Osteochondritis Dissecans & Physiotherapy Management
- Osteochondritis dissecans is a joint condition in which bone underneath the cartilage of a joint dies due to lack of blood flow. This bone and cartilage can then break loose, causing pain and possibly hindering joint motion.
- Osteochondritis dissecans occurs most often in children and adolescents. It can cause symptoms either after an injury to a joint or after several months of activity, especially high-impact activity such as jumping and running, which affects the joint. The condition occurs most commonly in the knee but also occurs in elbows, ankles, and other joints.
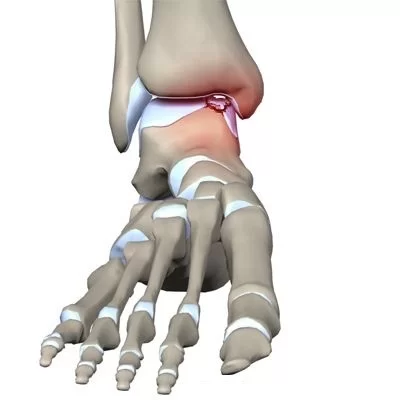
- Osteochondral lesions, sometimes called osteochondritis dessicans or osteochondral fractures, are injuries to the talus (the bottom bone of the ankle joint) that involve both the bone and the overlying cartilage. These injuries may include softening of the cartilage layers, cyst-like lesions within the bone below the cartilage, or fracture of the cartilage and bone layers. Throughout this article, these injuries will be referred to as osteochondral lesions of the talus (OLT).
Anatomy
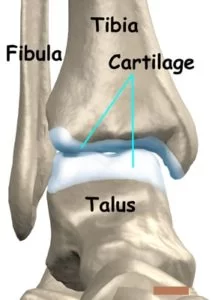
- Parts of the ankle The talus is the bottom bone of the ankle joint. Much of this bone is covered with cartilage. The tibia and fibula bones sit above and to the sides of the talus, forming the ankle joint.
- This joint permits much of them up (dorsiflexion) and down (plantarflexion) motion of the foot and ankle. The blood supply to the talus is not as rich as many other bones in the body, and as a result injuries to the talus sometimes are more difficult to heal than similar injuries in other bones.
Symptoms of Osteochondritis dissecans
- OLTs usually occurs after an injury to the ankle, either a single traumatic injury or as a result of repeated trauma. Common symptoms include prolonged pain, swelling, catching, and/or instability of the ankle joint.
- Symptoms can be vague. After an injury such as an ankle sprain, the initial pain and swelling should decrease with appropriate attention (rest, elevation).
- Persistent pain despite appropriate treatment after several months may raise concern for an OLT. Depending on the joint that’s affected, signs and symptoms of osteochondritis dissecans might include:
- Pain: Pain may be felt primarily at the lateral (outside) or medial (inside) point of the ankle joint. This most common symptom of osteochondritis dissecans might be triggered by physical activity — walking up stairs, climbing a hill, or playing sports.
- Swelling and tenderness.
- Joint popping or locking: joint might pop or stick in one position if a loose fragment gets caught between bones during movement.
- Joint weakness: might feel as though the joint is “giving way” or weakening.
- Decreased range of motion: might be unable to straighten the affected limb completely severe locking or catching symptoms, where the ankle freezes up and will not bend, may indicate that there is a large osteochondral lesion or even a loose piece of cartilage or free bone within the joint.
Causes of Osteochondritis dissecans
- The majority of OLTs, as many as 85 percent, occur after a traumatic injury to the ankle joint. Ankle sprains are a common cause of OLTs. With this type of injury, a section of the talus surface may impact another part of the ankle joint (tibia or fibula).
- As this happens, an impaction, crushing or shearing injury to the talus may occur. Some patients, however, have no history of an injury to their ankle.
Diagnosis of Osteochondritis dissecans
- OLTs are diagnosed with a combination of clinical and special studies. Your orthopedic foot and ankle surgeon may have a suspicion that you have this type of injury from the history you provide.
- A physical examination can further increase the suspicion for this type of injury. Imaging is necessary to confirm the diagnosis. Occasionally, regular X-rays can show an OLT but frequently additional imaging is needed. This additional imaging may be a CT scan or an MRI.
Treatments of Osteochondritis dissecans
- Once the diagnosis has been confirmed, treatment may be surgical or non-surgical, depending on the nature of the OLT, the presence of other injuries, and patient characteristics.
Non-surgical treatment
- Non-surgical treatment is appropriate for certain lesions and usually involves immobilization and restricted weight-bearing. This may be followed by a gradual progression of weight-bearing and physiotherapy. The goal of non-surgical treatment is to allow the injured cartilage and bone to heal.
- Patients may have an OLT that is present and doesn’t cause pain or limitations or a lesion that becomes painful but improves. In these cases, no additional treatment is necessary. It was once believed that all OLTs progress and worsen with time. This has been shown to no longer be true.
surgical management
- Other lesions may be more appropriately treated with surgery. The goals of surgery are to restore the normal shape and gliding surface of the talus in order to re-establish normal mechanics and joint forces. The hope is to minimize symptoms and limit the risk of developing arthritis.
- Depending on the characteristics and location of the OLT, surgery may be done arthroscopically or by opening the skin. Arthroscopy uses a camera and small instruments to view and work within the joint through small incisions.
- It may not be possible to properly treat certain lesions arthroscopically due to the size or location of the lesion.
- Treatments may include debridement (removing injured cartilage and bone), fixation of the injured fragment, microfracture or drilling of the lesion, bone grafting the bone cyst below the cartilage, and/or transfer or grafting of bone and cartilage.
- You and your foot and ankle orthopedic surgeon can discuss these treatment options and decide which one is best. Often, there may be several treatment options.
- If a patient has any underlying conditions that may predispose to an OLT such as ankle instability, ankle impingement, a high arched (cavovarus) foot, or tight calf muscles, it may be necessary to correct these problems at the time of surgery as well.
Physiotherapy management of Osteochondritis dissecans
- Physiotherapy management starts after the phase of immobilization or the surgical management of diseases. physiotherapy treatment should be avoided during the immobilization phase or in the acute phase of injury.
- The patient with Osteochondritis dissecans should be instructed to apply ice to the posterior heel and ankle in the acute period of pain. Icing can be performed several times a day, for 15-20 minutes each.
- TENS: transcutaneous electrical nerve stimulation is an electrical modality that provides pain relief by providing pain modulation.TENS closes the gate mechanism at the anterior grey horn in the spinal cord. also stimulates the endogenous opioid system which prevents the release of substance p at the anterior grey horn.

