Juvenile idiopathic arthritis
What is Juvenile idiopathic arthritis?
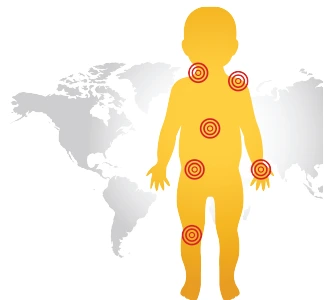
Juvenile Idiopathic Arthritis (JIA) is inflammation (swelling) of one or more of the patient’s joints. It first appears before your 16th birthday.JIA is slightly more general in girls. It most generally appears in preschool-age children or teenagers. There are various types of JIA and symptoms vary between the various types.
Knowing which kind of arthritis you have helps examine the likelihood you’ll grow out of JIA. JIA may be hard to control in some patients, but most patients will be well-controlled with treatment most of the time. If you have arthritis as part of another disease, it’s frequently managed in a very similar way to JIA.
Types of Juvenile Idiopathic Arthritis
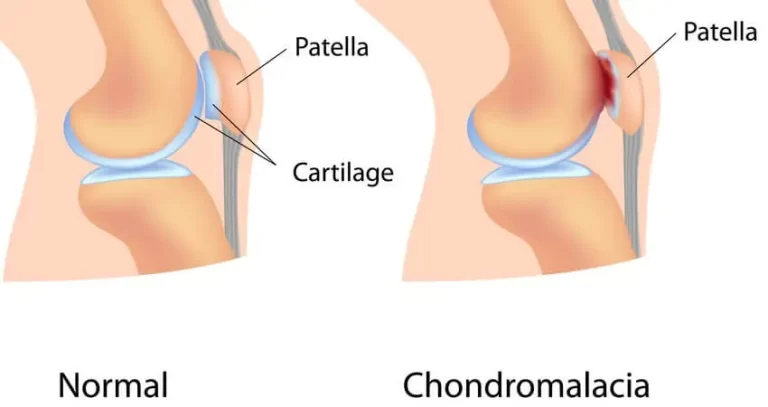
Oligoarticular juvenile idiopathic arthritis:
This is the most general and mildest form, involving four or fewer joints. It is considered constant if symptoms continue for 6 months or longer and extended if five or more joints become affected after 6 months of sickness. Generally, the involved joints are knees or ankles. A form of eye inflammation known as chronic (long-lasting) uveitis can evolve in children with this form of JIA. About half of children with Juvenile Idiopathic Arthritis-JIA have this variety.
Polyarticular juvenile idiopathic arthritis–rheumatoid factor negative:
This is the second most general variety, involving five or more joints in the first 6 months. Examinations for rheumatoid factor are negative. The rheumatoid factor blood test examines autoimmune disorders, particularly rheumatoid arthritis, which is a grown-up form of arthritis. Some of these patients evolve chronic uveitis.
Polyarticular juvenile idiopathic arthritis–rheumatoid factor positive:
A child with this variety has arthritis in five or more joints or junctions during the first 6 months of the disorder. Examination for rheumatoid factor, a marker for an autoimmune condition, is positive. It tends to happen in preteen and teenage girls, and it is seen to be essentially equal to adult rheumatoid arthritis.
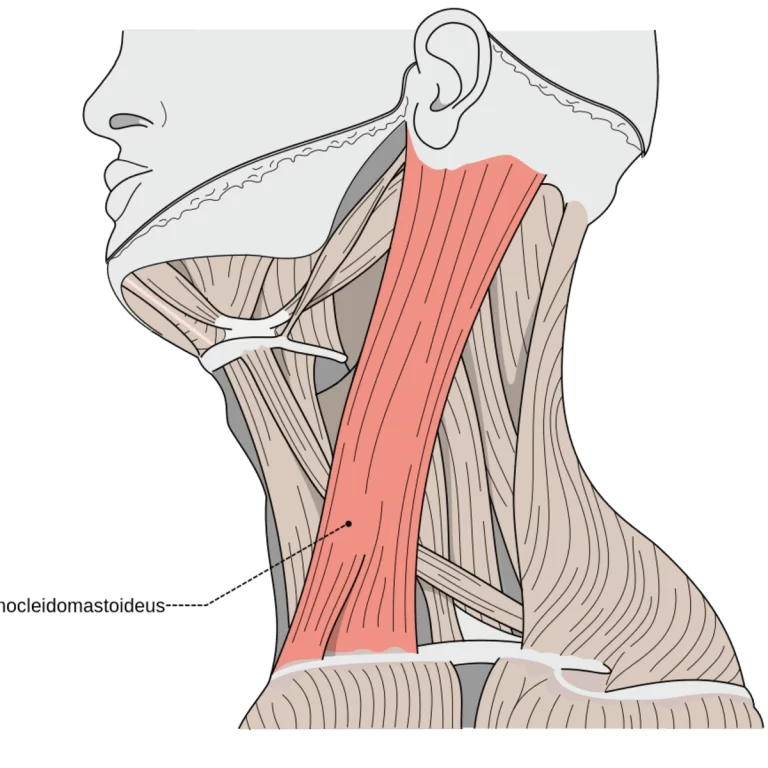
Enthesitis-related juvenile idiopathic arthritis:
This form of JIA includes both arthritis and enthesitis. Enthesitis happens when inflammation happens where a ligament or tendon connects to a bone. The most general locations for enthesitis are the knee joints, heels, and bottoms of the feet. Arthritis is generally in the knees, hips, ankles, and feet, but the sacroiliac joints (at the bottom of the back) and spinal joints or junctions can also become inflamed. Some patients get attacks of acute anterior uveitis, a sudden start of inflammation of the front of the eye. Unlike most other types of JIA, enthesitis-related JIA is more general in boys.
