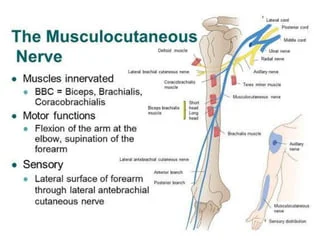
Musculocutaneous nerve
Introduction
The musculocutaneous nerve is a terminal branch of the lateral cord of the brachial plexus that carries fibers of cervical spinal nerves five along seven (i.e., C5, C6, & C7). The musculocutaneous nerve leaves the axilla & rapidly descends into the coracobrachialis muscle fibers.
The musculocutaneous nerve supplies the biceps brachii & brachialis muscles as it descends between them within the anterior compartment of the arm. The musculocutaneous nerve changes names as it passes lateral to the tendon of the biceps brachii, where it interchanges its name to the lateral cutaneous nerve of the forearm, also known as the lateral antebrachial cutaneous nerve. This nerve mainly provides motor innervation to the anterior compartment of the arm & returns cutaneous sensation from the lateral forearm.
Structure & Function of musculocutaneous nerve
The brachial plexus is the complex arrangement of nerves originating from the ventral roots of four cervical & one thoracic spinal nerve (C5-T1). The brachial plexus innervates numerous muscles & cutaneous regions of the upper limb, thorax, & back. The five ventral rami, or roots of the brachial plexus, rearrange into a superior, middle, & inferior trunk.
In turn, these trunks form six divisions (three anterior & three posteriors), which are continuous with a medial, posterior, & lateral cord. Alongside the course of the brachial plexus, 18 nerves emerge, including five terminal branches. The musculocutaneous nerve (C5-7) is an end branch of the lateral cord. The musculocutaneous nerve supplies the three muscles of the anterior compartment of the arm: the coracobrachialis, biceps brachii, & brachialis muscles. It is also responsible for the cutaneous supply of the lateral forearm.
Gross Anatomy & Course of musculocutaneous nerve
The musculocutaneous nerve may be the most appreciable nerve of the brachial plexus. When viewing the axilla, the musculocutaneous nerve can be seen arising from the lateral cord, at the inferior border of the pectoralis major muscle, & piercing directly into the deep surface of the coracobrachialis muscle. The nerve runs through the coracobrachialis an average of 5.6 cm from the muscle’s origination on the coracoid process of the scapula. It then can be seen leaving the anterior surface of the coracobrachialis to continue coursing inferiorly within the anterior compartment.
Throughout this portion of the arm, the nerve is found deep to the biceps brachii & superficial to the brachialis, & it gives off motor branches to these muscles along the way. Using the acromion process as the origin, the motor nerve branch points for the biceps brachii & brachialis were found to occur at an average distance of 13.0 cm & 17.5 cm by the side of the course of the musculocutaneous nerve, respectively. undergo given off all of its motor fibers, the main trunk of the musculocutaneous nerve continues inferiorly. A few centimeters superior to the elbow joint, it then exits the space between the biceps brachii & brachialis muscles just lateral to the biceps brachii tendon. at this point, the musculocutaneous nerve is considered the lateral cutaneous nerve of the forearm.
The lateral cutaneous nerve of the forearm pierces the deep fascia superficially to obtain access to the subcutaneous compartment. This terminal cutaneous branch of the musculocutaneous nerve gives off a ventral & dorsal branch to supply the skin of the lateral forearm. Cutaneous supplies of the medial forearm are supplied by the medial cutaneous nerve of the forearm (roots C8-T1), a direct branch of the medial cord. The posterior forearm receives cutaneous supplies from the posterior cutaneous nerve of the forearm (roots C7-C8), a branch of the radial nerve.
Blood Supply & Lymphatics
Arterial Supply
The musculocutaneous nerve runs parallel to the axillary artery proximally in the arm, but as the nerve passes into the coracobrachialis, it then takes the unique course between the biceps brachii & brachialis & does not parallel any specific artery. Nevertheless, the blood supply to the arm is managed primarily by the brachial artery, which is a continuation of the axillary artery that emerges once the vessel passes the lower margin of the teres major muscle. The brachial artery & its branches (the deep brachial, radial, & ulnar arteries) supply the muscles of the arm’s anterior compartment in addition to the other structures in the arm, forearm, & hand.
Venous Drainage
Venous drainage in the arm is primarily supplied by the cephalic vein & its tributaries laterally & the basilic vein & its tributaries medially. These two veins, next to the brachial vein deep in the arm, all drain into the axillary vein that carries blood back toward the right atrium. The cephalic vein nearby parallels with the lateral cutaneous nerve of the forearm distal to the nerve’s passage on the lateral side of the biceps brachii tendon.
