Myenteric plexus (Auerbach plexus)
Introduction
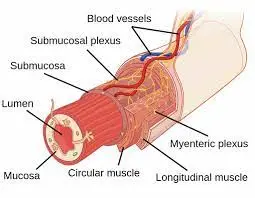
The myenteric plexus, also known as Auerbach’s plexus, is a network of nerve fibers and ganglia located in the muscular layer of the gastrointestinal tract. It is one of the two major plexuses of the enteric nervous system, which is a complex system of neurons that controls the functions of the digestive system. The other major plexus is the submucosal plexus, also known as Meissner’s plexus, which is located in the submucosa of the gastrointestinal tract.
The myenteric plexus regulates the contractions of the smooth muscle in the muscular layer of the gastrointestinal tract. It is responsible for the coordinated contractions of the muscles that move food and waste material through the digestive system. The myenteric plexus also regulates the secretion of digestive enzymes and hormones, as well as the absorption of nutrients from the digestive tract.
- Imagine if each time you needed to digest food, you had to actively manage your intestines. Fortunately, we don’t have to do that. Instead, all of the involuntary processes required to keep our bodies functioning, including those involving the intestines, are handled by our autonomic nervous system.
- For the goal of unimpeded food processing, digestion, and absorption, the gastrointestinal (digestive) tract has to have some autonomic control over its processes in order to function properly and constantly. Because of this, the digestive tract has its own neural system, known as the enteric nervous system. This system, which consists of two plexuses (myenteric and submucosal) and the ganglia that are connected to them, is embedded inside the walls of the digestive tract.
- The muscular layers of the digestive organs contain a network of autonomic motor nerve fibers called the myenteric plexus, also referred to as the Auerbach plexus. To maintain gastrointestinal tract movements, its principal function is to supply motor innervation to the muscular coat (muscular externa) of hollow alimentary canal organs. (peristalsis). The vagus nerve, which connects the central and enteric neural systems, has some influence over its operation. Numerous neurotransmitters and neuromodulators, primarily acetylcholine and nitric oxide regulate the myenteric plexus’s function.
The myenteric plexus receives input from the central nervous system and other components of the enteric nervous system, as well as from sensory receptors in the digestive tract. It integrates this input and coordinates the responses of the digestive system to maintain its proper functioning. Dysfunction of the myenteric plexus can lead to various digestive disorders, such as irritable bowel syndrome, gastroparesis, and achalasia.
Location
- The enteric nervous system has two main parts, the other being the myenteric plexus (Auerbach plexus). From the esophagus to the rectum, it is embedded in the walls of the digestive tract. In the muscular layer of hollow digestive organs, it is sandwiched between the inner circular and outer longitudinal muscle layers.
Structure
- The Auerbach’s plexus histology is still not completely understood. Myenteric ganglia and the nerves that emerge from them make up the plexus.
- inhibitory (nitrogenergic) and activating (cholinergic) neurons make up the myenteric neurons.
- Acetylcholine is used by the activating neurons to excite the smooth muscles of the hollow organs, whilst nitric oxide is used by the inhibitory neurons to suppress muscular activity.
Muscles
- Between the intestines’ outer longitudinal and inner circular smooth muscle layers is the myenteric plexus. It regulates motility along the gastrointestinal tract by provoking these muscles.
The flow of Blood and Lymphatics
- The gastrointestinal system’s blood supply is followed by that of the myenteric plexus. The foregut receives blood from the celiac artery. Alternately, the superior and inferior mesenteric arteries, respectively, supply blood to the midgut and the hindgut. Unlike the capillaries serving the other layers of the gut, the capillaries supplying the myenteric layer are peculiarly non-fenestrated.