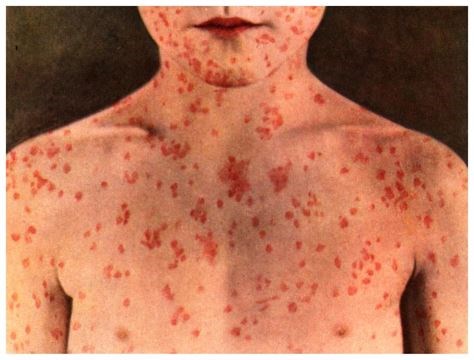
Psoriatic juvenile idiopathic arthritis:
Children with this variety have psoriasis, a skin problem, as well as inflammation of the joints or junctions. The skin disease is generally seen first, but sometimes acheful, stiff joints or junctions are the first sign, with the skin disorder occurring years later. Pitted fingernails and dactylitis (swollen fingers or toes) are also signs of the disorder.
Systemic juvenile idiopathic arthritis:
Systemic means the disorder can involve the whole body, not just a particular organ or joint. Systemic JIA generally begins with a fever and rash that arrives and goes over the span of at least 2 weeks. In many patients, the joints start inflamed, but sometimes not until long after the fever goes far, and sometimes not at all if management is started quickly. In severe types, inflammation can evolve in and around organs, like the lymph nodes, spleen, liver, and bordering of the heart and lungs. Systemic JIA involves boys and girls with the same frequency.
Undifferentiated arthritis:
This category involves children who have symptoms that do not match any of the other varieties or that match more than one type.
What are the Symptoms of Juvenile Idiopathic Arthritis?
Symptoms vary depending on the type of JIA and may involve:
- Pain, swelling, and tenderness in the joints or junctions. The joints may also sense warmth.
- Morning joint stiffness
- Limping gait (younger children may not be capable to do motor activities that they recently learned)
- Fever
- Rash
- Weight loss
- Swollen lymph nodes
- Fatigue or irritability
- Eye redness, eye pain, and blurred vision
- decreased range of motion
- redness in the involved area
What are the Causes of Juvenile Idiopathic Arthritis?
Malfunctioning of the immune system in JIA points to the bordering of the joint, called the synovial membrane. This lead to inflammation. When the inflammation is unmanaged, joint injured may possible.
It is not known what causes the protective system to malfunction in JIA. In rare patients (like in psoriatic arthritis or enthesitis-related arthritis) a parent has the same type of arthritis. Dietary and emotional factors do not seem to play a part in the development of JIA.
Because the causes of JIA are unknown, no one knows how to control these problems.
Epidemiology
JIA is the most general rheumatic disorder reported in children of the Western world. The incidence and majority ranged from 1.6 to 23 new cases for 100000 children.
JIA involves 30,000 to 50,000 children in the United States US.
JIA involves at least one 1 child in every 1,000 in Australia. For unknown reasons, it has appeared to be more prevalent in Norway and Australia.
Involves more than twice as many girls as their men counterparts.
The mean age of starting is 1-3 years old.
Risk Factors
The risk factors in a Juvenile Idiopathic arthritis patient for developing uveitis involve:
- The pattern of beginning presentation of arthritis; Oligo-arthritis
- Gender; female
- Status of the ANA; positivity
- Age at onset of arthritis before 4 years old
- Presence of HLA-DRB1or HLADRB1
- rheumatoid factor negative test
Uveitis generally presents after arthritis evolves, but 3-7% can have uveitis evolve before arthritis. The median time gap for the development of uveitis is 5.5 months. Roughly 20% of children with oligoarticular JIA (four or fewer joints or junctions affected) evolve uveitis, while polyarticular onset JIA patients feel uveitis at a lower rate (about 5%). Of those who will evolve uveitis, over 90% do so within 4 years of diagnosis of joint or junction disorder.
Diagnosis
Doctor Examination
Early diagnosis and management can assist to:
- Prevent inflammation
- Decrease pain
- Control joint damage
- Keep a child’s capability to function
- Your child’s doctor or physician will order a wide range of examinations. A complete medical history and physical observation, as well as blood tests, will assist the doctor or physician to rule out other diseases that cause arthritis.
Other tests, like ultrasounds, X-rays, and magnetic resonance imaging (MRI) scans, are sometimes used.
