Psoriatic Arthritis
What is Psoriatic Arthritis?
Psoriatic arthritis can cause aches, swelling, stiffness, or immobility in and surrounding your joints. It usually affects 3 in ten people who already have the skin disease psoriasis. Psoriasis causes patches of red color and friable skin which is coated with silvery-like patches.
Numerous people may develop psoriatic arthritis before psoriasis is even present. In irregular cases, humans have psoriatic arthritis and never have any evident patches of psoriasis. Psoriatic arthritis and psoriasis are both autoimmune diseases, caused by a defect in the immune system.
Our immune system defends us from sickness and infection. But in autoimmune diseases, the immune system evolves confused and attacks normal parts of the body, frequently causing inflammation. Psoriatic arthritis is a variety of spondyloarthritis. This is a group of diseases with similar symptoms.
Types of Psoriatic Arthritis
There are 5 types of PsA.
Symmetric PsA
This type involves the same joints on both sides of your body, so both your left and right knee joints, for example. Signs can be like those of rheumatoid arthritis (RA) Symmetric PsA grows to be milder and generates less joint deformity than RA. But symmetric Psoriatic Arthritis PsA can be disabling. About half of the humans with PsA have this type of arthritis.
Asymmetric PsA
This involves a joint or joint on one side of your body. Your joints may sense soreness and turn red in color. Asymmetric PsA is typically mild. It involves about 35 percent of humans with PsA.
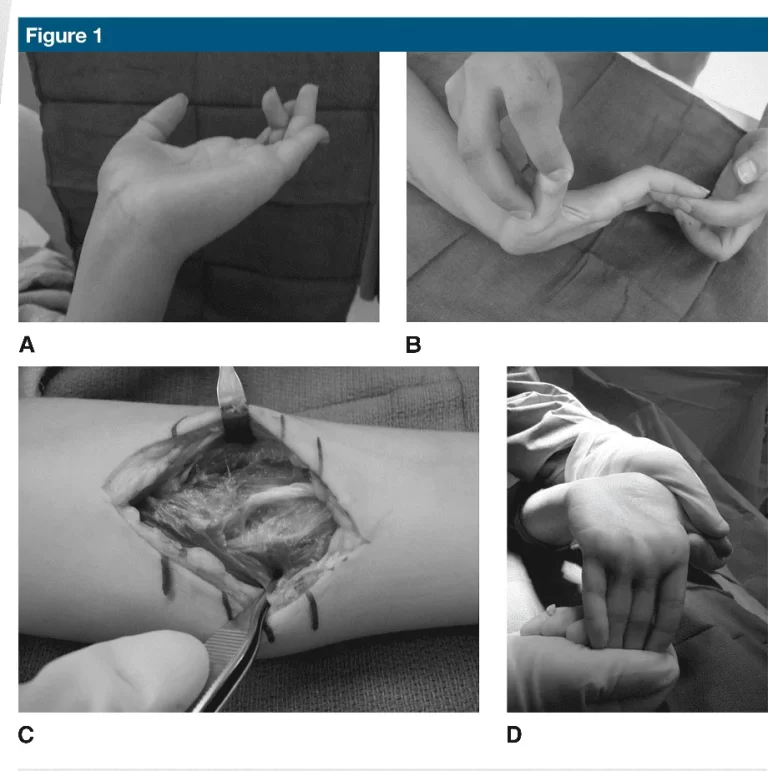
Distal interphalangeal predominant PsA
This type affects the joints nearest to your nails. These are called distal joints.
Spondylitis PsA
This type of PsA affects your spine. Your whole spine from your neck to your lower back may be involved. This can make motion very acheful. Your arms, hands, legs, feet, and hips may also be involved.
Psoriatic arthritis mutilans
This is an intense, deforming type of Psoriatic Arthritis PsA. About 5 percent of humans with PsA have this type of arthritis. Psoriatic arthritis mutilans usually involve your hands and feet. It can also generate aches in your neck and lower back.
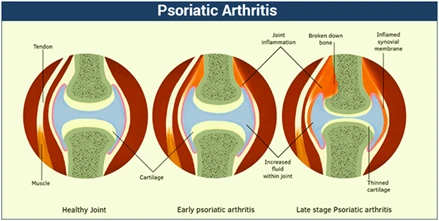
Psoriatic arthritis stages
PsA doesn’t follow the same way for each human diagnosed with this disease. Numerous people may only ever have gentle symptoms and limited effects on their joints. For others, joint malformation and bone growth may ultimately occur. It’s unclear why numerous people experience a more rapid progression of the disease and others don’t. But early diagnosis and treatment can assist to ease the ache and slow the harm to joints. It’s necessary you talk with your physician as soon as you start experiencing signs or symptoms that hint at PsA.