Nerves
- The enteric nervous system, the largest subgroup of the autonomic nervous system, includes the myenteric plexus as a branch. The dorsal motor nucleus-derived vagal efferents are the primary stimulators of innervation. The pelvic splanchnic nerves also provide some innervation to the myenteric plexus. These neurons don’t directly innervate the muscle; instead, they create terminals in the myenteric plexus that resemble beads in a necklace. Additionally, intrinsic cholinergic and nitrogenergic neurons that promote peristalsis are found in the myenteric plexus. Through ICC, platelet-derived growth factor receptor-alpha, and pacemaker cells of the gastrointestinal tract, these excitatory and inhibitory neural effects are transmitted.
Function
- The myenteric plexus’ main job is to trigger the peristaltic movement of the gut. A series of muscular contractions resembling waves called peristalsis aid in the passage of food through the digestive tract. The peristaltic reflex, which is an activity of the hollow organs, is what causes the peristalsis. Mechanical stimuli or food-induced physical distension of the organ’s wall can cause the peristaltic reflex (myenteric reflex), but the response is constrained and managed by the myenteric plexus. Achalasia, Hirschsprung disease, gastroparesis, etc. are only a few examples of life-threatening conditions that can result from damage to this plexus.
- Neurotransmitters, which can cause either relaxation or contraction of these smooth muscles, mediate the function of the intestinal smooth muscle. The process of controlling motor smooth muscles involves a number of neurotransmitters. Acetylcholine and tachykinin are the major neurotransmitters that promote contraction (excitation). Nitric oxide (NO), in contrast, is a key neurotransmitter for muscular relaxation (inhibition). In addition to NO, there are purine, pituitary adenylate cyclase-activating peptides, and vasoactive intestinal peptides (VIP).
- The interstitial cells of Cajal, which are the electrical pacemakers of the gut, primarily regulate the myenteric plexus locally, allowing it to function on its own. These cells regulate and adjust the activity of the myenteric neurons and the smooth muscle of the alimentary canal in order to produce continuous and rhythmic peristalsis. Even though the myenteric plexus is capable of functioning independently, it does receive central parasympathetic inputs from the vagus nerve, allowing the physiological state of the body to affect the activity of the gut (for example, the parasympathetic activity is increased during “rest and digest” periods).
Considerations for Surgery
Achalasia
- The peroral endoscopic myotomy (POEM) operation was developed as an avant-garde method of treating achalasia. It concentrates on the smooth muscle’s inner circular layers, which contract the lower esophageal sphincter (LES). Reaching the inner circular muscle bundles requires first creating a submucosal tunnel. The outer longitudinal muscle bundles are then kept once this layer has been removed. The procedure has since been extended to include rectal endoscopic myotomy and gastric POEM (G-POEM), which are used to treat Hirschsprung disease and gastroparesis, respectively.
Causes
It is unclear what causes achalasia exactly. It might be brought on by the esophagus losing nerve cells, according to researchers. There are ideas as to why this occurs, although autoimmune reactions or viral infections have been suggested. Achalasia can very infrequently be brought on by an inherited genetic condition or illness.
Symptoms
In most cases, achalasia symptoms develop gradually and get worse with time. Some warning signs and symptoms include:
- Dysphagia, or the inability to swallow, can make you feel as though food or liquid is trapped in your throat.
- spitting up food or saliva
- Heartburn
- Belching
- chest discomfort that is intermittent
- Nighttime coughing
- Pneumonia (caused by food aspiration)
- Loss of weight
- Vomiting
Diagnosis
Because achalasia’s symptoms are similar to those of other digestive disorders, it is possible for it to be missed or misdiagnosed. Your doctor may advise: to check for achalasia.
Manometry of the oesophagus. This test evaluates your lower oesophagal sphincter’s ability to relax or open during swallowing, as well as the rhythmic muscular contractions that occur in your oesophagus when you swallow. When determining which type of motility issue you might have, this test is the most useful.
X-rays of your oesophagus, or upper digestive system. After you consume a chalky liquid that coats and fills the interior lining of your digestive tract, X-rays are performed. Your oesophagus, stomach, and upper intestine may all be seen in silhouette by your doctor thanks to the coating.