Medical History
Your child’s doctor or physician will review your child’s full medical history. They will like to know:
- How long your child has had trouble with joint or junctions ache and swelling
- Whether the symptoms have gotten better or severe
- Whether your child senses stiffness when getting up after bedtime
The doctor or physician will look for other causes of the symptoms, like:
- A Trauma
- Another sickness (like cancers, infections, or other autoimmune disorders)
- A family history of autoimmune disorder
Physical Examination
Your child’s doctor or physician will examine your child’s joints or junctions. They will check for signs of:
- Swelling
- Warmth
- Reduced range of motion
- Muscle loss (atrophy) in the muscles near the involved joints
Laboratory Tests
Diagnosing JIA may be hard. There is no single test to verify the disorder. Your child’s healthcare provider or doctor will take your child’s health history and do a physical examination. Your child’s provider or doctor will ask about your child’s symptoms and any recent sickness. JIA is based on symptoms of inflammation that have happened for 6 weeks or more. Examinations or tests may also be done. These involve blood tests like:
- Antinuclear antibody (ANA) and other antibody tests. These tests estimate blood levels of antibodies that are frequently seen in patients with rheumatic disorder.
- Complete blood count (CBC). This test examines for low counts of white blood cells, red blood cells, and platelets.
- Complement test. This test is done to estimate the level of complement. This is a group of proteins in the blood that assist to eliminate foreign substances. Low levels of supplements in the blood are related to immune disease.
- Erythrocyte sedimentation rate (ESR or sed rate). This test sees how faster red blood cells RBC fall to the base of a test tube. When swelling and inflammation are present, the blood’s proteins plod jointly and start heavier than normal. They fall and settle quickly at the base of the test tube. The quicker the blood cell’s RBC fall, the worse the inflammation.
- C-reactive protein (CRP). This protein is displayed when inflammation is seen in the body. ESR and CRP show equal amounts of inflammation. But one may be high when the other is not. This test may be recurrently to check a child’s response to the drug.
- Creatinine. This is a blood test to examine for kidney disorders.
- Hematocrit. This estimate the number of red blood cells RBC in a blood collection. Low levels of red blood cells (anemia) are general in patients with inflammatory arthritis and rheumatic disorders.
- Rheumatoid factor (RF). This test examines to see if RF is in the blood. This is an antibody seen in the blood of most patient who has rheumatoid arthritis and other rheumatic disorders.
- White blood cell count. This estimates the number of white blood cells WBC in the blood. Higher levels of white blood cells WBC may mean an infection. Lower levels may be a sign of some rheumatic disorders or a reaction to drugs.
- Your child may also have imaging tests or examinations. These can display how much injured the bones have. The tests may involve:
- X-rays. This test uses a small quantity of radiation to make images of bones, organs, and other tissues.
- CT scan. This uses a sequence of X-rays and a computer to make precise images of bones, fat, muscles, and organs. CT scans are more precise than regular X-rays.
- MRI. This test helps large magnets and a computer to make precise pictures of organs and systems in the body.
- Bone scan. This uses a small quantity of radiation to highlight the bones in a scanner.
Other tests may involve: - Urine tests. These are seen for blood or protein in the urine. This can indicate that the kidneys are not working well.
- Joint aspiration (arthrocentesis). A small collection of the synovial fluid is taken from a joint or junction. It’s examined to see if crystals, bacteria, or viruses are present.
A full eye examination is done by an ophthalmologist
Treatment of Juvenile Idiopathic Arthritis
There is no treatment for JIA but remission (little or no disorder activity or symptoms) is possible. Early forceful management is key to getting the disorder under control as faster as possible.
The aims of JIA treatment are to:
- Delay or prevent inflammation.
- decrease symptoms, prevent pain, and enhance the quality of life.
- Control joint and organ damage.
- Preserve joint or junction function and mobility.
- Decrease long-term health effects.
- Achieve remission (little or no disorder activity or symptoms).
Treatment for JIA varies depending on the disorder’s variety and severity. A well-rounded plan involves complementary therapies, medication, and healthy lifestyle habits.
How is juvenile idiopathic arthritis treated?
The aims of treatment are to decrease pain, decrease swelling, raise joint mobility and strength, and control joint or junction damage and complications. Treatment mainly involves drugs and exercise.
Medication
Medications used to manage JIA involve the following:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These drugs provide ache relief and decrease swelling, but do not involve the method or prognosis of JIA. Some are available over the counter and others need a prescription. NSAIDs involve ibuprofen (like Motrin and Advil and naproxen (like Aleve). These drugs can cause nausea and stomach upset in a few people and are required to be taken with food.
- Corticosteroids (steroids): Corticosteroids are frequently given as an injection (shot) into a single involved joint. These drugs can also be taken orally (by mouth) as a pill, particularly by people with more widespread disorders. Oral corticosteroids can have dangerous side effects, involving weakened bones, specifically when used for long periods. Doctors or physicians usually try to limit using long-term steroids in children because they can interrupt a child’s normal growth.
