Osteitis Pubis
What is Osteitis Pubis?
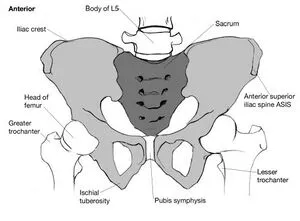
Osteitis pubis is a condition characterized by inflammation and pain in the pubic symphysis, which is the joint located at the front of the pelvis between the pubic bones. It is commonly seen in athletes, especially those involved in sports that require repetitive twisting and turning movements, such as soccer, hockey, or running.
If you have osteitis pubis, it could be uncomfortable and challenging (or impossible) to participate in your favorite physical activities. The good news is that most people may resume exercising or participating in sports after a few months of recovery. Surgery is a possibility if your symptoms don’t go away after a few months, despite the fact that it’s unusual.
Who does Osteitis Pubis affect?
- Male or female, everyone can irritate their pubic symphysis. However, those who are extremely active or athletes who often twist, kick, or suddenly change directions with their hips and core are more likely to develop osteitis pubis. The following sports are among those that might cause osteitis pubis:
- Soccer.
- Hockey.
- Marathon running.
- Basketball.
- Martial arts.
- Osteitis pubis is also more common in those who are pregnant, recently gave birth, or recently underwent surgery close to their abdomen.
How common is Osteitis Pubis?
Pubic osteitis is a rare condition. Osteitis pubis, in the opinion of specialists, accounts for less than 15% of instances of groin pain.
How does Osteitis Pubis affect my body?
Normally, your pelvis and pubic symphysis stretch together when you move, bend, and twist. It is where your two pubic bones converge. The ligaments that hold the joint together prevent your pelvic bones from shifting or moving too much.
The cartilage in your joint is irritated and inflamed if you have osteitis pubis, which can make it unpleasant or difficult to move about and engage in any physical activity.
The exact cause of osteitis pubis is not fully understood, but it is believed to result from repetitive stress or overuse of the muscles, tendons, and ligaments around the pubic symphysis. The condition can also be associated with pelvic instability, muscle imbalances, or previous trauma to the area.
What are the symptoms of Osteitis Pubis?
The main symptom of osteitis pubis is pain, which is typically felt in the groin area and may radiate to the lower abdomen, hips, or thighs. The pain is usually worsened by activities that involve the pelvis, such as running, kicking, or changing direction. Other symptoms may include tenderness over the pubic bone, stiffness, and difficulty with activities that require hip movement.
- Lower abdominal or groin discomfort (a dull ache that becomes worse as you move or is persistent).
- Symptoms of thigh adductor (inner thigh) muscle pain.
- Difficulty walking the way you usually can.
- A sensation of pressure or stiffness over your pelvis.
- Swelling.
- Pain in or near your genitals.
Causes:
- Playing a spot
- Pregnancy
- Gynecologic surgery
- Urologic surgery
- Major trauma
- Repeated minor trauma
- Rheumatological disorders
- Pregnancy/childbirth
- High level of athletic activity
- Urological or gynecological surgery
- Trauma
- Psoriatic arthritis
- ankylosing spondylitis
- Other related health conditions
Playing a spot:
Osteitis pubis is most frequently caused by sports-related injuries. Athletes who repeatedly strain the pubic symphysis’s muscles, tissues, and supporting components risk irritating the joint.
Pregnancy:
Osteitis pubis can be brought on by pregnancy or protracted labor. Additionally, some women get osteitis pubis after giving birth.
Surgery:
Some surgical procedures near your abdomen or groin, often urological procedures, might result in osteitis pubis as a side effect. You could get extra testing following surgery to check for an infection. Osteitis pubis symptoms can also be caused by osteomyelitis, an infection of the bone.
Other health conditions:
Osteitis pubis can be brought on by any illness or injury that alters your stride or how your hips and pelvis are placed. Due to alterations in how their hips move, those who have cam-type femoroacetabular impingement (FAI), also known as hip impingement, are more susceptible to developing osteitis pubis.