Muscles
the musculocutaneous nerve supplies the three muscles of the arm’s anterior compartment. The coracobrachialis, the first muscle to receive innervation, originates from the coracoid process & inserts on the middle third of the medial aspect of the humerus. It flexes & adducts the shoulder at the glenohumeral joint. It is important to note that, unlike the other two anterior compartment muscles, the coracobrachialis does not cross the elbow joint &, thus, has no action on the elbow.
The biceps brachii muscle has a short & long head. The short head originates from the coracoid process of the scapula, whereas the long head originates from the supraglenoid tubercle of the scapula. These two heads come together to form a single tendon that inserts into the radial tuberosity & the fascia of the forearm via the bicipital aponeurosis. The biceps brachii helps to flex the elbow, as well as supinate the forearm. The biceps brachii muscle receives its innervation from the C5 & C6 fibers of the musculocutaneous nerve.
The brachialis muscle originates on the distal portion of the anterior humerus & inserts in both the coronoid process & flexion, but it is actually the brachialis that is considered the primary flexor of the elbow. The brachialis is an adaptable flexor in that it is able to flex the elbow from either a pronated or supinated forearm position.
Surgical Considerations
Surgeons always remain sharp-witted to peripheral nerve anatomy due to the relative sensitivity that many nerves have to intraoperative damage. Zlotolow & colleagues describe the many surgical exposures of the humerus & the specific nerves that may be injured with each approach. The deltopectoral make conversation, specifically for the repair of subscapularis tears, places the musculocutaneous nerve at risk.
Anterolateral approaches for the reduction of humeral fractures put the lateral cutaneous nerve of the forearm at risk. Additionally, it is noted that surgeons should avoid dissecting medial to the conjoined tendon (short head of the biceps & coracobrachialis attachment on the coracoid process) due to the risk of lesioning the musculocutaneous nerve.
- Surgery
A nerve graft from the lower leg
Peripheral nerve graft
Peripheral nerve transfer
If the injury does not seem to be healing properly, the surgeon can use EMG testing in the operating room to assess whether scarred nerves are recovering. Doing an EMG test directly on the nerve is more accurate & reliable than doing the test over the skin. - Sometimes a nerve sits inside a tight space (similar to a tunnel) & is compressed by scarring. In these cases, the surgeon may enlarge the tight space or free the nerve from the scar.
- Sometimes a section of a nerve is cut completely & damaged behind repair. the surgeon can remove the damaged section & reconnect healthy nerve ends (nerve repair) or implant a piece of nerve from another part of the body (nerve graft). These procedures can help the nerves regrow.
- If the person has a particularly severe nerve injury, the doctor may suggest surgery to restore function to critical muscles by transferring tendons from one muscle to another.
Clinical Significance
Musculocutaneous Nerve Palsy
As with all nerves, direct trauma to the musculocutaneous nerve in lacerations, gunshot wounds, & nearby bone fractures has been reported. While isolated musculocutaneous nerve syndromes are relatively rare, a few specific clinical situations have been described in the literature. Most significant is the entrapment of the musculocutaneous nerve within the coracobrachialis muscle, leading to biceps brachii & brachialis weakness & atrophy with accompanying loss of sensation in the lateral forearm. It has been found that patients most apt to develop this condition are active young individuals who frequently engage in shoulder & elbow flexion with the forearm in a pronated position. This syndrome frequently occurs next to hypertrophy of the coracobrachialis as a result of chronic overuse. It is important to observe that the compressed nerve within the coracobrachialis has already given off its motor branch to the coracobrachialis & thus will not present with defects of coracobrachialis muscle function.
Another critical clinical condition involving the musculocutaneous nerve is a shoulder dislocation. While the most frequently injured nerve in this condition is the axillary nerve, several cases of musculocutaneous nerve damage have been appearing secondary to anterior humeral dislocations. The musculocutaneous nerve branches from the lateral cord just anterior to the glenohumeral joint, explaining its sensitivity to destruct with anterior dislocations. Additionally, it has been found that downward traction & external rotation place significant tension on the nerve, & anterior humeral dislocations may place the nerve in this position.
Lateral Cutaneous Nerve of the Forearm Palsy
additionally, the musculocutaneous nerve lesions described, & the specific effect on the lateral cutaneous nerve of the forearm have also been examined. While this sensory-only lesion frequently goes unnoticed clinically, a few clinical situations are worth noting. Just before exiting the deep fascia to supply the cutaneous innervation, the lateral cutaneous nerve of the forearm passes between what has been expressed as a tunnel created by tough fascial layers of the brachialis & bicipital aponeurosis. The nerve can be compressed by bicipital aponeurosis in cases of chronic elbow extension with the forearm in a pronated position. This can cause hypesthesia in the lateral forearm area.