Early stage PsA
In the initial stages of this arthritis, you may feel mild symptoms such as joint swelling and a decreased range of movement. These symptoms may appear at the same time you develop psoriasis skin area, or they may appear years later. NSAIDs are the typical management. These drugs ease aches and symptoms, but they don’t slow Psoriatic Arthritis PsA.
Moderate PsA
Depending on the variety of PsA you have, the moderate or middle phase will likely see aggravating symptoms that need more progressive treatments, such as DMARDs and biologics. These drugs can assist ease symptoms. They may assist to slow the progression of harm as well.
Late-stage PsA
At this point, bone tissue is heavily involved. Joint malformation and bone growth are likely. The treatment goal is to ease symptoms and control worsening complications.
Prevalence
- Appears in 6%-42% of humans that have psoriasis
- Roughly 2% of the local population has psoriasis
- Psoriatic arthritis is calculated to have a majority of 0.1%-0.25%
- Equal prevalence in both men and women
- Can occur at any age but generally occurs between the ages of 30-fifty years old
- 80-90% probability of having psoriatic arthritis PSA if one of your first-degree relatives has the conditions
What are the symptoms of psoriatic arthritis?
The symptoms of psoriatic arthritis involve:
- Swollen toes and fingers
- Foot ache
- Lower backache
- Fatigue
- Swelling and ache surrounding your tendons
- Stiffness and tiredness in the morning
- Decrease range of motion
- Nail changes
- Eye red in color and ache
- Scaly skin, Particularly on your knees, elbows, and scalp area
Psoriatic arthritis can cause several various symptoms surrounding the body. Humans will often have 2 or more of these symptoms, and they can criteria from mild to severe.
Some of the main symptoms involve:
joint ache
- swelling in 1 or more joints
- joint stiffness – which senses worse when you get up after a nap and lasts longer than thirty minutes.
These symptoms are generated by inflammation inside a joint. This is called inflammatory arthritis. - Psoriatic arthritis can generate aches and swell along the bones that form the joints. This is induced by inflammation in the connective tissue, called entheses, which connect tendons and ligaments to the bones. When they evolve inflamed it’s called enthesitis.
- Enthesitis ache can spread over a broad area instead of just inside a joint. Harmed areas can sense tenderness if you touch them or if there’s just a small quantity of pressure on them. It generally occurs in the feet. This can occur at the back of the heel or on the base of the foot near the heel. In a few cases, this ache can make standing or walking harder.
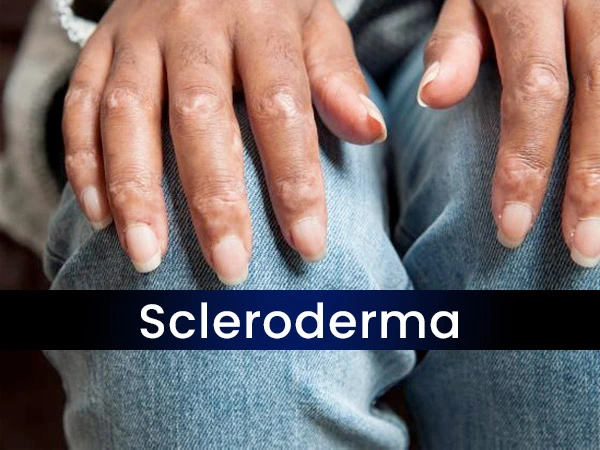
- The knee joints, hip joints, elbows, and chest can also be involved by enthesitis. Patients with psoriatic arthritis can have swollen fingers and toes. This is called dactylitis, or sausage digit because it generates the full finger or toe to bulge up. It most generally involves one or two fingers or toes at a time.
- Psoriatic arthritis can also generate little circle-shaped dents in fingernails and toenails, which is called pitting. The nails can also change color, evolve thicker, and may lift far from your finger.
- It can also cause weakness, which is severe and continuous tiredness that doesn’t get well with rest.
Psoriatic Arthritis Causes
Physicians aren’t sure what causes psoriatic arthritis, but these things may play a function:
- Genes. Having a parent with psoriasis triples your probability of getting psoriasis and makes it more possible to have psoriatic arthritis.
- Infection. An infection that sets off your protective system could be to blame. Psoriasis, for example, is frequently triggered by strep throat.