Overload training errors:
- Exercising on hard surfaces (like concrete)
- Exercising on uneven ground
- starting a fitness regimen after a protracted unemployment
- Increasing exercise intensity or duration too quickly
- Exercising in worn-out or ill-fitting shoes
Biomechanical inefficiencies:
- improper body and foot mechanics as well as gait disruptions
- Poor running or walking mechanics
- Muscles in the hips, groin, and buttocks that are tense and rigid
- Muscular imbalances
- Leg length differences
Epidemiology:
The real incidence of osteitis pubis has not yet been determined by an epidemiological investigation. The prevalence among athletes has been observed to range from 0.5% to 8%, with distance runners and athletes in kicking sports, particularly male football players, having a greater frequency (10% to 18%).
Pathophysiology:
The pubic symphysis is an amphiarthrodial, non-synovial joint that separates hyaline cartilage with a fibrocartilaginous disc in between. Due to the stiff ligamentous complex, the joint seldom moves much. The adductor complex and the rectus abdominis are both derived from the pubic symphysis. The rectus abdominis, which elevates the pubic symphysis while the adductors depress the joint, has an antagonistic character, which acts as a nidus for the development of osteitis pubis.
Repetitive usage of the anterior pelvic muscle causes chronic tendinosis. Chronic muscle imbalance leads to inappropriate pressures being applied across the pubic symphysis, which leads to symphyseal instability, a stress reaction in the pubic bone, and finally hyaline cartilage degradation. According to a newer viewpoint, more compensatory motion across the pubic bone causes the development of osteitis pubis.
Differential Diagnosis:
- Athletic public
- Osteomyelitis
- Groin Strain – Adductor strain
- Rectus Abdominus strain
Diagnosis
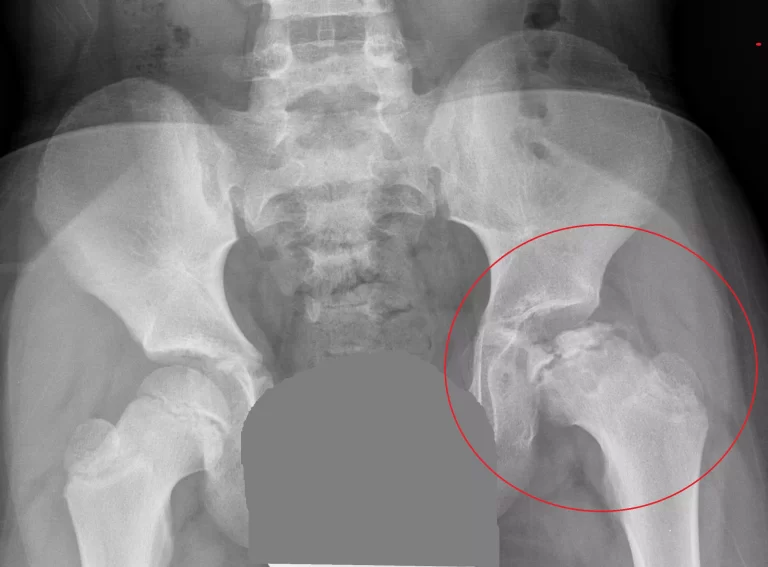
- X-ray
- Ultrasound
- MRI
- CT scan
- Bone scan
- Blood and urine test
Treatment of osteitis pubis:
The treatment mostly are a combination of rest, physical therapy, and anti-inflammatory pain-relieving medications. Resting from activities that aggravate the symptoms is important to allow the inflamed tissues to heal. Physical therapy may focus on strengthening the muscles around the pelvis, improving flexibility, and correcting any imbalances or movement dysfunctions.
In severe cases of osteitis pubis that do not respond to conservative treatment, more invasive interventions such as injections of corticosteroids or platelet-rich plasma (PRP) may be considered. Surgery is rarely needed and is usually reserved for cases that do not improve with conservative measures.