The lateral cutaneous nerve of the forearm travels in close proximity to the cephalic vein & thus is at risk for injury during phlebotomy procedures. General practice is to avoid the medial aspect of the cubital fossa during phlebotomy due to cases of injury to the medial cutaneous nerve of the forearm. However, cases of injury to the lateral cutaneous nerve of the forearm, similar to that described by Rayegani & Azadi, suggest that caution should be taken when using the lateral aspect of the cubital fossa. It has been suggested that using as superficial an address as possible may reduce the overall risk of peripheral nerve damage
Diagnosis
the doctor will review the medical history, ask about any accidents & previous surgeries, & discuss the symptoms with you. the doctor will also conduct a physical & neurological examination. If your neurological examination shows signs of a nerve injury, the doctor may recommend diagnostic tests, which may include:
Electromyography (EMG). In an EMG, a thin-needle electrode inserted into the muscle records the muscle’s electrical activity at rest & in motion. Reduced muscle activity can indicate nerve injury.
Nerve conduction study. Electrodes placed at two different points in the body measure how well electrical signals pass through the nerves.
Magnetic resonance imaging (MRI). MRI uses a magnetic field & radio waves to produce detailed images of areas affected by nerve damage.
Ultrasound. Like MRI, these high-frequency sound waves produce detailed images of the area affected by nerve damage
Treatment
If the nerve is injured but not cut, the injury is more likely to heal. Injuries in which the nerve has been completely severed are very difficult to treat, & recovery might not be possible.
the doctor will determine the treatment based on the extent & cause of the injury & how well the nerve is healing.
- If the nerve is healing properly, the person may not need surgery. the person may need to rest the affected area until it’s healed. Nerves recover slowly, & maximal recovery may take many months or some years.
- the person will need regular checkups to make sure the recovery stays on track.
- If the injury is caused by a medical condition, the doctor will treat the underlying condition.
- Depending on the type and severity of the nerve injury, the person may need medications such as aspirin or ibuprofen (Advil, Motrin IB, & others) to relieve the pain. Medications used to treat depression, seizures & insomnia might be used to relieve nerve pain. In some cases, the person may need corticosteroid injections for pain relief.
- the doctor may recommend physical therapy to prevent stiffness & restore function.
Role of physiotherapy in Restoring function
A number of treatments can help regain the function of the affected muscles.
braces & splints. These devices keep the affected limb, fingers, hand & foot in the proper position to improve muscle function.
Electrical stimulator. Stimulators can activate muscle given out by an injured nerve while the nerve regrows. though, this treatment may not be effective for everyone. the doctor will discuss electrical stimulation with a person if it’s an option.
Physical therapy. Therapy involves specific movements & exercises to maintain affected muscles & joints active. Physical therapy can prevent stiffness & help restore function & feel.
Exercise. Exercise can help improve muscle strength, maintain range of motion & reduce muscle cramps.
FAQ
Where is the musculocutaneous nerve most vulnerable?
axilla
outlying injury to the musculocutaneous nerve has less connected to disability than that of any other major upper extremity nerve injury. Injury is also rare as the nerve has a protected location & course, deep within the arm. It is unprotected in the axilla, which is the most common site of outlying injury.
What would happen if the musculocutaneous nerve was damaged?
outlying injury to the musculocutaneous nerve is a rare occurrence. Associated signs & symptoms of an outlying musculocutaneous neuropathy may include weakness in elbow flexion or shoulder flexion, atrophy of the biceps brachii,& pain or paresthesia at the lateral forearm.
What gives rise to the musculocutaneous nerve?
Origin. The musculocutaneous nerve originates from the lateral cord of the brachial plexus (C5-C7) at the inferior border of the pectoralis minor muscle. The brachial plexus fundamentally originates from the anterior rami of the spinal nerves C5-T1.
How do you test for musculocutaneous nerve damage?
Nerve conduction studies, electro
myography & MRI scans should confirm a lower motor neuron & sensory nerve lesion & are useful in differentiating musculocutaneous nerve lesions from cervical spine nerve root impingement.
Which muscle does the musculocutaneous nerve typically Pierce?
The musculocutaneous nerve takes origin in the lateral cord of the brachial plexus & contains fibers from C5 to C7. It pierces the coracobrachialis muscle & descends in the anterior compartment of the arm between the biceps & brachialis muscles.
How are musculocutaneous nerves injured?
It may become injured by: Brachial Plexus damage. Compression injury eg weight lifting & sports involving lots of forearm flexing & supination. The biceps aponeurosis & tendon compress against the fascia of the brachialis muscle causing loss of sensation below the elbow on the lateral aspect of the forearm.
Where can the musculocutaneous nerve be compressed?
Wasting & weakness of the biceps & brachialis muscles can occur when the musculocutaneous nerve is compressed as it passes through the coracobrachialis muscle; there may also be an impairment of sensation on the lateral side of the forearm.
How is the musculocutaneous nerve injured?
Most frequently, musculocutaneous nerve dysfunction is caused by injury to the brachial plexus, which contains numerous nerves. Typically, brachial plexus damage is caused by a penetrating injury to the axilla, like a stabbing & gunshot wound. The nerve can also be damaged during shoulder surgeries.





5 Comments