Post-Traumatic Arthritis
What is Post-Traumatic Arthritis?
Post-traumatic arthritis is inflammation in your joints that builds after you’ve experienced trauma. It develops fast after an injury rather than over years of wear and tears like different forms of arthritis. It’s generally a temporary problem, and many patients recover in a few months.
Occasionally, post-traumatic arthritis lasts longer and evolves into a chronic (long-term) disease. It’s irregular, but you might require surgery if your symptoms are severe and restrict your quality of life. Most patient can treat their post-traumatic arthritis with lifestyle modifications and exercise, frequently as part of their recovery program from their original injury.
Epidemiology
Approximately 12% of all osteoarthritis patients in the United States are categorized as post-traumatic osteoarthritis. This indicates that over 5.6 million patients are involved in post-traumatic osteoarthritis solely in the United States. Females are more frequently involved than men.
What are the Causes of Post-Traumatic Arthritis?
The cause of post-traumatic arthritis is an acute traumatic injury to a person’s joints or junctions. Research has displayed that such damages can occur from several sources, involving:
- vehicle accidents
- sports
- falls
- military injuries
Although a single traumatic happening can cause post-traumatic arthritis, the risk also further raises with the:
- age
- multiple injuries
- people with excess body weight
Post-Traumatic Arthritis Symptoms
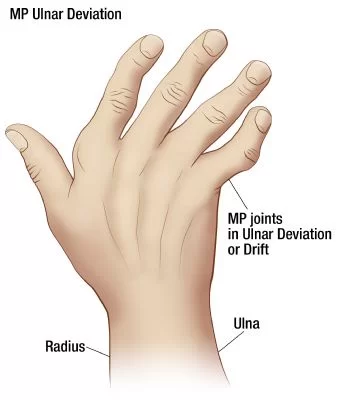
Symptoms of post-traumatic arthritis contain:
- Bone spurs
- Cracking or grating sound (crepitus) when the joint or junction moves
- Joint or junction pain
- Stiffness
- Swelling of the junction or joint
Differential diagnosis
- Osteoarthritis
- Rheumatoid arthritis
- Juvenile rheumatoid arthritis
- Various pathologies related to precise junctions or joints
Diagnosis
Your healthcare provider or doctor will diagnose post-traumatic arthritis with a physical examination and imaging examinations. Your provider or doctor will move your joint or junction, ask you about your symptoms and compare your joint or junction and its range of movement (how far you can transfer part of your body) to what it was before your injury if feasible.
What tests are done to diagnose post-traumatic arthritis?
After a physical examination, you might require at least one of a few imaging tests:
X-rays: An X-ray will verify and show how injured the bones in your joint or junction are.
Magnetic Resonance Imaging (MRI): Your provider or doctor might use an MRI to get a complete image of the injury to your joint or junction and the region near it. This will display them your bones and the tissue near them.
CT scan: If you require surgery, your provider or surgeon requires to know precisely how injured your joint or junction is. A CT scan will show them a more detailed image of your bones and the surrounding tissue than an X-ray.
How is post-traumatic arthritis treated?
Post-traumatic arthritis treatment contains:
Weight loss: Being overweight can place extra pressure on your joints or junctions.
Low-impact exercise: Activities such as swimming or biking can assist you to move your joint or junction and decrease aches while not placing your full weight onto your joints or junctions.
Physical therapy: Your provider or doctor will create customized activities and motions to improve your strength and flexibility around your involved joint or junction.
Wearing a brace: A brace around your joint or junction can assist to decrease tension on it and hold it in position.
Medical management
Conservative management is the therapy of the first option, and surgery is only considered when this fails. Surgical management will decide on the joint or junction involved, as well as the degree of injury to the joint or junction. For instance, post-traumatic hip arthritis might be controlled with a hip replacement when a conservative regime fails. Medical management can not control the condition procedure of post-traumatic arthritis, but it can be used to control the symptoms. Supplemental glucosamine and anti-inflammatory pain drugs are generally prescribed to people. Management will be very comparable to that of osteoarthritis.
Physiotherapy treatment in Post-Traumatic Arthritis
Conservative management contains:
- Activity modification
- Unloading the joint or junction with a mobility assistive gadget
- Exercise schedule aimed at recovering range of motion, strength, and coordination
- Weight management
Stretching
Stretching activities will be tailored to target your issue locations and will differ in intensity and duration relying on the expected effect. The motions will be easy to complete and only bring a few minutes of your time each day. Your muscles will gain a better stretch if they are warmed up first with some gentle motions. This leads to more suitable soft tissue extensibility and enhances the effectiveness of the stretch. Holding each stretch for about 10-15 seconds is essential to overcome the initial tension in the muscle tissue and reach lasting differences in tissue flexibility.
