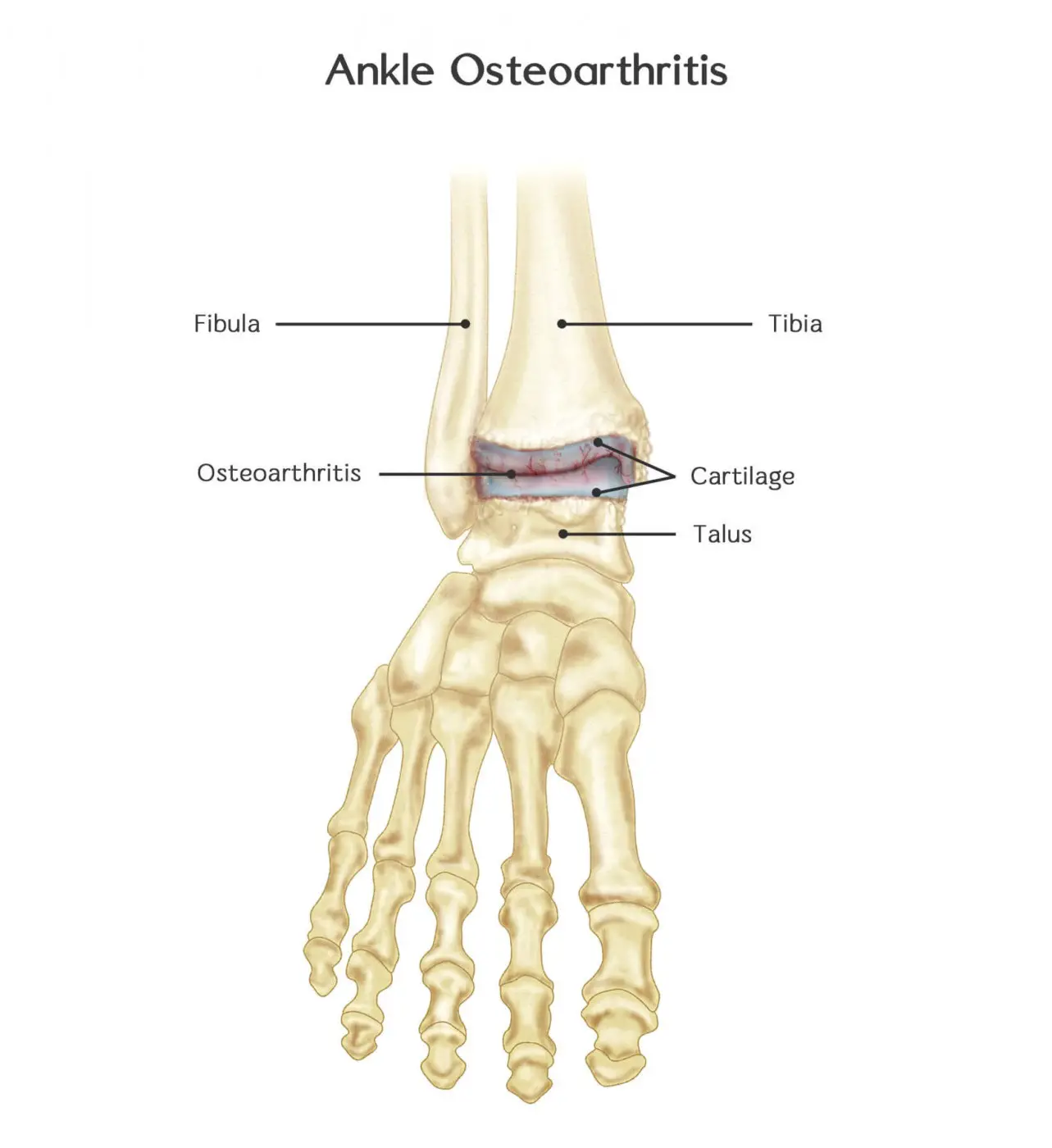
Osteoarthritis Of Ankle And Physiotherapy Treatment
- Ankle osteoarthritis is the occurrence of osteoarthritis (OA) in the ankle joint. The ankle joint consists of two synovial joints, namely the talocrural joint and the subtalar joint.
- In both joints, osteoarthritis can be diagnosed in the medial and the lateral compartment.
- The ankle joint is far less commonly affected by arthritis than other major joints.
- The reasons for this include differences in articular cartilage, joint motion, and the susceptibility of cartilage to inflammatory mediators.
Anatomy Related to Osteoarthritis Of Ankle
- Osteoarthritis of the ankle can occur in the joints of the Ankle, the main two being the Talocrural (True ankle joint) and Subtalar joints.
- There is also a third ankle joint the Inferior Tibiofibular joint which does contribute to movement at the ankle but much less than its’ counterparts and, subsequently will be less of a focus.
