Lumbar Spondylolisthesis & Physiotherapy Treatment
What is a Lumbar Spondylolisthesis?
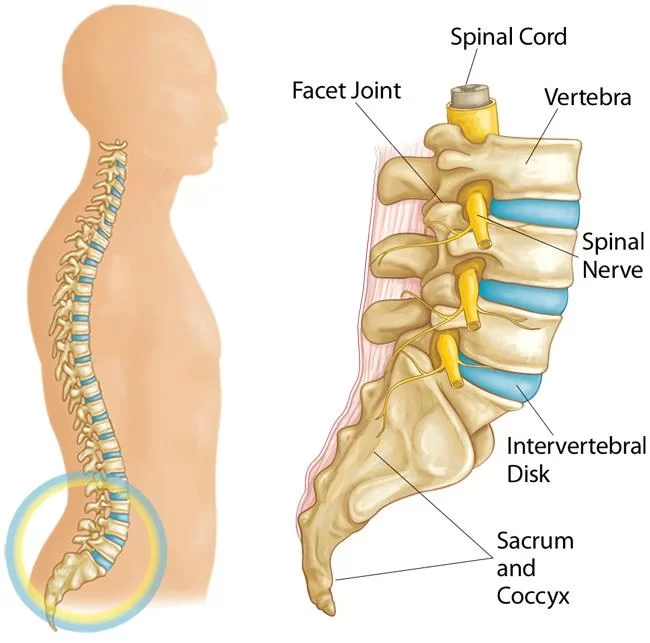
Lumbar spondylolisthesis is a condition characterized by the forward displacement of one vertebra over the vertebra below it in the lumbar (lower back) region of the spine. This displacement can cause compression of the spinal nerves and lead to symptoms such as lower back pain, leg pain, and weakness.
DEFINITION AND INTRODUCTION:
- The word spondylolisthesis derives from two parts: spondylo which means spine, and listhesis which means slippage. So, a spondylolisthesis is a forward slip of one vertebra (ie, one of the 33 bones of the spinal column) relative to another. Spondylolisthesis usually occurs towards the base of your spine in the lumbar area.
- Approximately 5%-6% of males, and 2%-3% of females have a spondylolisthesis.
- It becomes apparent more often in people who are involved with very physical activities such as weightlifting, gymnastics, or football.
- Males are more likely than females to develop symptoms from the disorder, primarily due to their engaging in more physical activities.
- Although some children under the age of five may be pre-disposed towards having a spondylolisthesis, or may indeed already have an undetected spondylolisthesis, it is rare that such young children are diagnosed with spondylolisthesis. Spondylolisthesis becomes more common among 7-10 year olds. The increased physical activities of adolescence and adulthood, along with the wear-and-tear of daily life, result in spondylolisthesis being most common among adolescents and adults.
PATHOPHYSIOLOGY:
- Spondylolisthesis can be graded according to the amount of vertebral subluxation in the sagittal plane, as adapted from Meyerding (1932):
- Grade 1 – Less than 25% of vertebral diameter
- Grade 2 – 25-50%
- Grade 3 – 50-75%
- Grade 4 – 75-100%
- Spondyloptosis – Greater than 100%
- The dysplastic type occurs from a neural arch defect in the upper sacrum or L5. In this type, 94% of cases are associated with spina bifida occulta. A high rate of nerve root compression at the S1 foramen exists, though the slip may be minimal (ie, grade 1).
- The pars interarticularis, or isthmus, is the bone between the lamina, pedicle, articular facets, and the transverse process. This portion of the vertebra can resist significant forces during normal motion. The pars may be congenitally defective (eg, in spondylolytic subtype of isthmic spondylolisthesis) or undergo repeated stress under hyperextension and rotation, resulting in microfractures. If a fibrous nonunion forms from ongoing insult, elongation of the pars and progressive listhesis results. This occurs in the second and third subtypes of type 2 (isthmic) spondylolisthesis. These typically present in the teenage or early adulthood years and are most common at L5-S1.