It’s important to consult with a healthcare professional if you suspect you have osteitis pubis or if you’re experiencing persistent pelvic or groin pain. They can provide an accurate diagnosis and develop an appropriate treatment plan tailored to your specific condition.
Physiotherapy treatment of osteitis pubis:
You may be able to heal and stop reoccurring issues with the use of exercises to help strengthen the muscles surrounding the pubic symphysis. You shouldn’t perform these workouts if you’re still in discomfort.
Transversus abdominis retraining:
Transverse abdominals are a group of deep core muscles that encircle your abdomen. They are essential muscle that helps to keep your pelvis stable.
The following transverse abdominal workout may be performed while laying down, or you can do a standing or sitting variation of it.
Contract your abdominal muscles while resting on your back and imagine dragging your belly button towards your spine.
Hold on to this position for a while. Avoid raising your ribcage.
Apart from your abdominal muscles, try to maintain the rest of your body in a relaxed state.
Three to four times a day, repeat this exercise.
Adductor stretch:
On the interior of your thigh are the adductor muscles.
Try the following stretch to assist these muscles, which support the pubic bones, become more flexible and strong.
Lunge to the left while maintaining your right leg straight. You should be standing with your back straight and your legs wider than shoulder width.
Your right leg ought to feel stretched.
Hold without straining or exaggerating the lunge for 10 to 15 seconds.
Return to your starting position gradually.
Keep your left leg straight as you lunge to the right.
Return to your starting posture after holding until you experience a stretch.
Rest: Acute inflammation can go away with rest. Sleeping flat on your back while recovering might lessen discomfort.
Ice and heat application: Inflammation can be reduced by using ice packs. Once the initial swelling has subsided, heat can aid with pain management.
Anti-inflammatory medication: NSAIDs sold without a prescription, such as Advil (ibuprofen) and Aleve (naproxen), can lessen both pain and inflammation.
Assistive walking devices: Crutches or a cane may be advised if the symptoms are severe in order to lessen pressure on the pelvis.
Summary:
Osteitis pubis is an inflammation of the pelvic symphysis, the joint that links the pelvic bones. One of the symptoms is pelvic discomfort in the middle. Additionally, there might be clicking, cracking, or hobbling noises when moving. Walking, sprinting, climbing stairs, lying on your side, changing directions, coughing, or sneezing can all cause pelvic pain.
The majority of sportsmen who play sports that call for kicking, rotating, or changing directions are more likely to develop osteitis pubis. Football, soccer, and hockey players are frequently impacted. Injuries, pregnancy, and delivery can all lead to osteitis pubic.
FAQ:
What osteitis pubis signs and symptoms are there?
Symptoms of thigh adductor (inner thigh) muscle pain.
Difficulty walking the way you usually can.
A sensation of pressure or stiffness over your pelvis.
Swelling
What triggers osteitis pubis?
Inflammation around the pelvic center is a painful symptom of osteitis pubis. Because the muscles in the hip and leg are overused, it typically happens as a sports injury. It occurs often in athletes who participate in sports like football or hockey that call for pivoting, kicking, or shifting direction.
What is osteitis pubis stage 3?
Your entire pelvis feels like it is collapsing in on you. Even worse, coughing could make the discomfort worse. You could be given scans at this point. These indicate pelvic sclerosis, pubic symphysis enlarging, or other grave pelvic conditions.
How is pain in the pubis treated?
Taking NSAIDs.
Wearing comfortable shoes.
an ice pack or Hot Pack on your painful pelvic area.
Sleeping with a pillow between your legs.
Wearing a pregnancy belt (pelvic support belt).
when getting out of your automobile, squeeze your legs together.
Does an MRI reveal osteitis pubis?
The most trustworthy MRI findings of the chronic condition that has been present for more than six months include osteophytes (or pubic beaking), subchondral sclerosis, subchondral resorption, and bony edge abnormalities.




One Comment