Talocrural Joint
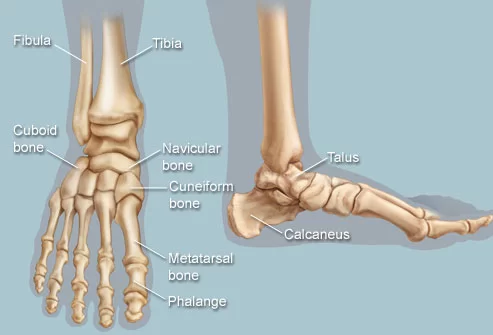
- The ankle joint is a synovial hinge joint comprised of hyaline-covered articular surfaces of the talus, the tibia as well and the fibula, allowing up to 20 degrees dorsiflexion and 50 degrees plantarflexion.
- The distal ends of the tibia and fibula are held together firmly by ligaments of the medial (Deltoid) and lateral ligament complexes of the ankle which can be damaged and contribute to ankle arthritis (Ankle Sprain).
- The ligaments hold the tibia and fibula into a deep bracket-like shape in which the talus sits.
The Talus
- The ROOF of the joint is the distal inferior surface of the tibia
- The MEDIAL SIDE of the joint is formed of the medial malleolus of the tibia
- The LATERAL SIDE of the joint is formed of the lateral malleolus of the fibula.
- The articular part of the talus looks like a cylinder and fits snugly into the bracket provided by the syndemosis of the tibia and fibula, when looking down upon the talus the articular surface is wider anteriorly than posteriorly.
- Subsequently, this increases the congruent, stable nature of this joint when it is in dorsiflexion. As this is a synovial joint, a membrane is present as well as a fibrous membrane providing the same functions as any other synovial joint synovial membrane.
Subtalar Joint
The Subtalar joint is also known as the Talocalcaneal joint and is between:
- The large posterior calcaneal facet on the inferior surface of the talus; and
- The corresponding posterior facet on the superior surface of the calcaneus
- This joint, due to its orientation, allows the movements of inversion (0-35 degrees) and eversion (0-25 degrees), broken down this must mean the joint allows some amount of glide and rotation.
- It is known as a simple synovial condyloid joint. There are a large number of strong ligaments supporting the:
- Anterior talocalcaneal ligament
- Posterior talocalcaneal ligament
- Lateral talocalcaneal ligament
- medial talocalcaneal ligament
Etiology of Osteoarthritis Of Ankle
- There are 2 types of Osteoarthritis: primary and secondary
Primary Osteoarthritis
- This is a form of osteoarthritis in which you don’t know what could trigger the disease. You can’t infer anything from history, nor clinical or radiographic examination.
- Compared with results reported for knee and hip, there is a substantially lower rate of primary ankle OA. Although early cartilage degeneration occurs, progression to severe grades of degeneration is not frequently observed.
- This phenomenon is thought to be caused by the unique anatomic, biomechanical, and cartilage characteristics of the ankle.
- Specifically, the ankle has a smaller contact area than the hip or knee in a load-bearing pattern and subsequently, the pressure distribution is different which explains the differences between joints.
- There is also a relatively higher cartilage resistance in the ankle, which might protect it from degenerative changes leading to primary OA.
- This higher cartilage resistance in the ankle is due to the fact that the ankle is primarily a rolling joint with congruent surfaces at high loads, which allows it to withstand large pressures.
- Although the ankle cartilage is thinner compared with knee or hip cartilage, it shows higher compressive stiffness and proteoglycan density, lower matrix degradation, and less response to catabolic stimulations.
- So the ankle is not generally a site of primary OA (This occurs only in approximately 7% of all ankle OA cases).
Secondary Osteoarthritis
- This last form can be caused by trauma, metabolic disease, congenital malformations, premature menopause, etc. Sometimes, it can happen that a patient is suffering from secondary osteoarthritis before the age of 40.
- In most cases, ankle OA is developed secondary to trauma such as fractures of the malleoli, the tibial plafond, the talus, maybe some varus alignment, and also potentially ankle ligament injuries.
- The mechanism of ligament injuries leading to OA may be twofold: either an acute osteochondral lesion which can occur in severe ankle sprains or chronic change in ankle mechanics leading to repetitive cartilage degeneration, as in recurrent or chronic unstable ankles.
- Due to the fact that this second mechanism is the leading cause of ankle OA, sufferers are usually younger than patients with primary OA.
Clinical features of Osteoarthritis Of Ankle
- As with osteoarthritis of any joint, there are subjective and objective patterns that match the symptoms of osteoarthritis you need to be aware of, below is a table with the most common signs.