- Disease-modifying anti-rheumatic drugs (DMARDs): These drugs work by changing, or modifying, the actual disorder process in arthritis. The goal of DMARD therapy is to control bone and joint or junctions destruction by suppressing the immune system’s damage to the joints or junctions. Methotrexate is the DMARD that is most frequently used to manage JIA. Other drugs used involve sulfasalazine and leflunomide.
- Biological modifying agents: Biological agents are drugs that directly point to molecules or proteins in the protective system that is liable for causing inflammation. They are given by subcutaneous injection or intravenously and are used to manage children with worse arthritis that has not responded to other drugs. Biological agents must be used with precaution because they suppress the protective system and make children weak to infection. These medications involve infliximab, etanercept, abatacept, adalimumab, rilonacept, anakinra, and tocilizumab.
Physiotherapy Treatment
Physical therapy is an essential part of the management of JIA. It is essential for the child to remain active and participated in sports and activities with their peers and friends. While aches may limit the amount of motion a child can handle it is essential to promote involvement during periods of remission and permit rest and symptom-decreasing therapies during periods of flare-ups. Daily activity and local exercise programs assist to maintain the range of movement in involved joints, build and keep strength, keep function, and can even assist with symptom decrease.
Factors that should be focused on during a physiotherapy session are as follows:
- Muscle tone
- Strengthening
- Range of motion
- Stretching
- Education on joint protection
- Home exercise plan
- Education on pain-reducing techniques
- Muscle relaxation techniques
- Splints or Introduction to Orthotics maybe be important to help to keep normal bone and joint growth/control deformities during growth
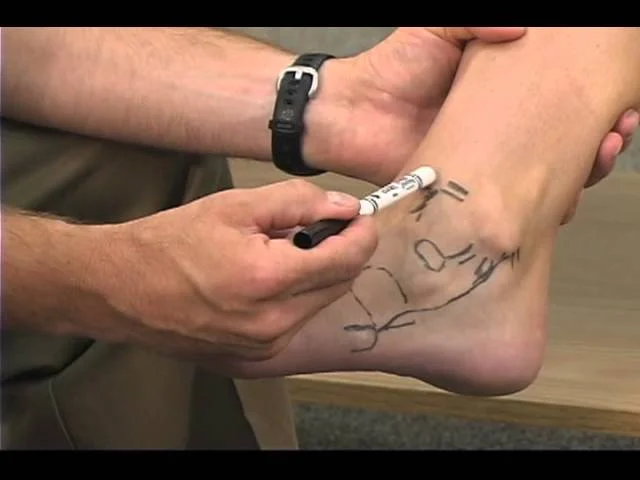
Heel and calf stretch
This stretch pointed to the muscles in your lower leg, particularly your calf muscles.
position: Stand face towards a wall.
Put your both hands on the wall and move one foot back as far as you can. Toes on both feet should be facing ahead, heels flat, with a slight flex in your knee joints.
Tilt into the stretch and hold for 30 seconds. You should experience the stretch in your back leg.
same do in opposite legs and repeat it.
Do this stretch twice for both legs with rest.

Quadriceps stretch
This stretch particularly targets your quadriceps muscle, the muscles situated at the front of your thighs. Performing this move can assist to enhance the flexibility in your hip flexors muscles and quadricep muscles.
position: Stand next to a wall or use a chair for assistance. Your feet level should be shoulder-width apart.
Flex one knee joint so your foot moves up toward your glutes muscle.
Clasp your ankle joint and slowly pull it toward your glute muscles as away as you can comfortably.
Hold it for 30 seconds.
Return to the beginning position and do the same opposite the legs.
Repeat 2 times on each side with rest.

This stretch points to your hamstrings muscle and the muscles situated in the back of your thigh.
You should experience this stretch in the back of your leg and up to the bottom of your glute muscles. If you bend your foot, you may also sense the stretch in your calf.
Start with the, you can take a rug to add cushioning under the back of the spine.
Lie down in a supine position on the ground or rug and straighten both legs. Or, if it’s more possible, you can flex both knees with your feet flat on the ground.
Raise one leg off to the ground.
Put your hands behind your thigh muscles, but below the knee joint, and slowly pull your knee joint toward your chest until you experience a slight stretch. This shouldn’t be acheful.
Hold it for 30 seconds.
Down and do the same for opposite legs.
Repeat it 2 times on each side with rest.

Half squat
Half squats are a great path to strengthen your quadriceps muscles, glutes muscle, and hamstrings muscle without straining your knee joints.
position: Get into a standing squat position with your feet level shoulder-width apart. Put your hands on your hips or out away from you for balance.
Seeing straight ahead, gently squat down roughly 10 inches. This is the central target of a full squat.
Hold for a few seconds, then stand up by forcing via your heels.
Do 10 repetitions 2 to 3 sets with rest.
Calf raises
This activity builds ups the back of your lower leg muscles, which involves your calf muscles.
position: Stand with your feet level shoulder-width apart. Position of the patient next to a wall or keep on to the back of a chair for assistance.
Raise both your heels off to the surface so that you’re standing on the front part of your feet.
Gently down your heels to the neutral position. balance is important with this activity for the buildup of your calf muscles.