You might also be instructed to take a barium tablet, which can help to reveal whether your oesophagus is blocked.
The upper endoscope. To view the interior of your oesophagus and stomach, your doctor inserts an endoscope, a thin, flexible tube with a light and camera. If your symptoms or the findings of a barium study suggest that there may be a partial blockage of the oesophagus, endoscopy can be utilized to determine that. Endoscopy may also be used to get a tissue sample (biopsy) in order to check for reflux-related disorders like Barrett’s oesophagus.
Treatment
Treatment for achalasia focuses on loosening or stretching open the lower esophageal sphincter to allow food and liquid to pass through the digestive tract more freely.
Your age, state of health, and degree of achalasia will all influence the sort of treatment you receive.
non-surgical procedure
Nonsurgical alternatives comprise:
pneumatic expansion. By using endoscopy, a balloon is put into the esophageal sphincter’s center and inflated to widen the aperture. In the event that the esophageal sphincter doesn’t remain open, this outpatient operation might need to be repeated. Within five years, nearly one-third of patients who received balloon dilation treatment require a second procedure. Sedation is required for this treatment.
Botulinum toxin types A, or Botox. An endoscopic needle can be used to administer this muscle relaxant directly into the esophageal sphincter. It might be necessary to repeat the injections, and if so, doing so might make it more challenging to conduct surgery down the road.
Only those who are poor candidates for pneumatic dilation or surgery due to age or general health are typically advised to use Botox. Typically, Botox injections last no longer than six months. A significant improvement following a Botox injection could support the achalasia diagnosis.
Medication. Doctors mostly prescribe a muscle relaxant before meals, such as nitroglycerin (Nitrostat) or nifedipine (Procardia). These drugs have severe side effects and little therapeutic benefit. If you’re not a candidate for pneumatic dilation or surgery and Botox hasn’t worked, medications are often only considered. Rarely is this kind of therapy needed.
The Heller myotomy. In order to facilitate easier passage of food into the stomach, the surgeon trims the muscle at the lower end of the esophageal sphincter. Laparoscopic Heller myotomy is a minimally invasive way to complete the surgery. Following a Heller myotomy, some patients may go on to develop gastroesophageal reflux disease (GERD).
Surgery
Following are some surgical options for treating achalasia:
A Heller myotomy may be combined with a treatment known as fundoplication to prevent GERD issues in the future. To establish an anti-reflux valve and stop acid reflux disease (GERD) from entering the esophagus, the surgeon performs a fundoplication, wrapping the top of your stomach over the lower esophagus. Typically, a minimally invasive (laparoscopic) procedure is used to perform fundoplication.
(POEM) Peroral endoscopic myotomy. In the POEM procedure, the surgeon makes an incision in the inner lining of your oesophagus using an endoscope that is inserted through your mouth and down your throat. The surgeon next cuts the muscle at the lower end of the esophageal sphincter, much like in a Heller myotomy.
Hirschsprung disease
- A birth condition known as Hirschsprung disease, often called congenital megacolon, is characterized by the absence of ganglionic cells in the myenteric plexus in a portion of the gut. As a result, peristalsis is lost, which leads to bowel blockage. Clinically, Hirschsprung disease typically manifests as abdominal swell, bilious emesis, and meconium obstruction. This illness can develop into toxic megacolon, a potentially fatal consequence if it is not addressed.
Causes
For instance, if one parent has Hirschsprung’s disease, there is a higher likelihood that the child will as well. Hirschsprung’s illness in the mother increases the likelihood of the condition. There is a 3–12% risk that another child from the same parents will also have Hirschsprung’s disease if the family has one child who does.
Hirschsprung’s disease affects boys five times more frequently than it does girls. Children with Down syndrome are also more vulnerable.
