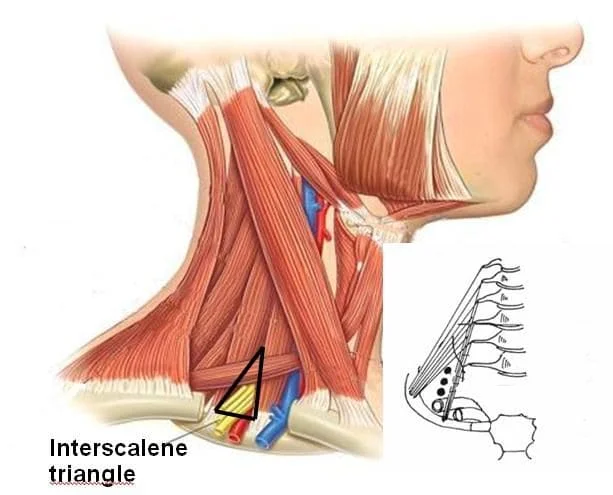
Inter-scalene Triangle
Introduction
The Inter-scalene triangle, also known as the scalene triangle, is a region of the neck with fundamental importance to the function of the upper limbs.
It is crossed by the third segment of the subclavian artery and the brachial plexus roots.
The interscalene triangle is a paired structure with an apex that points superiorly toward the base of the skull.
The first rib inferiorly, the medial border of the scalenus medius muscle, and the lateral border of the scalenus anterior muscle serve as the triangle’s edges. Thoracic outlet syndrome, which can cause vascular or neurological impairment of the upper limb as a result of compression at the interscalene triangle, is a clinical manifestation of interscalene triangle issues.
If the problem has a significant negative impact on everyday activities or compromises the upper limb, surgical decompression may be necessary.
The borders of the triangle are:
- Anteriorly: the posterior edge of the scalenus anterior muscle
- Posteriorly: the anterior edge of the scalenus medius muscle
- Inferiorly: the superior aspect of the first rib
Structure
The interscalene triangle is a paired structure with an apex that points superiorly toward the base of the skull. It is located at the root of the neck. The superior edge of the first rib forms the triangle’s horizontal base. The scalenus anterior and scalenus medius muscles make up the triangle’s two vertical sides. The prevertebral fascia of the neck, which runs from the body of the T4 vertebra up to the base of the skull, serves as the anterior covering of the scalene triangle, or the triangle’s “roof.”
Only the roots of the brachial plexus and the equivalent portion of the subclavian artery enter through the little opening between the scalenus anterior and scalenus medius muscles.
The first rib is the widest, flattest, and most curved of all the ribs. The medial half of it articulates with the manubrium sternum, and its head articulates with the body of the T1 vertebra. A subclavian artery groove and the scalene tubercle, to which the scalenus anterior is linked, can be found on its top side.
The transverse processes of the anterior tubercles of C3 to C6 give origin to the anterior scalene, which emerges as a narrow tendon at the first rib and is linked to the scalene tubercle on its upper surface. The middle scalene enters into the first rib in the quadrangular region between its neck and the subclavian groove. It originates from the lateral sections of C1 and C2 (atlas and axis), as well as the transverse processes of the posterior tubercles of C3 to C7.
Function
These muscles provide postural stability, neck flexion, and rotation, as well as first rib elevation, which reduces the amount of work required for breathing.
Embryology
The embryonic mesoderm is the source of the neck muscles as well as the anterior and middle scalene muscles. The paraxial mesoderm is divided into distinct cell masses known as somites. The sclerotome and dermomyotome are then produced by them, with the latter creating the body wall muscles.
Blood Supply and Lymphatics
At the base of the inter-scalene triangle lie the subclavian artery and vein. The subclavian artery, which arises on the right side from the brachiocephalic artery and the left side from the aortic arch, runs directly through the triangle formed by the brachial plexus. The scalene triangle is where the subclavian arteries enter after ascending superolaterally from their point of origin, curving laterally, and passing posteriorly to the anterior scalene triangle. At the triangle’s base, the subclavian vein is still visible. Weakness, numbness, and vascular impairment can result from the compression of these vascular structures.
Nerves
The anterior rami of the third through fifth cervical spinal neurons are located in the top portion of the interscalene triangle. The brachial plexus is located near the triangle’s base. The motor and sensory functions of the shoulder all the way down to the fingertips are controlled by the plexus. This plexus can sustain serious quality of life deficits as a result of injuries. The roots of the brachial plexus run via the interscalene triangle, as was previously mentioned. After passing behind the collarbone, the brachial plexus divisions stretch out distally in respect to the axillary artery until coming to an end in discrete branches that provide the upper limb’s muscle and cutaneous innervation.
The phrenic nerve travels anteriorly to the subclavian artery (C3, C4, C5) and is oblique to the anterior scalene. Although the phrenic nerve is not within the interscalene triangle, it is similar to the subclavian vein in that it is easily vulnerable to compromise from pathologies affecting the interscalene triangle due to its proximity to the triangle. The phrenic nerve controls the diaphragmatic muscles that are used for breathing.
The long thoracic nerve is another nerve that is connected to the interscalene triangle but is not actually a part of it. Its C7 branch, one of its anterior branches, crosses inside the triangle. The serratus anterior muscle is innervated by this nerve, which enters the subcutaneous layer close to the first and second ribs.
Muscles
The transverse processes of the anterior tubercles of C3 to C6 give origin to the anterior scalene, which emerges as a narrow tendon at the first rib and is linked to the scalene tubercle on its upper surface. The middle scalene enters into the first rib in the quadrangular region between its neck and the subclavian groove. It originates from the lateral sections of C1 and C2 (atlas and axis), as well as the transverse processes of the posterior tubercles of C3 to C7. These muscles provide postural stability, neck flexion and rotation, as well as first rib elevation, which reduces the amount of work required for breathing.
