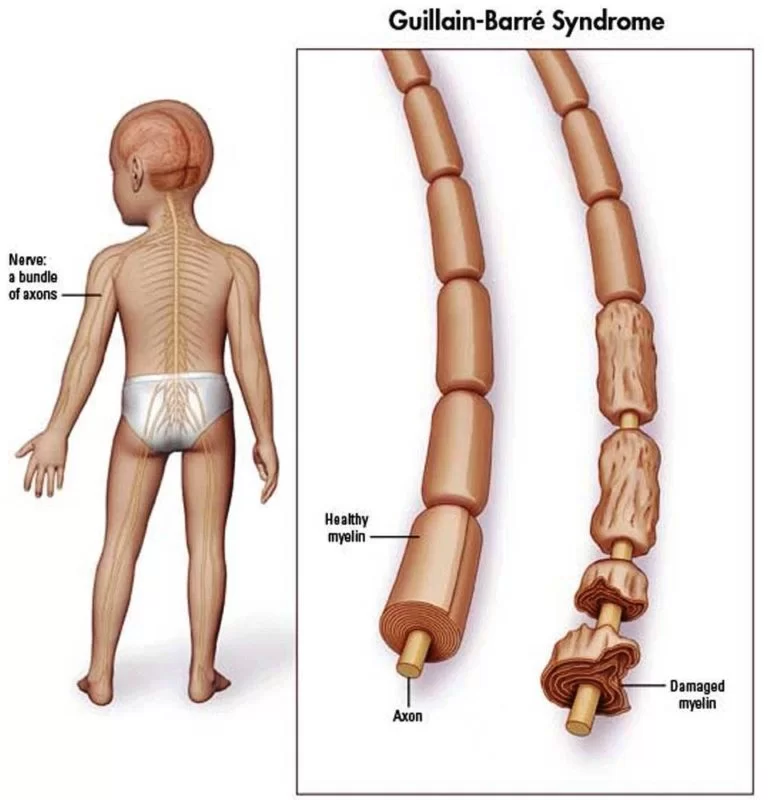
Guillain-Barré syndrome is a rare but serious autoimmune disorder in which the immune system attacks healthy nerve cells in your peripheral nervous system. This leads to weakness, numbness, and tingling. It can eventually cause paralysis. The cause of this condition is unknown, but it’s typically triggered by an infectious illness, such as the stomach flu or a lung infection.
Causes of (Guillain-Barre syndrome)GBS
→ About two-thirds of people with Guillain-Barré develop it soon after they’ve been sick with diarrhea or a respiratory infection.
→ Campylobacter jejuni infection has been associated with Guillain-Barré. Campylobacter is one of the most common bacterial causes of diarrhea. It’s also the most common risk factor for Guillain-Barré. Campylobacter is often found in undercooked food, especially poultry.
→ Idiopathic. No Known Cause For GBS.
The following infections have also been associated with Guillain-Barré:
→ Influenza.
→ Cytomegalovirus, which is a strain of the herpes virus.
→ Epstein-Barr virus infection, or mononucleosis.
→ Mycoplasma pneumonia, which is an atypical pneumonia caused by bacteria-like organisms.
→ HIV or AIDS.
→ Zika Virus
→Hepatitis A, B, C, and E
→ Surgery
→ Hodgkin’s lymphoma
Types of GBS:
Mainly Known as a single disorder, Guillain-Barre syndrome is now known to occur in various forms.
The main types are:
(1) Acute inflammatory demyelinating polyradiculoneuropathy (AIDP) :
The most common form in the U.S. The most common sign of AIDP is muscle weakness that starts From the lower limb of your body spreads to the Upper Limb And Gradually Involves the Lungs And Neck.
(2) Miller Fisher syndrome (MFS): in which Paralysis Starts From Eye Movement associated with an unsteady gait. MFS occurs in about 5 percent of people with Guillain-Barre syndrome in the U.S. but is more common in Asia.
(3) Acute motor axonal neuropathy (AMAN) and acute motor-sensory axonal neuropathy (AMSAN) :
This type is Rarely seen in the U.S. But AMAN and AMSAN are more frequently seen in China, Japan, and Mexico.
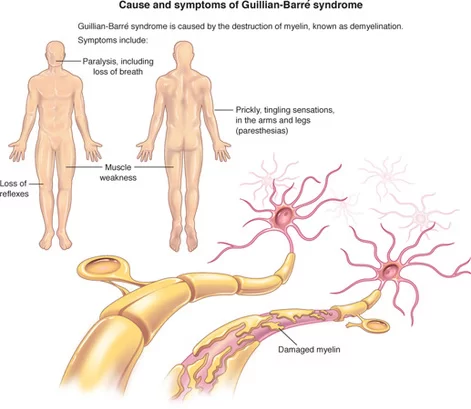
Symptoms of Guillain Baree Syndrome:
→ Tingling or prickly sensations in your fingers and toes.
→ Muscle weakness in your legs that travels to your upper body and gets worse over time.
→ Difficulty walking steadily.
→ Difficulty moving your eyes or face, talking, chewing, or swallowing.
→ Severe lower back pain.
→ Loss of bladder/Bowl control.
→Fast heart rate.
→ Difficulty breathing.
→ Paralysis.
Diagnosis of Guillain Baree Syndrome:
Physical Examination
In addition to examining your physical symptoms, your doctor will review your medical history and do tests to evaluate the health of your muscles and nerves. Your doctor or a specialist will record the timing of the onset of symptoms (with other conditions, muscular weakness may worsen over months rather than days or weeks) and if they affect both sides of the body, as is usual with Guillain-Barré syndrome. Your reflexes will also be examined since deep tendon reflexes in the legs—like knee jerks—are typically impaired in GBS patients. It’s also possible that the arms lack reflexes.
→ Spinal tap
A spinal tap involves taking a small amount of fluid from your spine in your lower back. This fluid is called cerebrospinal fluid. Your cerebrospinal fluid is then tested to detect protein levels. People with Guillain-Barré typically have higher-than-normal levels of protein in their cerebrospinal fluid. This test is also referred to as a lumbar puncture.
→ Electromyography
An electromyography is a nerve function test. It reads electrical activity from the muscles to help your doctor learn if your muscle weakness is caused by nerve damage or muscle damage.
→ Nerve conduction tests
Nerve conduction studies may be used to test how well your nerves and muscles respond to small electrical pulses.
Medical Treatment in Guillain Baree Syndrome:
→ There’s no cure for Guillain-Barre syndrome. But two types of treatments can speed recovery and reduce the severity of the illness:
→ Plasma exchange (plasmapheresis). The liquid portion of part of your blood (plasma) is removed and separated from your blood cells. The blood cells are then put back into your body, which manufactures more plasma to make up for what was removed. Plasmapheresis may work by ridding plasma of certain antibodies that contribute to the immune system’s attack on the peripheral nerves.
→ Immunoglobulin therapy. Immunoglobulin containing healthy antibodies from blood donors is given through a vein (intravenously). High doses of immunoglobulin can block the damaging antibodies that may contribute to Guillain-Barre syndrome.
→ These treatments are equally effective. Mixing them or administering one after the other is no more effective than using either method alone.
You also are likely to be given medication to:
Relieve pain, which can be severe
Prevent blood clots, which can develop while you’re immobile
People with Guillain-Barre syndrome need physical help and physiotherapy before and during recovery.
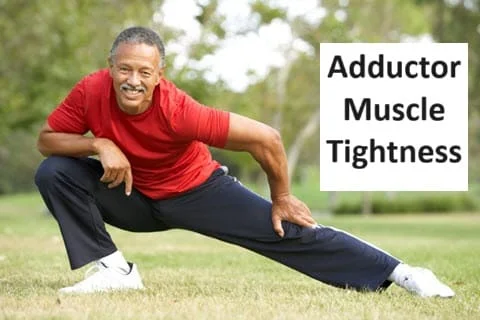
PHYSIOTHERAPY EXERCISE:
The role of physiotherapy for GBS disease can be divided into three parts –
(1) Acute phase
(2) The middle phase of rehabilitation
(3) Long-term, ongoing rehabilitation
The important factor is communication with this multi-disciplinary approach with the aim of the team to help the flow of the treatment of the patient.