- IFT: Interferential current therapy produces a low-frequency effect at targeted tissue, it inhibits transmission of pain impulses, stimulates the endogenous opioid system, increases blood supply, relieves edema, and removes the waste products.
- Contrast bath therapy: Contrast bath therapy is a form of treatment where a limb or the entire body is immersed in hot (but not boiling) water followed by the immediate immersion of the limb or body in cold ice water. This procedure is repeated several times, alternating hot and cold. It relieves inflammation of bursae, swelling and reduce the pain.
- Immobilization: a short-leg cast or boot, it allows the tendon to heal, or avoid all weight-bearing.
- Medications: non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce pain and inflammation.
- After relieving in symptoms of Osteochondritis dissecans, graded exercise protocol should start with care.
Ankle joint Range of motion exercise
- Dorsiflexion
- Plantarflexion
- Eversion
- Inversion
- Gradual progressive stretching of the Achilles tendon can be performed in the following manner:
- Stand in front of a wall, with the affected foot flat on the floor. Lean forward toward the wall until a gentle stretching is felt within the ipsilateral Achilles tendon.
- Maintain the stretch for 20-60 seconds and then relax.
- Perform the stretches with the knee extended and then again with the knee flexed.
- To maximize the benefit of the stretching program, repeat the above steps for several stretches per set, several times daily. Avoid ballistically (ie, abrupt, jerking) stretches.
- Other treatment options are microcurrent therapy and corticosteroid injection into the retrocalcaneal bursa
Strengthening exercise :

- Start by sitting with your foot flat on the floor and pushing it outward against an immovable object such as a wall or heavy furniture. Hold for about 6 seconds, then relax. After you feel comfortable with this, try using rubber tubing looped around the outside of your feet for resistance.
- Push your foot out to the side against the tubing, then count to 10 as you slowly bring your foot back to the middle.
- While still sitting, put your feet together flat on the floor. Press your injured foot inward against your other foot. Hold for about 6 seconds, then relax.
- Next, place the heel of your other foot on top of the injured one. Push down with the top heel while trying to push up with your injured foot. Hold for about 6 seconds, then relax.
Weight-bearing exercise

- walk-on toe
- walk-on heel
- toe standing
- heel standing
Balance exercise :

- Stand on just your injured foot while holding your arms out to your sides with your eyes open. If you feel unsteady, stand in a doorway so you can put your hands on the door frame to help you. Balance for a long as you can, working up to 60 seconds. When you can do this for 60 seconds.
- Stand on your injured foot only and hold your arms across your chest with your eyes open. When you can do this for 60 seconds.
- Stand on your injured foot only, hold your arms out to the sides, and close your eyes. If you feel unsteady, stand in a doorway so you can put your hands on the door frame to help you. When you can do this for 60 seconds, try exercise number.
- Stand on your injured foot only, hold your arms across your chest, and close your eyes. Balance for as long as you can, working up to 60 seconds.
Proprioceptive training
- proprioceptive training on bosu
- proprioceptive training on wobble board
- proprioceptive training in the balance board





3 Comments