- A unilateral pars defect (spondylolysis) may not demonstrate any degree of slippage; thus, a patient may have spondylolysis without spondylolisthesis. The reverse is also true as in the degenerative-type slips described below.
- Biomechanical factors are significant in the development of spondylolysis leading to spondylolisthesis. Gravitational and postural forces cause the greatest stress at the pars interarticularis. Both lumbar lordosis and rotational forces are also believed to play a role in the development of lytic pars defects and the fatigue of the pars in the young. An association exists between high levels of activity during childhood and the development of pars defects. Genetic factors also play a role.
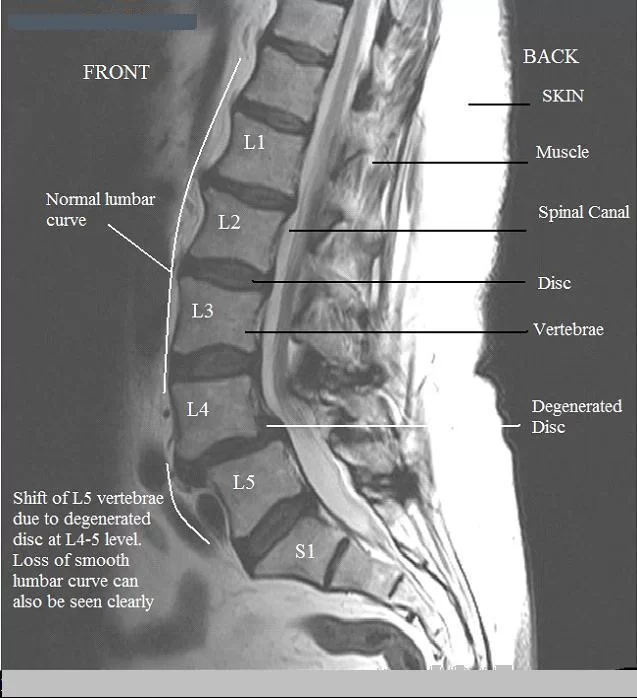
- In degenerative spondylolisthesis, intersegmental instability is present as a result of degenerative disk disease and facet arthropathy. These processes are collectively known as spondylosis (ie, acquired age-related degeneration). The slip occurs from progressive spondylosis within this three-joint motion complex. This typically occurs at L4-5, and elderly females are most commonly affected. The L5 nerve root is usually compressed from lateral recess stenosis as a result of facet and/or ligamentous hypertrophy.
- In traumatic spondylolisthesis, any part (usually not the pars) of the neural arch can be fractured, leading to unstable vertebral subluxation.
- Pathologic spondylolisthesis results from generalized bone disease, which causes abnormal mineralization, remodeling, and attenuation of the posterior elements leading to the slip.
GRADES OF SPONDYLOLISTHESIS:
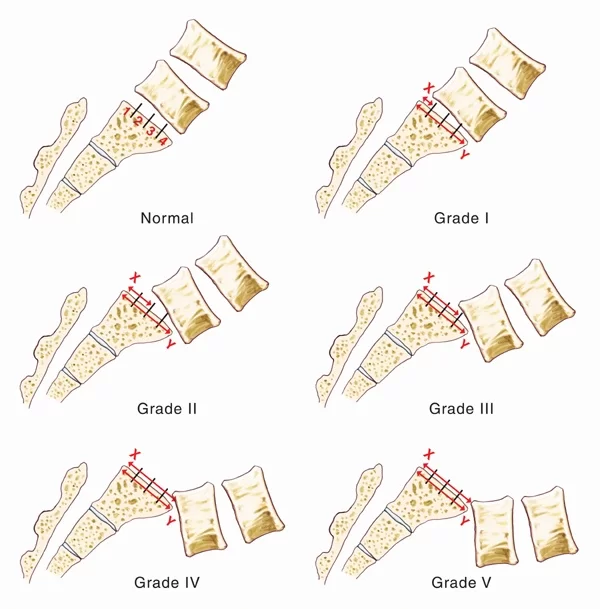
- Spondylolisthesis can be described according to its degree of severity. One commonly used description grades spondylolisthesis, with grade 1 being least advanced, and grade 5 being most advanced. The spondylolisthesis is graded by measuring how much of a vertebral body has slipped forward over the body beneath it.