Do 2 to 3 sets of 10 repetitions for both sides with rest.
Hamstring curl
The standing hamstring curl pointed to your hamstring muscle and glute muscles. It also needs well core strength to hold your upper body and hips steady.
Position: Stand face towards a wall or use a chair for assistance. Your feet level should be hip-width apart.
Raise one-foot upside, flex your knee joints, and lift your heel toward the sky. Go as away as you can, while holding your upper body still and hips pointing forward.
Hold it for 5 to 10 seconds.
Relax and down to the natural position.
Do 2 to 3 sets of 10 repetitions for each leg with rest.
Leg extensions
Using your or your patient’s body weight, instead of a weighted machine or instruments, to strengthen your quadriceps muscles helps to hold added pressure off your knee joints.
Position: Sit up tall in a chair or achieve a sitting position.
Place your feet flat on the ground and level them, hip-width apart.
See straight ahead, squeeze your thigh muscles, and straighten one leg as high as possible without lifting your buttocks off to the chair.
Hold, then down to the beginning position.
Do 2 to 3 sets of 10 repetitions for each leg with rest.
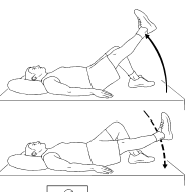
Straight leg raises
The straight leg raises the buildup of your quadriceps muscles as well as your hip flexor muscles. If you bend your foot at the last part of the move, you should also experience your shins tightening.
As this activity gets comfortable to do, you can add some ankle weight and slowly work up to a heavier weight as you grow strength in your legs.
Position: The exercise starts with, you take to use of a rug to add cushioning under the back of the spine.
Lie down on the ground in a supine position with one leg flexed and one leg extend out in front of you.
Squeezed the quadricep muscles of your straight leg and gently lift it up off the ground until it’s the same height as your flex knee joint.
Hold at the end for 5 seconds, then down to the neutral position
Do 2 to 3 sets of 10 repetitions for each leg with rest.
Side leg raises
This activity works on your hip abductor muscles as well as your glutes muscles. Your hip abductor muscles, situated on the outside of your hips, assist you to stand, walk and twist your legs with ease. Build-ups of these muscles can assist to control and manage aches in the hips and knees.
As this activity gets easier to do, you can add some ankle weight and slowly work up to a heavier weight as you grow strength in your leg muscles.
Position: Lie on your side in a side-lying position with your legs piled on the end of each other. Put your head in your hand, and put your other hand on the ground in front of you.
Lift your upper leg as high as you easily can. You should experience this on the side of your hips.
Hold briefly at the end, then down your leg.
Do 2 to 3 sets of 10 repetitions for each leg with rest.

Prone leg raises
This activity works your hamstrings muscle as well as your glutes muscle. As this activity gets comfortable to do, you can add some ankle weight and slowly work up to a heavier weight as you make strength in your leg muscles.
Position: Start with, you can take a rough to add cushioning under you.
Lie on your stomach in a prone position with your legs extending out behind you. You can put your headrest on your hands.
Amuse your glute muscle and hamstring muscles in your left leg and raise your leg as far as you easily can without causing pain. Be sure to keep your pelvic bones on the ground throughout this exercise.
Hold your leg in the raised position for 5 seconds.
Down your leg, rest for 2 seconds, then repeat again.
Do 2 to 3 sets of 10 repetitions for each leg with proper rest.
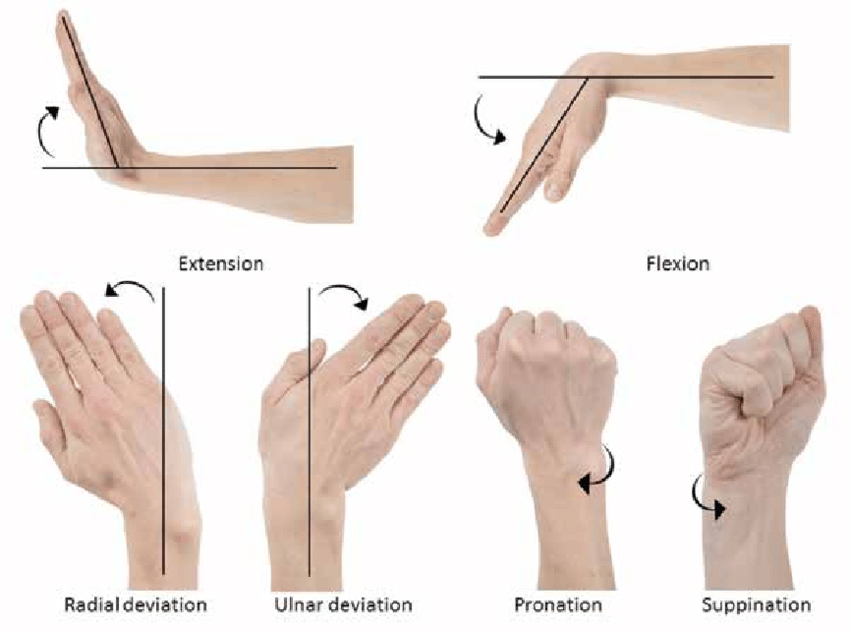
Wrist extension
To do this activity you have to Sit in a chair in a sitting position and hold a two 2-pound weight vertically in your hand, with your elbow joint keeping on your thigh.