The genes you inherit from your parents and grandparents can make it more possible to evolve psoriatic arthritis. If you have genes that put you at risk of this disease, the following may then aggravate it:
- an infection
- an accident or trauma
- being overweight
- smoking.
- There is also an element of chance, and it might not be possible to say for certain what caused your disease.
Psoriasis and psoriatic arthritis are not infectious, so humans can’t catch them from one another.
Psoriatic Arthritis Risk Factors
- Psoriasis. Up to 30% of humans with psoriasis obtain psoriatic arthritis. It involves men and women in the same.
- Age. You can get Psoriatic Arthritis PsA at any age, but it generally affects humans between 30 and 50.
- Family history. As many as 40% of humans with psoriatic arthritis have a family history of skin or joint disorder.
Complications
Having psoriatic arthritis can put you at risk of evolving other diseases and complications around the body.
The probability of getting one of these is occasional. But it’s worth knowing about them and talking to your physician if you have any problems.
Eyes
Seek urgent medical alert if one or both of your eyes are red in color and acheful, specifically if you have a difference in your vision. You could go to your Physician, an eye clinic, or your general eye department.
These symptoms could be caused by a problem called uveitis, which can cause inflammation in the central layer of the eye.
Uveitis can permanently harm your eyesight if left untreated.
Other symptoms are involved:
- blurred or cloudy vision
- sensitivity to light
- not being capable to see things at the side of your field of vision – called a loss of peripheral sight
- small shapes proceeding across your field of vision.
- These symptoms can arrive suddenly, or slowly over a few days. It can involve one or both eyes. It can be managed effectively with steroids.
Heart
Psoriatic arthritis can put you at a slightly higher risk of having a heart disorder. You can decrease your risk by:
- Do not smoke
- Maintaining a healthy weight
- exercising daily
- Consuming a healthy diet, that’s low in sugar, fat, and salt
- Do not drink too much alcohol.
- These positive lifestyle options can assist to improve your arthritis and skin symptoms.
- Talk to your physician if you have any problems with your heart health.
Digestive System
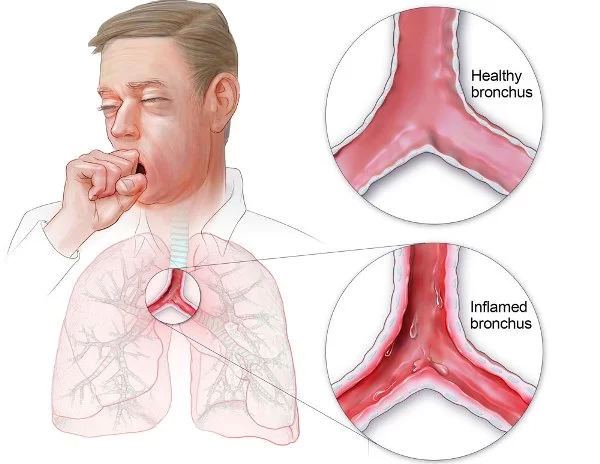
You have an increased risk of evolving Crohn’s disorder if you have psoriatic arthritis. Crohn’s disease is a disease in which parts of the digestive system evolve inflamed.
See a physician if you have any of these symptoms, specifically if you have two or more and they don’t go far:
- blood
- diarrhea for more than 7 days
- daily pain or aches, or cramps in your stomach
- fevers
- a general feeling of being sick
- unexplained weight loss.
Liver
Non-alcoholic fatty liver disease -NAFLD is a term used to define some diseases where there is a build-up of fat in the liver. This doesn’t cause problems in the early phases. But it can show to cirrhosis, which is when the liver starts scarred and may stop working appropriately.
See a doctor if you have the following:
- excessive tiredness
- the ache in the top right of the stomach, which can be dull or aching
- unexplained weight loss
- yellowing color of the skin and eyes, which is called jaundice
- itchy skin
- swelling in the ankles, legs, feet, or tummy.
How is psoriatic arthritis diagnosed?
Psoriatic arthritis is easier to verify if you already have a psoriasis condition. If you don’t have skin symptoms or signs, diagnosis is harder. The procedure starts with a health history and a physical examination. Your healthcare provider or doctor will ask about your symptoms and signs. You may have blood tests to inspect the following:
- Erythrocyte sedimentation rate (ESR or sed rate). This test examines how fastly red blood cells or RBCs fall to the base of a test tube. When swelling and inflammation in the body are present, the blood’s proteins clump jointly and get heavier than normal. They fall and settle rapidly at the base of the test tube. The more rapidly the blood cells fall, the more intense the inflammation.