- Grade 1: 25% of vertebral body has slipped forward
- Grade 2: 50%
- Grade 3: 75%
- Grade 4: 100%
- Grade 5: Vertebral body completely fallen off (i.e.,spondyloptosis)
ETIOLOGY:
- The etiology of spondylolisthesis is multifactorial. A congenital predisposition exists in types 1 and 2, and posture, gravity, rotational forces, and high concentration of stress loading all play parts in the development of the slip.
- The following scheme of spondylolisthesis types, based on etiology, is adapted from Wiltse et al.
- Type 1 – The dysplastic (congenital) type represents a defect in the upper sacrum or arch of L5; a high rate of associated spina bifida occulta and a high rate of nerve root involvement exist (see Pathophysiology).
- Type 2 – The isthmic (early in life) type results from a defect in pars interarticularis, which permits forward slippage of the superior vertebra, usually L5; there are three recognized subcategories—namely, (1) lytic (ie, spondylolysis) or stress fracture of the pars, (2) elongated yet intact pars, and (3) acutely fractured pars.
- Type 3 – The degenerative (late in life) type is an acquired condition resulting from chronic disk degeneration and facet incompetence, leading to long-standing segmental instability and gradual slippage, usually at L4-5; spondylosis is a general term reserved for acquired age-related degenerative changes of the spine (ie, diskopathy or facet arthropathy) that can lead to this type of spondylolisthesis.
- Type 4 – The traumatic (any age) type results from fracture of any part of the neural arch or pars that leads to listhesis.
- Type 5 – The pathologic type results from a generalized bone disease, such as Paget disease or osteogenesis imperfecta.
TYPES OF SPONDYLOLISTHESIS:
- (1) Developmental Spondylolisthesis: This type of spondylolisthesis may exist at birth, or may develop during childhood, but generally is not noticed until later in childhood or even in adult life.
- (2) Acquired Spondylolisthesis: Acquired spondylolisthesis can be caused in one of two ways:
With all of the daily stresses that are put on a spine, such as carrying heavy items and physical sports, the spine may wear out (ie, degenerate). As the connections between the vertebrae weaken, this may lead to spondylolisthesis. - A single or repeated force being applied to the spine can cause spondylolisthesis; for example, the impact of falling off a ladder and landing on your feet, or the regular impact to the spine endured by offensive linemen playing football.
CLASSIFICATION OF SPONDYLOLISTHESIS:
- Type I:
- Congenital (dysplastic).
- Caused by agenesis of the superior articular facet.
- Type II:
- Isthmic (spondylolytic).
- Caused by pars interarticularis defects.
- Type III:
- Degenerative.
- Secondary to articular degeneration.
- Type IV:
- Traumatic.
- Caused by fracture or dislocation of the lumbar spine, not involving the pars.
- Type V:
- Pathologic.
- Caused by malignancy, infection, or other types of abnormal bone.
- Type VI:
- Postsurgical (iatrogenic).
SYMPTOMS:
- Many people with a spondylolisthesis will have no symptoms and will only become aware of the problem when it is revealed on an x-ray for a different problem. However, there are several symptoms that often accompany spondylolisthesis:
- Pain in the low back and tenderness, especially after exercise.
- Increased lordosis (ie, swayback).
- Buttock pain.
- Numbness or weakness in one or both legs.
- Walking resembles waddling movements.
- Protruding abdomen.
- Pain and/or weakness in one or both thighs or legs.
- Reduced ability to control bowel and bladder functions.
- Tightness in hamstring muscles.
- In cases of advanced spondylolisthesis changes may occur in the way people stand and walk; for example, development of a waddling style of walking. This causes the abdomen to protrude further, due to the lowback curving forward more. The torso (chest, etc.) may seem shorter; and muscle spasms in the lowback may occur.
CAUSES:
- Spondylolisthesis has several main causes. Doctors have developed a classification system to help talk about the different causes of spondylolisthesis.