- joint pain: Usually affects 1 to a few joints at a time Insidious onset, slow progression over time variable Intensity, Worse in weight-bearing, Relieved by rest initially, May have severe night pain
- Stiffness: Short-lived early morning stiffness (<30 mins), Short-lived inactivity-related stiffness
- Swelling: Some sufferers report swelling, mild effusion, and deformity.
- Swelling over bony and soft tissue surfaces
Diagnosis of Osteoarthritis Of the Ankle
- Clinical diagnosis made on the history of the patient, chief complaint of patient, observation, and palpation.
Observation, specifically looking at:
- Swelling/effusion of the ankle (and grade of this swelling)
- Active inflammatory process
- Gait
- Looking for muscular atrophy
- Expression of pain
- Joint deformity
2. Palpation:
- Feeling deep within the joint’s articular surfaces, searching for specific tenderness and reproduction of the patient’s symptoms
- Feeling for any crepitus in movement
- Feeling for the type of swelling/effusion
- Feel for temperature
- Any sensation loss in a dermatomal patter
3. Basic Objective Tools
- ROM active and passive, any limitations, feel for crepitus, where pain or stiffness onset, reproduction of symptoms
- Strength, any weakness in specific muscles or groups globally
- Functional tasks such as sit-to-stand, steps, squats, and quick changes of direction.
4. Special Tests
- Talar tilt to check for instability
- Anterior and posterior drawer to test for instability and arthrokinematics
- Balance and proprioception such as a single-leg stand
- Medical Management
- Potentially relapsing and intermittent
Medical Management of Osteoarthritis Of Ankle
- Depending on the type and the severity of OA, there are several medical and nonsurgical treatments:
- Anti-inflammatory medication to counter periodic inflammation.
- Intra-articular injection of corticosteroids, a drug that reduces inflammation.
- An injection of hyaluronic acid in the joint. This viscosupplementation refers to the concept of synovial fluid replacement with intra-articular injections of hyaluronic acid for the relief of pain, associated with OA.
Surgical Treatment
- There are also medical-surgical treatments. What surgical treatment is required depends on the location of OA, how severely the joint is affected, and the degree of experiencing the condition.
- Sometimes more than one type of surgical treatment is needed. The most common surgical procedures in ankle OA are:
- cleaning the joint with keyhole surgery: arthroscopy.
- securing the joint: arthrodesis.
- replacing of the joint: ankle prosthesis.
Physiotherapy management
ELECTROTHERAPY
pain-relieving modalities such
- SWD: Short Wave Diathermy is a deep heating modality that uses heat to provide pain relief, improves the blood supply to targeted muscles, and removal waste products.
- TENS: transcutaneous electrical nerve stimulation is an electrical modality that provides pain relief by providing pain modulation.
- TENS closes the gate mechanism at the anterior grey horn in the spinal cord. also stimulates the endogenous opioid system which prevents the release of substance p at the anterior grey horn.

- IFT: Interferential current therapy produces a low-frequency effect at targeted tissue, it inhibits transmission of pain impulses, stimulates the endogenous opioid system, increasess blood supply, relieves edema, and removes waste products.
- Cold therapy: used to relieve inflammation and reduce pain, Ice Massage- Ice on the area of inflammation for anti-inflammatory effects. Use ice in a paper or Styrofoam cup (peeled away) for 5-7 minutes, make sure to avoid frostbite.
EXERCISE THERAPY
- Exercise: is most effective when it consists of a combination of:
- Strength training: muscle strengthening exercises for Gastrocnemius, Soleus, Tibialis Anterior, and Peronei (repeated exercises with theraband).
- Endurance training: exercises to increase aerobic capacity. Run training and cycling are recommended.
- RANGE OF MOTION EXERCISES: range of motion exercises. Exercises including plantarflexion, dorsiflexion, inversion and eversion of the ankle are recommended.
- Balance and proprioceptive training if there is the instability of the ankle joint. Exercises (plantarflexion, dorsiflexion, inversion, and eversion of the ankle) with air cushion and wobble board are recommended.
- Functional exercises like standing on one leg, walking on various surfaces, sitting down and getting up, getting up from lying position, climbing stairs are also recommended because these exercises include several components simultaneously.

- Hydrotherapy: is recommended by international guidelines. It can be useful in cases where the pain is too severe to exercise on dry land.
- Some studies suggest that swimming and water exercises (including plantar flexion, dorsiflexion, inversion, and eversion of the ankle) are excellent for OA patients.
- It provides relaxation (in the case of a warm bath), decreased pain level, and improved mobility.
- Passive mobilization: this includes mobilizations for plantarflexion, dorsiflexion, inversion, and eversion of the ankle. It has proved to be effective in eliminating pain and joint immobility. It is only effective in combination with active exercise therapy.
- Massage: of the muscles around the ankle. This is not effective for ankle OA. However careful and progressive massage of a pain point can lead to a temporary waiver of localized pain