Physiologic Variants
The anterior scalene muscle can have several origins from C2 to C6, C3 to C5, or it can insert into the second or third rib, among other variations. Unlike the anterior scalene, the middle scalene can also insertion onto the second rib and can originate from C1 (the atlas). In some people, the scalene (more specifically the anterior scalene) may hypertrophy, which could lead to subclavian artery aneurysmal alterations in the future.
A narrow space is created on the first rib by the variable locations of the anterior and middle scalene insertions, which leads to an elevated subclavian artery and brachial plexus. When performing a surgical procedure in this region, this is crucial to keep in mind. The middle scalene may also extend the entire length of the first rib in some cases. Rarely, the middle and anterior scalene will have merged, necessitating a muscular sheath piercing to allow the artery and plexus to pass through. There are other variations besides those involving the muscles.
The first rib may contain structural irregularities that reduce the available space, such as rib fusion, unusual placement, and a healed fracture. All changes may make the structures more difficult to see and necessitate additional surgical or non-surgical treatments.
Surgical Considerations
Scalenectomy
Scalenectomy is one option for treating upper thoracic outlet syndrome, whereas a first rib resection is an alternative for treating lower thoracic outlet syndrome. For the greatest outcomes, you can also perform both treatments at the same time. In any case, they are carried out to provide the nerves and vasculature with more access to the remaining upper extremities. Both a trans-axillary and a supraclavicular approach can be used to carry out this treatment, and the available data do not show any appreciable variations in safety or complication rates between the two methods.
The first rib is removed first, followed by the identification and division of the scalenus anterior and medius muscles; however, utilizing an interscalene technique, it is also possible to perform this without dividing the scalenus anterior.
Scalpene muscle injections can also be used as a conservative measure to lessen pain rather than surgery. Patients with thoracic outlet syndrome caused by whiplash or traction injuries respond better to this injection.
Clinical Importance
Interscalene Block
Nerve blocks may be utilized to lessen the patient’s pain after surgery during the healing process. The inter-scalene nerve block, which is utilized specifically in many upper extremity injuries, is one frequently cited illustration of such a nerve block. The suprascapular, lateral pectoral, musculocutaneous, and axillary nerves, as well as a portion of the cervical plexus, can all be anesthetized using this nerve block, which can be applied either before or after shoulder surgery.
To lessen the chance of harming significant neighboring neurological structures, such as the long thoracic and dorsal scapular nerves, the needle is put mediolaterally. One prospective experiment indicated a 0.4% incidence of long-term problems following interscalene nerve blocks; nonetheless, considering the importance of the upper limb to everyday function, any impairment has a significant influence on a patient’s quality of life.
Thoracic Outlet Syndrome
With a frequency of between 3 and 8 per 1000 individuals, thoracic outlet syndrome (TOS) is a common syndrome caused by abnormal regional anatomy or injury to the related structures. The interscalene triangle is one of three locations where the vital neurovascular structures that run from the neck to the upper limb can be squeezed, which is significant. The interscalene triangle, the costoclavicular space, and the sub-pectoral space are the three areas of compression that lead to thoracic outlet syndrome.
Numerous factors, such as extra scalene muscles, congenital anomalies of the first rib, cervical ribs, fibrous bands, aneurysms, and trauma, might contribute to this illness. Indeed, the pathological group known as thoracic outlet syndrome (TOS) includes the pathological entities of neurogenic TOS (compression of the brachial plexus), arterial TOS (compression of the subclavian artery), venous TOS (compression of the subclavian vein), and disputed TOS (non-specific TOS with no obvious origin).
Due to these factors and the absence of a defined clinical diagnostic test, thoracic outlet syndrome has historically been seen as being challenging to diagnose. In addition to pain in the neck, occiput, chest, shoulder, and upper limbs, the clinical history may also include paraesthesia, weakness, or heaviness in the affected upper limb. Depending on the source and location of the compression, the patient may exhibit Raynaud’s phenomenon, upper limb ischemia, upper limb edema, cyanosis, muscle atrophy, or muscle wasting.
If this is the level of compression, palpation of the interscalene triangle may also replicate the symptoms. Due to its infamous lack of a distinct clinical manifestation, thoracic outlet syndrome.
In general, the triangle’s neurovascular structures experience compression. Because vein compression can occur in patients who do not have TOS, the compression of the subclavian artery is more diagnostic of TOS than the compression of the subclavian vein. Imaging and clinic techniques are both used in the diagnosis of this disease.
Ultrasonography, chest radiography, CT angiography, magnetic resonance angiography, specialized venography or arteriography, nerve conduction investigations, or needle electromyography are among diagnostic techniques that may be used to look into suspected thoracic outlet syndrome. Different standards may be applied to diagnose TOS. The anterior or middle scalene may be tender, there must be a positive Tinel sign, the neck tilt test must be positive, and the costoclavicular compression test must also be positive.
FAQs
What is the Interscalene triangle?
The interscalene triangle, also known as the scalene triangle, is a region of the neck with fundamental importance to the function of the upper limbs.
What are the triangles in thoracic outlet syndrome?
The initial description of thoracic outlet syndrome (TOS) appeared in 1956 and refers to a set of illnesses that cause compression of the neurovasculature leaving the thoracic outlet. The scalene triangle, costoclavicular region, and subcoracoid space are the three locations where TOS traditionally occurs.
References
Georgakopoulos, B. (2022, November 9). Anatomy, Head, and Neck: Inter-scalene Triangle. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK544222/



One Comment