- Type I: This is also called dysplastic or congenital spondylolisthesis. Congenital means that you’re born with it. Type I spondylolisthesis, then, is a defect in the articular processes of the vertebra (the part that’s supposed to control the movement of the vertebra; your facet joints are made of the articular processes). It usually happens in the area where the lumbar spine and the sacrum come together: the L5-S1 area. The defect allows the L5 vertebra (your last vertebra in your lumbar spine) to slip forward over the sacrum.
- Type II: Also called isthmic, this is the most common kind of spondylolisthesis. With type II spondylolisthesis, there’s a problem with the pars interarticularis, a particular region of your vertebra. (You can see an illustration of this in Anatomy of Spondylolisthesis). Isthmic spondylolisthesis is divided further:
- Type II A: Gymnasts, weight lifters, and football linemen are especially prone to this kind of spondylolisthesis. It’s caused by multiple micro-fractures on the pars interarticularis—micro-fractures that occur because of hyperextension (overarching) and overuse. The pars fractures completely in type II A.
- Type II B: This type is also caused by micro-fractures. The difference, though, is that the pars don’t fracture completely. Instead, new bones grow as the pars heals, causing it to stretch. A longer pars can then cause the vertebra to slide forward.
- Vertebral FractureType II C: Like type II A, this type has a complete fracture. However, it’s caused by trauma.
- The impact in a car accident could fracture your pars, for example.
- A pars fracture can lead to a mobile piece of bone; the detached inferior articular process can actually move around. This bone fragment, also called a Gill fragment, can pinch the exiting nerve root, so the bone may need to be removed.
- Problems with the pars interarticularis can also be called spondylolysis. The word looks like spondylolisthesis, and they are somewhat related. Micro-fractures in the pars interarticularis—the kind that gymnasts, football linemen, and weightlifters are prone to—are a form of spondylolysis. The fractures are called spondylolysis; if the vertebra slips forward because it’s not being held in place properly, it’s called spondylolisthesis.
- Type III: Aging can also cause spondylolisthesis. As you grow older, the parts of your spine can degenerate; they can wear out. Usually your intervertebral discs change first. The older you get, the less water and proteoglycan content the discs have—and less fluid makes them less able to handle movement and shock. Less fluid can also cause the disc to thin, and a thinner disc brings the facet joints closer together. Without the disc acting as the cushion, the facets can’t control the spine’s movement as well, and they become hypermobile. Eventually, a vertebra can slip forward because the facets aren’t holding it in place effectively as the spine moves. Type III spondylolisthesis usually happens at the L4-L5 region (the fourth and fifth vertebrae in your low back), and it’s more common in women older than 50 years old.
- Type IV: Similar to type II C, type IV involves a fracture. However, it’s a fracture of any other part of the vertebra other than the pars interarticularis. Your facet joints, for example, can fracture, separating the front part of your vertebra from the back part.
- Type V: Tumors on the vertebra can also cause spondylolisthesis because they weaken the bones and can cause fractures that split your vertebra, leading to instability and a potential slip.
Type VI: You have this type of spondylolisthesis if surgery caused your vertebra to slip forward. It’s also known as iatrogenic spondylolisthesis, and it’s caused by a weakening of the pars, often as a result of a laminectomy (a typical back surgery, but type VI spondylolisthesis isn’t a typical result of the surgery).
As a quick summary, spondylolisthesis can be caused by: - A birth defect.
- Fractures.
- Degeneration due to age or overuse.
- Tumors.
- Surgery.
INVESTIGATION:
- X-ray.
- CT Sacan.
- MRI.
TREATMENTS:
Medications:
- Pain medications, such as acetaminophen, and/or NSAID’s (e.g. ibuprofen, COX-2 inhibitors) or oral steroids to reduce inflammation in the area.
Heat and/or ice application:

- Heat and/or ice application, to reduce localized pain. Generally, ice is recommended to relieve pain or discomfort directly after an activity that has caused the pain. Heat application is recommended to relax the muscles, and promote blood flow and a healing environment.