(1) The Acute Phase
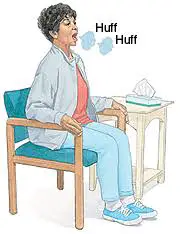
→ In the acute phase a large part of physiotherapy Treatment is for respiratory care. If it affects the intercostal muscle – the one between the ribs that lift up the ribs as we take a breath. Equally, if the diaphragm is affected – the part of the body between the abdomen and the chest – the patient has the inability to take a large breath. So in the acute phase regular breathing exercises are necessary.
(2) Phase of Rehabilitation
→ So the first part of the rehabilitation phase begins. When we start to get patients moving we have to keep in mind that physiotherapy must be graduated. We realize the patients can fatigue quite quickly and so we try to build up the strength very gradually, deliberately providing a little more demand each time in exercising the respiratory muscles.
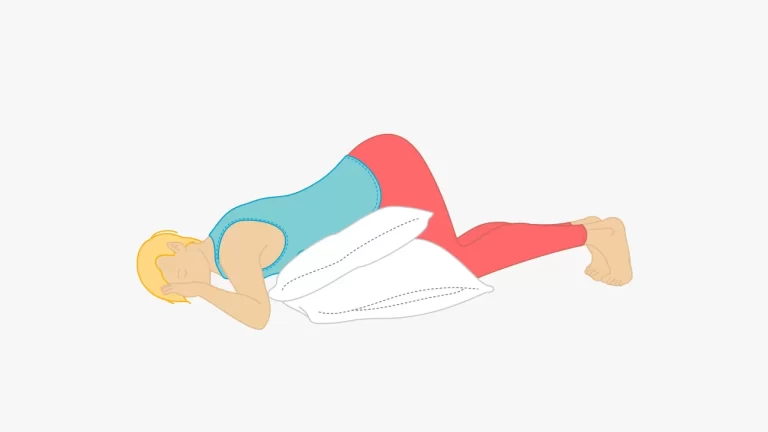
→ The positioning of the patient is vital. He/she needs to be nursed so that the lungs are kept clear – from side to side and if need be to be “jacked up” with the head down so allowing any secretion in the lungs to be drained out.
Patients suffering from GBS disease often complain of severe pain, which can be managed by applying TENS, IFT, and other pain relieving techniques.