- Uric acid. High blood uric acid amounts can be found in psoriatic arthritis but are not operated on for diagnosis or monitoring.
- Imaging. X-rays, CT scans, ultrasound, MRI, and skin biopsies may all be utilized to support the diagnosis.
- Rheumatoid factor (RF). Your protective system generates this autoantibody. It’s generally present in Rheumatoid Arthritis RA but negative in PsA. An RF blood test can assist your physician to tell whether you have PsA or RA.
- Joint fluid. An arthrocentesis releases a small quantity of liquid from your knee joints or another joint. If uric acid crystals are in the fluid, you might have gout rather than PsA. A culture fluid examination can rule out infection or sepsis.
Psoriatic Arthritis Treatment
Medication
Medical treatments for psoriatic arthritis involve:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). These are over-the-counter drugs such as ibuprofen and naproxen.
- Disease-modifying antirheumatic drugs (DMARDs). These can slow or stop the ache, swelling, and joint and tissue harm. If NSAIDs don’t work, your physician will try DMARDs. They may bring longer to work.
- Immunosuppressants. If you can’t eat a DMARD, you might get a variety of drugs known as an immunosuppressant. These medicines curb your protective system, which is what’s causing the condition in an autoimmune condition such as PSA. But they can also create it more probable that you’ll get an infection.
- UV light. Therapy with UVA light can reduce skin symptoms in people who have extreme psoriasis. But it may also increase your chances of skin cancer.
- Biologics. If protective suppression doesn’t work, your physician may prescribe a biologic. These are newer varieties of DMARD. Instead, than weaken your entire protective system, these drugs block a protein that leads to inflammation.
- Enzyme inhibitor. This works by restricting a certain enzyme, a type of protein, known as PDE-4. That assist to slow other responses that lead to inflammation.
- Steroids. These can assist in stabilizing inflammation, but physicians don’t use them frequently for PsA because they can make your skin rash more harmful. Physicians prescribe steroids only when you really require them. If you use these drugs for a long time, you could have dangerous side effects such as flaky bones, increase weight, hypertension, and diabetes.
- Surgery. A severely harmed joint can be replaced with a new one constructed from metal and plastic.
Physiotherapy Treatment
In general, low-impact exercises are best for humans with arthritis. Here are some concepts to get you proceeding while living with psoriatic arthritis.
Walking
Walking is a tried and true low-impact exercise for patients. Begin with a few minutes per day and try to walk on flat ground to decrease the pressure on your joints.
If arthritis involves your feet, make sure you wear shoes that include:
- fit properly
- offer good assistance
- don’t pinch your toes
- You can also get specific insoles for added protection.
Work up to a thirty-minute walk each day or add short walks in whenever you can.
To add walking into your regular routine:
- Select the farthest parking space and walk the additional distance.
- Get up and walk surrounding your home or property several times a day.
- Take a long route and add in a few more steps whenever possible.
- Walk surrounding the block or use a treadmill.
- As you walk, pay alert to how you move your joints or junctions and how you’re sensing. If you feel sore, it may be best to try various exercises and return to walking tomorrow.
Weight training
Strong muscles help to assist your joints, and weight training can help to maintain your muscles strong and healthy.
Resistance training improved function and quality of life while decreasing symptoms in humans with PsA.
The goal for strengthening exercises a pair of times per week or every other day. You’ll want to give your muscles some rest between workout days if necessary.
Examples of weight training that’s beneficial for psoriatic arthritis involve:
- holding a five-pound weight straight out from your body at arm’s length
- pushups
- squats and lunges
- Pilates
- Back off from strength training for a few days if you develop swelling or aches. Check with your physician before continuing if it continues to cause a problem.
If you’re currently feeling aches from arthritis, use isometric exercises to build up your muscles by tensing them without moving your joints.
Nevertheless of whether you have arthritis, aerobic exercise is better for your heart. It enhances general health and increases energy levels.
Aerobic exercise also helps with weight control, which, in turn, assists to decrease pressure on joints and decrease inflammation.
There are lots of fun ways to get aerobic exercise, like:
- brisk walking
- biking
- dancing
- swimming
- using an elliptical machine
- water aerobics
- tai chi
- using a rowing machine
- If you haven’t been active recently, begin slowly. Slowly raise your speed and workout time until you’re exercising for about 20 to 30 minutes, three times a week.
If your joints can’t take that length of time, break it up into ten-minute segments throughout the day.

Swimming
Another fun method to get some exercise is to hit the pool.
Swimming exercises some of your joints or junctions and gives aerobic activity. Water assists your hardworking joints while giving resistance to work against. Also, a heated pool can assist to decrease joint aches and muscle stiffness.