Palm should be facing towards the floor, straighten your wrist joint by curling it far from your body.
If this is too Harding, do the motion with no weight.
Return to the starting position and do it again ten times on each side.
Wrist flexion
The wrist flexors are a bunch of muscles that use for the flexing of the wrist joint.
These small muscles that attach to your elbow joints are also subject to hyper use, which can lead to aches and inflammation over the elbow joint.
To do this activity you have to Sit in a chair in a sitting position and hold a 2-pound weight vertically in your hand, with your elbow joint keeping on your thigh.
Your palm should be facing toward the sky, bend your wrist joint by curling it toward your body. Return to the starting position and do it again ten times on both sides.
Wrist turn
To do this activity you have to bend the elbow joint up to 90 degrees with the palm facing toward the sky.
rotate the hand over gently until the palm is facing the floor.
Maintain this position for five seconds and do it again for 10 repetitions.
Wrist turn with weight
This is the same as a wrist turn but it does more with weight.
Bend the elbow joint at a right angle with the palm facing toward the sky.
Rotate the hand over gently until the palm is facing the floor.
Maintain this position for 4 to 5 seconds and do it again for 10 to 12 repetitions.
Wrist lift, palm up
To do this activity you have to clasp a lightweight, like a small dumbbell or a tin of food bend the elbow joint at a right angle then extend the hand outsides, palm facing up bend the wrist joint up towards the ceiling.
Maintain this position for five seconds, then return gently repeat these 9 more times do it 2 to 3 sets of 10 repetitions with both sides
Elbow bend
To do this activity you have to stand straight and down the arm to any one side gently bend the arm upside until the hand touches the shoulder.
Maintain this position for 20 to 30 seconds and do it 10 times for both sides.
Wrist extensor stretch
To do this stretch you have to lose your elbow joint, extend the arm, and bend the wrist joint back as if signaling stop.
It is okay to use the other hand to assist in straight the hand slowly.
Maintain this position for about thirty seconds and repeat it 5 times and do the same for the opposite side.
wrist flexor stretch
You can do this stretch take a position like a wrist extension stretch, except the wrist is bent down (opposite of “stop”).
Use the other hand to assist.
Maintain this position for 20 to 30 seconds and repeat it 5 times and do the same for the opposite side.
Fist squeeze
Take a rolled-up towel, sock, or tennis ball and put it in the palm clasp the ball or towel with the fingers to make a fist and contract tightly for 10 seconds repeat nine more times with the rest
Towel Twist
To do this exercise you have to Sit in a chair in a sitting position, clasp a towel with both hands, and your both shoulder relaxed.
Move the towel with each hand in the opposite order, as if you are squeezing out the water of washed clothes.
Repeat it 10 to 12 times, then repeat it another ten times in the opposite direction.
Biceps Curl
To do this activity you have to stand in a standing position or sit in a sitting position on a bench or chair.
With the palm facing forward. keep a 2-pound weight in both hands and the elbow joint opposite your side, and lift the elevate up toward the shoulder.
Your elbow joint should be firmly opposite your side and down the weight back to the netural position.
Triceps Extensions
To do this activity you have to Lie on your back in a supine position on a weight bench. Keep a weight beginning with the elbow joint straight.