The main rehabilitation uses of our stretching programs contain;
- Improved range of motion
- Declines muscle tension/tone
- Gains proprioception, awareness of body position
- Enhances neuromuscular coordination
- Decreases the risk of muscular and soft tissue injury
- Enhances sweep of synovial fluid around joint or junction capsule, supplying nutrients
Range of motion
Range of motion activities will be prescribed upon the result of a physiotherapy review. This review will look at the range and the quality of the motion. Quite frequently strengthening activities are defined alongside or shortly after a range of motion activities as the raised motion at a joint or junction without raising the strength could cause another injury. Range of motion activity programs will contain:
Passive range of motion activities – where another person or another body region achieves the full motion without muscle activation
Auto-assisted range of motion exercises – where the muscles achieve the motion within the available range and then more force is used to perform a few extra degrees.
Gravity-assisted range of motion exercises – where the motion is done by muscle activation in a position where gravity can help to drag the weight of the limb to the end of the joints or junctions available range.
Range of motion exercises within the water – this can be suggested by the physiotherapist as warm water can assist to calm the tissues and raise the extensibility of the tissues improving the achievable range.
The range of motion exercises will be defined on the result of the initial review and assessment of the outcome measure. Strengthening activities may also accompany a range of motion activities.
Strength
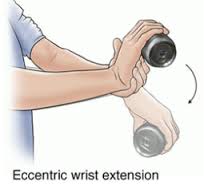
Strengthening training schedules will contain a variety of activities designed to target precise groups or individual muscles. These activities will start easier and progress as strength is invented. Some of the activities may include the next:
- Exercising opposite to the gravity
- Exercising opposite to the resistance of water
- Exercising opposite to a resistance band
- Exercising with weight
- Exercising with helping of your body weight as the load
Strengthening exercising will only be useful if the muscle is overloaded. These activities will be available to the purpose you want to perform eg. if the purpose is to be capable to flex down and pick an item up off the bottom, the functional activity would be a squat. This is because non-functional activities decrease compliance.
Heat therapy
Heat improves blood flow to the place where heat is applied. This raises the supply of oxygen, proteins, and nutrients to the site which will speed up restoration. Heat therapy has several different uses involving:
- Decrease in pain
- Decrease in joint or junction stiffness
- Muscle relaxation
- Improved flexibility
- Less inflammation
Post-traumatic arthritis surgery
Surgery for post-traumatic arthritis is irregular and is generally only a choice when your arthritis is so severe that it’s restricting your quality of life. If further therapies aren’t working or you’re still experiencing intense aches after several months, your provider or doctor might suggest surgery. Post-traumatic arthritis surgery contains:
Debridement: Debridement is how surgeons refer to washing up something in your body. This indicates removing injured tissue or reshaping your bones to repair your arthritis.
Joint fusion (arthrodesis): Your surgeon will insert a plate and pins to hold the bones of your joint or junction together. You’ll have a more steady, pain-free joint or junction, but will have restricted flexibility and motion.
Joint replacement (arthroplasty): Your surgeon will substitute your injured joint or junction with an artificial joint or junction (constructed of metal, ceramic, or plastic).
FAQ
How can I decrease my risk for post-traumatic arthritis?
Obey this general safety information to decrease your risk of an injury:
Always wear your seatbelt.
Wear the right defensive gear for all activities and sports.
Make sure your house and workspace are free from the clutter that could stumble you or others.
Always use the right tools or supplies at a house to reach items. Never stand on tables, chairs, or countertops.
What can I expect if I have post-traumatic arthritis?
You should hope to feel some pain, but therapy should decrease your stiffness, pain, and further symptoms. How long it brings to feel better relies on the original trauma that induced your arthritis. More severe injuries have longer healing timelines and are more probable to experience complications. Talk to your provider or doctor about your precise injury and post-traumatic arthritis.
How long does post-traumatic arthritis last?
Most patients have post-traumatic arthritis short-term, generally about a few months. Your symptoms might go out as your body heals from your trauma. If you experience post-traumatic arthritis symptoms for more extended than six months you could have chronic post-traumatic arthritis, which can stay for the remains of your life.
What is the outlook for post-traumatic arthritis?
Post-traumatic arthritis is something you might solely have for a few months. Though, if you have chronic post-traumatic arthritis, you’ll have to work it as a long-term disease. Your provider or doctor will assist you to find the best patterns to address your precise symptoms while you heal.
Will I need to miss work or school?
If you can accomplish your job or schoolwork without disturbing your arthritis symptoms, you shouldn’t require to neglect work or school. Talk to your healthcare provider or surgeon before continuing any physical actions while you’re healing.






3 Comments