Physiotherapy management:
- Treatment is given according to the grades of the slip. Grade 1 and 2 can be managed conservatively, while grade 3 and 4 require surgical intervention.
- Treatment is given with the aim to achieve maximum correction of the exaggerated lordosis and then maintain the correction.
- Conservative Management usually Requires of physiotherapy Treatment:
- Some heat modality like SWD (Short wave diathermy) is given for pain relief., Interferential Therapy / TENS is very Good For Pain Relief.
- Spondylolisthesis exercises to correct the deformity:
- Exercises to induce relaxation are given.
- Strong abdominal execises are given for abdominal muscles.
- Flexion exercises for the spine, for example: sitting on a chair with back resting, then gradually bending the trunk forward from the lumbar region.

- Active posterior tilting is teach to the patient to compensate the exaggerated lumbar lordosis.
- The patient is given guidelines for correction of posture and its maintenance.
- Stretching of hamstrings is done at regular intervals.

- Patient is advised to lie prone to control the advancement of lordosis.
- A thoraco-lumbar-sacral orthoses is given to prevent the lordosis. The brace has to be worn continuously.
- Spondylolisthesis surgery is indicated when there are neurological symptoms, slip is progressing or if the pain is very intense.
- Spinal fusion is done with or without the reduction of slip, postero-lateral fusion is very common. Spinal fusion prevents further progression of the slip. The spine may be internally stabilized with the help of rods and plates.
Physiotherapy Management after Surgery:
- During Immobilization:
- Deep breathing exercises
- Early ankle, foot and arm movements are also encouraged
- Assisted movements to knee joints are given
- Isometric exercises of gluteal muscles
- Gradually hip flexion is encouraged, but it should not exceed 60 degrees.
- During Mobilization:
- Gradual mobilization of spine is initiated. The patient is encouraged to perform functional activities and to perform all the activities of daily living.
Lumbar Spondylolisthesis Exercise video
FAQs
How do you treat lumbar spondylolisthesis?
Treatment of Spondylolisthesis Without Surgery
Bracing and activity modification. Your doctor might advise resting from particular sports or activities until the pain goes away if they cause lower back pain
Physical Therapy.
Medication to relieve pain
Injections of corticosteroids
Is lumbar spondylolisthesis serious?
Generally speaking, spondylolisthesis is not a significant or risky condition. Spondylolisthesis sufferers often have minimal or no symptoms. Only when patients experience accompanying symptoms from osteoarthritis, disc degeneration, or nerve compression (radiculopathy) does spondylolisthesis become a cause for worry.
What is the best treatment for spondylolisthesis?
The success rate of surgery is high. Within a few months of surgery, people with spondylolisthesis frequently resume active lifestyles. After surgery, you’ll probably require Physical therapy exercises.
What causes lumbar spondylolisthesis?
Spondylolisthesis occurs in adults as a result of abnormal wear on the bones and cartilage caused by diseases like arthritis, trauma from an accident or injury, or as a result of a fracture, tumour, or deformity of the bone.
Can lumbar spondylolisthesis be cured?
Spondylolisthesis is irreversible from a medical viewpoint. Although non-surgical treatment options cannot stop the vertebra from slipping, they can successfully reduce patients’ pain. An operation can realign the misaligned vertebra.
Is walking good for lumbar spondylolisthesis?
Walking is frequently suggested for people with spondylolisthesis because it keeps your muscles and joints dynamic without putting additional strain on your lower back. Start off with daily 5 or 10 minute walks while maintaining a neutral spine and relaxed shoulders.





I was diagnosed with L5+S1 Gr-II spondylolisthesis in Mar2020, I opt for conservative therapy and since then doing physiotherapy exercises. I want progression and advanced home exercises for this. Now I am doing 2 times 50-60 minutes exercises advised by physiotherapist. Please tell me about your online video consultation charges.
Hello Madam,
we charged 300rs. per session on Online Video session, Nearly to 5 minute per session we give time.
if U want online consultation Please Call Dr. Nitesh Patel – Physiotherapist : mo No : 9898607803