Maintain your upper arm vertically while gently flexing the elbow joint toward the forehead. Gently return to the starting position
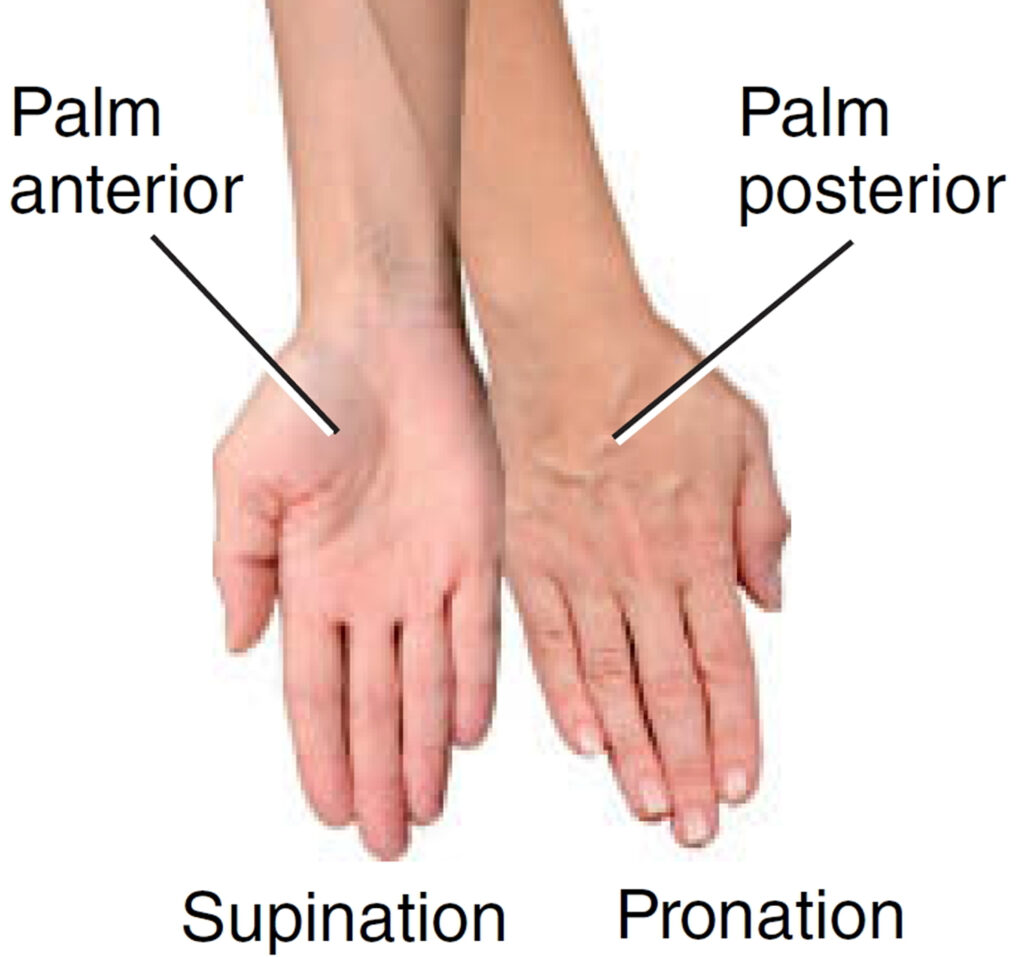
Supination and Pronation
Supination and pronation is the movement of rotating your wrist joint over to have your palm face up or palm face down.
This simple activity goal is to enhance and strengthen the rotational capacity of the elbow joint and forearm.
For this supination and pronation activity, you will require a washcloth or washcloth-sized part of the material.
To do this activity you have to Stand up straight, keeping a washcloth in your hands. Act to wring the cloth waterless for 6 seconds. Hold and repeat this movement ten times.
Change the direction in which your hands are wringing the cloth.
Repeat this ten times by altering the hands.
Ankle Alphabet
Sit down in a sitting position so that your feet don’t touch the surface.
With help of your foot write each letter of the alphabet in the air, with your big toe. Maintain the motions small, helping just your foot and ankle.
Ankle out
Create a loop out of a piece of an elastic fitness band, and keep it in place, either with the leg of a table or chair or with your opposite foot. Put one foot in the loop. Maintaining your heel fixed on the floor, rotate your toes outwards opposite the resistance of the band. Keep your foot back in the natural position gently. increase up to repeating this 10 times, and do the set three times a day with rest.
Basic balance
Take a stable object like a kitchen counter for assistance, and balance on one foot. Increase how long you do this, goal for one minute. Try to perform this three times, and do it the set twice a day.
Use any chance to practice standing on one leg – increasing it in your daily activities will assist you to improve.
When you experience confidence with this basic balance activity, you can make it difficult by standing on a cushion or pillow. Build up the quantity you do gently.
When you can comfortably balance on a pillow, and if you’re sensing confidence, go back to standing on the ground and repeat the basic balance activity with your eyes closed.
Toe Salutes
Sit in a chair in a sitting position with your feet relaxing on the surface.
Raise your big toe, while maintaining the other four toes on the surface. Keep for a few seconds; then relax and do it again.
Raise your four toes together, while maintaining the big toe on the surface. Keep for a few seconds; then relax and do it again.
Toe Splaying
Sit in a chair in a sitting position with your feet relaxing on the surface.
Widen all your toes apart as far as comfortable. Keep for a few seconds; then relax and do it again.
Toe Squeezing
Put foam toe dividers between your toes (like pedicure toe dividers).
Contact your toes together for a few seconds; then relax and do it again.
Towel Curls
Sit or achieve a sitting position with both feet relaxing flat on the surface.
Put a small towel on the surface in front of you.
Clasp the middle point of the towel with your toes and wrinkle your toes, twisting the towel toward you. Relax, then do it again.
Towel pickup
Sit down in a sitting position with a towel on the surface in front of you. Maintaining your heel on the surface, pick up the towel by wrinkling it between your toes. Repeat it 10 to 20 times. As you enhance, add a small weight, like a tin of beans, to the towel.
Toe Extension
Sit in a chair in a sitting position, with your feet relaxing on the surface.
Pick a one-foot lift and put it on the other thigh. Maintain on to your heel with one hand.
Clasp your toes with the opposite hand and flex them toward your ankle joint and keep them for a few seconds; then back toward your heel and keep them for a few seconds. Maintain your movements slow and smooth.
Repeat it again.