Symptoms
abdominal distention (stomach bloating) within 48 hours of birth failure to have a bowel movement
vomiting that starts to come on gradually, fever, constipation, or an inability to pass regular stool movements
Hirschsprung’s disease symptoms that children without early symptoms may develop as they age include:
constipation that worsens with time appetite loss
stomach distention and slow development passing tiny, watery stools
Additional signs include:
swelling and pain in the abdomen.
vomit that’s brown or green.
a lot of the time bloody diarrhoea.
failure to acquire weight and a lack of appetite.
slow expansion.
Diagnosis
- A chest x-ray
- Unlike an enema. With this procedure, the doctor can check for anomalies in the large intestine. The rectum is used to administer an enema of a specific dye that may be detected on X-rays. This produces a clearer X-ray and improves the doctor’s understanding of the situation for your child.
- recti biopsy. As a result, we have a piece of the rectum to examine under a microscope to determine whether or not ganglion cells and hypertrophic nerve trunks (thickened, larger bundles of nerve fibres) are present.
- Other tests may indicate the possibility of Hirschsprung’s when they come back abnormal. For this diagnosis to be confirmed or ruled out, your kid may require more tests or a biopsy.
- Anorectal measurement. Rectal nerve reflexes, which are the main signs of Hirschsprung’s disease, are measured by this non-invasive test. The best test to determine whether your child needs a biopsy is this one.
- stomach x-ray. This examination can reveal blockage symptoms as well as enlarged sections of the large and small intestines.
- Barium dialysis. This method is used to check for anomalies in the large intestine. The rectum is used to administer an enema of barium, a liquid that coats the inside of the organs to make them visible on an X-ray. This produces a clearer X-ray and improves the doctor’s understanding of the situation for your child.
- rectum or large intestine biopsy.
Treatments
injections of Botulinum toxin (Botox) into the anal sphincter in order to relax this muscle
further removal of an unusual intestine appendicostomy, a surgical procedure to flush out and empty the colon by creating an opening outside the belly Program for Bowel Management
Mu-opioids
- Mu-opioids have pharmacological effects on every part of the digestive system. These drugs inhibit peristalsis, stimulate pyloric tone, lengthen transit time, and enhance the tone of the anal sphincter primarily on the myenteric plexus of the longitudinal muscle layer. Mu-opioids prevent the release of acetylcholine and nitric oxide at the cellular level.
Gastroparesis
- In the absence of a mechanical obstruction, gastroparesis is a delayed stomach emptying. Patients have symptoms such as belching, bloating, early satiety, postprandial fullness, and vomiting. Extrinsic neural control, intrinsic nerves, interstitial cells, and smooth muscle action are all affected by gastroparesis. The most typical cause of gastroparesis is diabetes. Additionally, it could be idiopathic, linked to neurological conditions, brought on by a bacterial or viral infection, or result from surgery. Gastric emptying scintigraphy is used in diagnosis. Metoclopramide is the only medication for gastroparesis that the FDA has approved. Both D2 and 5HT4 receptors are affected by it.
Diagnosis
Gastric emptying tests
- Scintigraphy. This is a very important test used in making a diagnosis of gastroparesis condition. A scanner that detects the movement of the radioactive material is placed over the belly while a light meal is consumed, such as eggs and toast, in order to track the speed at which food exits the stomach.
Any medications you are taking that can slow down or lessen stomach emptying must be stopped. Inquire with your doctor about any medications that can hinder or slow down digestion.
- Breath tests. For breath tests, you consume a solid or liquid food that comprises a substance that absorbs by your body. Eventually, the substance can be found in the breath samples taken over a period of time, and the amount of the drug in them is measured.
By counting how much of the chemical is in your breath after consumption, the test can determine how quickly your stomach empties.
- Endoscopy of the upper digestive system
Your esophagus, stomach, and duodenum—the first part of your small intestine—are all visually inspected during this process. On the end of a lengthy, flexible tube is a tiny camera that is used. Another disorder that may present with symptoms similar to gastroparesis is peptic ulcer disease or pyloric stenosis, which can be diagnosed with the same test.