→ If muscles are kept in a shortened position long enough then there is an increase in the stiffness of the muscle. So there should be “passive” movements, ie aided – through the full range at least once a day. If there is too much movement with weak muscles around a joint, the joint can become quite loose and set up later some pain. Too little movement and you end up with a stiff joint. You can have muscle stiffness and then joint stiffness. This again can become quite painful.
→ There are available Resting Splints for wrist/hands and ankles which can be important in the early stages. Tight calf muscles can, later on, make it more difficult for one to walk, particularly upstairs and downstairs and even on a slight slope. You get too tired.
→ The important feature at the next phase, when a patient gets out of bed, is that his/her circulation is quite dependent on the muscles in the body.
→ There will be swelling in the ankles and hands if one doesn’t move around much. So a patient’s blood pressure is monitored at this stage to check there is no sudden drop. Such patients wear elastic stockings to push the blood back to the heart and also to prevent blood clots. If the blood sits in the legs there is more potential for clotting.

→ Some patients with weak abdominal muscles may need abdominal corsets. Once the patient is getting up the whole effect of what gravity has on the joints becomes important. The shoulder joint particularly relies on the muscles around it. He/she may need the arms supported in the early stages of sitting up and walking.
→ It is important to get good seating. If necessary one can make do with a cushion, towel, or pillow to support the lumbar spine. Prolonged sitting with a curved spine can lead to small damage to the joints in your upper spine, producing backache. It is similarly important to support the middle and top of the spine as well as the arms.

→ Stretching the arms including the hands, legs feet, and body (particularly by slumping), helps to rehabilitate not only the peripheral muscles but also, we believe, the associated nerves. This is important for GBS and CIDP patients suffering from nerve damage. One has to be careful not to overstretch.

→ Functional tasks of daily living that involve exercise tend to be beneficial. These tasks include walking, repeated sitting to standing, rolling over and moving up and down in bed, and putting on and taking off clothes. These tasks help to restore the patient to normal living.
(3) Ongoing Rehabilitation
→ Hydrotherapy is fantastic as patients can float; so their weight is supported and also they can exercise against the graded resistance of the water – the faster they move the harder it is, and the slower the more gentle. It does not suit everyone – some find the heat too much.
→ It is important to watch the posture as muscle weakness can affect it. It is often the physiotherapist’s role to examine and give the patient advice about posture.
→ The patient may need balance retraining because we know the ankles are important for balance. The patient may find the hips have to be moved to keep the balance.
→ As the patient progresses we begin some training in advanced skills of walking up and down slopes and stairs.
As an ongoing practice, it is important to have regular exercises to keep stretching muscles that may be at risk of tightening up – calf muscles, hamstrings, arm muscles.
→ Hydrotherapy, walking, exercise bikes, or anything that can get a patient’s heart rate up are important for ensuring that your cardiovascular and general fitness are in good condition.
Complications in GBS:
Guillain-Barre syndrome (BGS) affects the Body’s nervous System. Because nerves control your movements and body functions, people with GBS loss Of Movement May Leads complicate other Problems These are :
Breathlessness: The weakness or paralysis can spread to the muscles around the lung that control your breathing, a potentially fatal complication. Up to 30 percent of people with GBS need temporary help ventilation to breathe when they are hospitalized for treatment.
Heart & blood pressure problems: Blood pressure fluctuations and irregular heart rhythms (cardiac arrhythmias) are common side effects of Guillain-Barre syndrome.
Pain: Up to half of people with Guillain-Barre syndrome experience severe nerve pain and back Pain which may be eased with medication.
Bowel/Bowl Incontinence: Muscles Which are Controlling the Bladder And Bowl Are Also involved leading to weakness/paralyzed leading to Bladder/Bowl incontinence.
Residual numbness or other sensations or Loss Of Movement: Most people with Guillain-Barre syndrome recover completely or have only minor, residual weakness, Loss of Movement, numbness, or tingling.
Bed sores:

Being unable to move (immobile) may lead to the risk of developing a pressure sore also called a Bedsore over a weight-bearing area. Frequent repositioning may help avoid this problem. From Supine to side lying Position, the Use of an air bed and water bed is also recommended.
Blood clotting: People who are immobile due to GBS are at risk of developing blood clots. Until you’re able to walk independently, taking blood thinners wearing support stockings and regular exercise may be recommended.
Re-occurring: Around 3 percent of people with GBS experience a redeveloping over time.
Severe, early symptoms of GBS or Delay in Treatment significantly increase the risk of serious long-term complications. Rarely, death may occur from complications such as respiratory distress syndrome and heart attack.
GBS life expectancy
The life expectancy of those who recover from Guillain-Barré syndrome is typical. When GBS symptoms are at their worst, less than 2% of cases result in death.
GBS-related causes of death frequently include:
- Pneumonia.
- Sepsis.
- Acute respiratory distress syndrome (ARDS).
- Blood clots in your lungs (pulmonary embolism).
- Cardiac arrest.
How can you Prevent GBS?
Guillain-Barré syndrome cannot usually be prevented. The reason why some patients get GBS after being ill and others don’t is unknown to researchers. However, maintaining your health as much as possible is one method you may try to reduce your risk of GBS.
These actions may assist to some extent:
- Hand hygiene is important.
- Remain away from those who are infected or who have the stomach flu.
- Maintain a healthy diet and frequent exercise to strengthen your immune system.
- Common surfaces like phones, doorknobs, toys, tables, and counters should all be cleaned and sanitized.
- Keep up with all of your vaccinations.
Conclusion
GBS is a dangerous illness that has the potential to drastically alter your health. The good news is that most GBS patients respond favorably to therapy. But it could take some time. Furthermore, the healing process can be overwhelming and draining. Recognize that your medical team will support you during the whole journey. Don’t forget to rely on your loved ones for assistance.
FAQ
What is the cause of GBS?
The illness typically manifests itself a few days or weeks following a stomach or respiratory infection. Rarely, a recent vaccine or surgery may cause Guillain-Barre syndrome. Reports of instances have been made after contracting the Zika virus. Guillain-Barre syndrome may develop following COVID-19 virus infection.
Can Guillain-Barre be cured?
A cure for Guillain-Barré syndrome is unknown. Certain treatments, however, can decrease the intensity of the disease and speed up your recuperation. Additionally, there are several approaches to treating the disease’s consequences.
How long does GBS last?
For around two weeks following the onset of signs and symptoms, the illness tends to get worse. The symptoms subside after four weeks. The period of recovery typically lasts between six and twelve months, although it can take up to three years for certain individuals.
What are the three stages of Guillain-Barré syndrome?
The progressive phase (duration: days to 4 weeks), the plateau period (duration: days to months) with minimal clinical change, and the recovery phase are the three stages of GBS. About 75% of patients will reach their neurologic function nadir by 7 days, and 98% will do so by 4 weeks.
Is GBS a serious disease?
Rarely, Guillain-Barré syndrome might result in potentially fatal conditions including severe dyspnea or blood clots. In all, 1 in 20 people will pass away from Guillain-Barré syndrome. Learn more about Guillain-Barré syndrome recovery.
Is GBS high-risk?
GBS illness may be extremely dangerous, particularly in infants.
Within the first three months of a newborn’s life, GBS bacteria are the primary cause of meningitis and bloodstream infections in the United States. Should a mother test positive for the bacterium towards the end of her pregnancy, her newborn’s chance of contracting GBS illness is elevated.
What is the best treatment for GBS?
Intravenous immunoglobulin (IVIG)
IVIG is a therapy derived from healthy antibodies found in donor blood. These are administered to assist in preventing dangerous antibodies from injuring your nerves. IVIG is administered intravenously.




11 Comments