Some modalities that can be used to help decreased symptoms like pain are:
- Ultrasound
- Paraffin wax dips (hands and feet primarily)
- Moist compress (hot pack)
- Hydrotherapy (warm)
- Cold packs
Surgery
Surgery is rarely required in managing juvenile arthritis. In very severe types of juvenile arthritis or with very worse complications, surgery may be required to enhance the position of the joint or junction. An example of this might be when a joint or junction has to start deformed.
- Joint replacement — often used to manage adults with arthritis — has almost no place in managing children. In addition, adequate management of juvenile arthritis will cover the joint and control long-term injured that may ultimately need joint replacement.
- Cataract extraction with intraocular lens implants has been taken out with a standard of success in non-uveitic pediatric eyes but in patients of uveitis, multiple factors are involved in the final outcome.
- synovectomy
- epiphysiodesis – LLD (involved leg typically longer in oligoarticular disease)
- corrective osteotomies- extremity deformity, deferred until skeletal maturity
- arthrodesis and arthroplasty-for severe disorder
Complications
If it is not managed, JIA can lead to:
- Permanent injured to joints or junctions
- Interruption with a child’s bones and growth
- Chronic (long-term) arthritis and disability (loss of function)
- Vision difficulties, involving a loss of vision caused by uveitis (inflammation inside the eye)
- Inflammation of the membranes surrounding the heart (pericarditis) or lungs (pleuritis) in systemic JIA
- anemia
- long-term recurring pain
- joint destruction
- stunted growth
- uneven limbs
- changes in vision
- pericarditis, or swelling around the heart
- Lyme Disease
- Rheumatic fever
- Osteomyelitis
- Psoriatic arthritis
- Inflammatory bowel disease
- Leukemia
- Caffey Disease
- Chronic Eosinophilic Granuloma
- Osteoporosis
- Involutional Osteoarthritis
Lifestyle remedies
Exercising and keeping a healthful diet are essential for everyone, but they’re especially important for children who have JIA. Having your child Make the following lifestyle adjustments can assist them to deal with their symptoms more comfortably and decrease the risk of complications:
Eating well
Weight changes are general in children with JIA. Drugs may increase or reduce their appetite, causing rapid weight gain or weight loss. In such patients, a healthful diet including the right number of calories can assist your child keep an appropriate body weight. Speak with your healthcare provider or doctor about a meal plan if your child is increasing or decreasing too much weight as a result of JIA.
Exercising regularly
Exercising at least three times per week can build up muscles and enhance joint flexibility, making it comfortable to deal with JIA in the long run. Low-impact exercises, like swimming and walking, are generally best. However, it’s the best idea to speak with your child’s healthcare provider or doctor first.
Physical therapy
A physical therapist can teach your child the benefit of sticking with an exercise daily and can even suggest exercises suited to their particular condition. The therapist may recommend certain exercises that can assist to build strength and restore flexibility in stiff, sore joints or junctions. They will work with your primary healthcare provider or doctor to help control joint damage and bone/joint growth malformation.
Prognosis
Risk factors have been notifiable which are associated with a severe prognosis and development of complications.
Male gender
Young age at onset of uveitis
The short duration between the onset of arthritis and the development of uveitis
Presence of synechiae at first ophthalmologist visit
Well, control of the inflammation and a multi-disciplinary approach is key to enhancing the prognosis in the course of the disorder.
FAQ
Helping your child live with juvenile idiopathic arthritis?
Help your child treat his or her symptoms by sticking to the management plan. This involves getting full sleep. Encourage activity and physical therapy and search paths to make it fun. Work with your child’s school to make sure your child has helped as required. Work with other caregivers to assist your child take part as much as possible in social, school, and physical activities. Your child may also be educated for special specific under Section 504 of the Rehabilitation Act of 1973. You can also assist your child find a support group to be around with other children with JIA.
What is the prognosis for children who have juvenile idiopathic arthritis?
JIA involved each child differently. For some, only one or two joints are involved and the disorder is easy to maintain. For others, JIA may include many joints and the symptoms may be worse and may last longer. With early findings and management, involving physical and occupational therapy, it is likely to achieve well control of arthritis, control joint damage, and permit normal or near-normal function for most children who have JIA.
What is some advice for children living with JIA?
Children with JIA should survive life as normally as feasible. Attending school, and participating in extracurricular and family activities daily is encouraged. Activity does not cause symptoms of arthritis severe. In fact, exercise can assist to prevent deconditioning, and increase muscle power and muscle constancy to support the joints or junctions. There are no measures that show particular diets are useful for arthritis, so children can consume a standard, good-balanced diet.
What is uveitis and why do I see an ophthalmologist doctor?
Uveitis is a type of inflammation inside the layer eye. About 10-20% of children with JIA will evolve uveitis. Unfortunately, there are frequently no symptoms until the inflammation has already induced injured. To allow to detect and manage uveitis before there is injury, children with JIA require to see an ophthalmologist for often screening eye exams.
Does JIA ever go away?
For some children, yes. This is known as remission. For a few children, arthritis will go into remission only to arrive back months to years after. It is hard to indicate which children will go into endless remission and which children will require continued management into adulthood. Fortunately, advancements in the management and monitoring of JIA have enhanced the prediction for all children.



3 Comments