- Ultrasound
High-frequency sound waves are used in this test to create photographs of the internal structures in your body. If you have symptoms that could be related to your gallbladder or kidneys, ultrasound can aid with the diagnosis.
Treatment
- Medication to activate the muscles of the stomach. Metoclopramide (Reglan) and erythromycin are two of these drugs. Serious adverse reactions are possible with metoclopramide. Over time, erythromycin may become less effective and may have undesirable side effects, like diarrhea.
- Domperidone is a more recent drug with fewer adverse effects that are also accessible under certain conditions.
- drugs that prevent nausea and vomiting. Ondansetron (Zofran) and diphenhydramine (Benadryl, among others) are medications that reduce nausea and vomiting. If nausea and vomiting continue, prochlorperazine (Compro) is given.
surgical procedure
- Some gastroparesis sufferers might not be able to handle any food or liquids. In some cases, doctors could advise having a feeding tube (also known as a jejunostomy tube) inserted into the small intestine. Or, to help relieve pressure from gastric contents, doctors might advise using a gastric venting tube.
- Feeding tubes can be inserted into your small intestine through your skin, nose, or mouth. The tube is often only used temporarily and only when blood sugar levels cannot be controlled by conventional means or when gastroparesis is really severe. Some people might need an IV (parenteral feeding tube) that inserts into a chest vein.
Diabetic enteric neuropathy
- It is hypothesized that the region-specific thickening of the endothelial basement membrane of the capillaries supplying the myenteric ganglia in the gut is caused by a local decrease in matrix metalloproteinase 9 (MMP9), which causes an accumulation of extracellular matrix and, in turn, causes diabetic enteric neuropathy.
FAQ
What distinguishes the myenteric from Meissner’s plexus?
The myenteric plexus, also called Auerbach’s plexus, is situated between the circular and longitudinal muscle layers of the small and large intestine, stomach, and esophagus. Between the circular muscle and mucosa, in the submucosal region, lies where the submucosal plexus, also known as Meissner’s plexus.
What is secreted by the myenteric plexus?
The myenteric plexus’ main job is to trigger the peristaltic movement of the gut. Food is moved through the digestive tract by a wave-like muscle contraction called peristalsis. The peristaltic reflex, which is an activity of the hollow organs, is what causes the peristalsis.
What does the Auerbach plexus do?
The Auerbach or myenteric plexus is the term used to describe the gut. The peristaltic waves that transport digestive byproducts from the mouth to the anal opening are controlled by neurons in this plexus. Myenteric neurons also regulate regional muscle contractions in charge of stationary mixing and churning.
What is the histology of the myenteric and Auerbach’s plexus?
Standard histology. In the colon, the myenteric plexuses with ganglia can be detected. Between the inner circular and outer longitudinal muscle layers lie these myenteric (Auerbach’s) plexuses. The mucosa may be observed at the far right, followed by a thin muscular mucosa and a submucosa.
Where is the Auerbach Plexus?
The coordination of intrinsic (entero-enteric) and extrinsic (under the influence of the central nervous system [CNS]) information, and subsequent regulation of GI motility, are primarily the responsibility of the myenteric plexus (Auerbach’s plexus), which is situated between the longitudinal and circular muscular layers.
What layer is Auerbach’s plexus located in?
muscle extensor
Between the circular and longitudinal smooth muscle layers of the muscularis externa is where Auerbach’s plexus is situated.
What are the two plexus kinds in Git look like?
The myenteric plexus (Auerbach’s plexus) and the submucous plexus (Meissner’s plexus) are two significant nerve centers that are implicated.
What part does the submucosal plexus play in the digestive process?
The submucosal (Meissner) plexus perceives the lumen environment, controls gastrointestinal blood flow, and also governs the activities and secretion of epithelial cells.



One Comment