Remember to make gentle motions as you exercise and stop if you feel an ache.
Examples of exercises you can do in the water involve:
A forward arm reaches. Lift one or both arms upward as up as you can, starting with your arms immersed in the water.
Arm circles. Create circles with your arms underwater.
Leg swings. Holding the pool fence for balance if required, hang your leg up in front of you and then back behind you.
Chlorine in pools can cause skin dryness, so you may want to take a shower and use moisturizing cream after swimming.
Other exercises for psoriatic arthritis patients:
Complementary therapies like yoga and tai chi assist in enhancing stress relief. Slow, gentle motions can enhance balance and coordination.
The concentration and deep breathing techniques associated with yoga can assist to decrease stress. These practices frequently take place in a group environment, which can also keep you motivated.
Other complementary practices like acupuncture and meditation may give benefits, too.
Acupuncture can enhance the quality of life in patients with rheumatoid arthritis. Meditation may also assist in decreasing stress and enhancing relaxation.
Ice packs
You can buy specific ice packs from a chemist or they can be created from a packet of frozen peas covered in a wet towel. If you use frozen peas memorize to mark them as not to be eaten as they will have defrosted and refrozen if you use the same package every time which could lead to food poisoning. Ice packs can assist to decrease the heat and swelling in an inflamed joint. Apply for about 10 minutes every 2 hours. If you have bed circulation, check with your physician first. Don’t apply ice straight to the skin.
massaging
Rubbing or massaging an area of swelling can assist in enhancing circulation. Ask your physician about the use of anti-inflammatory gels available at medical stores.
Splints
Splints to help acheful joints can be supplied by a doctor, Physician, physiotherapist, or occupational therapist. All splints should be prescribed and fitted by a health professional or doctor, who will give you suggestions on when and how long to wear them.
Heat and cold therapy
Heat therapy and cold therapy may also be useful to relieve aches and stiffness. The simplest layouts are a hot water bottle, a hot bath or shower, or microwave heat packs. These can be useful to decrease morning stiffness. Do not purchase wax baths except at the suggestion of a doctor or physiotherapist. Intermittent heat and cold therapy include choosing or switching the use of moist heat and cold therapy on harmed joints. Moist heat – provided by a hot pack, a warm towel, or a warm bath or shower – assist to relax aching muscles and decrease joint pain, swelling, and soreness. Cold therapy – provided by a bag of ice or even a bag of frozen vegetables wrapped in a towel – can decrease swelling and relieve pain by numbing the involved joints.
Transcutaneous electrical nerve stimulation (TENS)
TENS machine provides low voltage, intermittent currents to acheful areas and has been shown to help to control pain very appropriately. The machines are affordable and can be bought or hired. Your doctor or physiotherapist can give you more suggestions.
What to avoid?
Exercise is important for a healthy lifestyle, but it’s important not to exaggerate it, specifically when you have psoriatic arthritis. Certain exercises and a variety of equipment are also advised over others.
High-impact
In general, it’s good to stick to low-impact exercises that are easier on your joint junctions. This is especially important if Psoriatic Arthritis PsA affects your spine.
Still, some recent advancement suggests that higher-impact exercises may also be good for people with PsA.
Small interactions in high-intensity interval training for a few months did not worsen disease activity in patients with PsA and even decreased fatigue.
To help avoid trauma, talk with your doctor, physicians, or physical therapist first if you want to try higher-impact exercises.
Free-weight workouts that hurt your hands
Free weights are good for doing strength training at home but make sure you’re using the right instrument.
It helps to find weights with a rubber grip or band since they’re easier to hold. You can use weights that strap to your ankles or wrists, too.
You may also have a more comfortable time with a set of nonadjustable weights. Adding or subtracting weight from a dumbbell can be hard if arthritis involves in your hands.
Be sure to understand and use the correct form to help prevent trauma, particularly when using free weights.
If the exercise is acheful or you can’t find a suitable instrument, it may be good to use weight machines. These tend to be simpler to use and may assist you to avoid trauma.
Range of motion exercises that hurt
Range of movement exercises is important for maintaining and increasing joint motions and decreasing stiffness.
Try to do these exercises every day to assist in enhancing flexibility. You want to sense a stretch without forcing the movement or pushing through any ache.
When your joints or junctions are swollen or in ache, do your best to achieve as much range of movement as you can without increasing your ache.
Overexerting yourself
Whatever your activity of selection is, there may be times when you’re just not up to it. Remember to listen to your body and take days off and take rest. Forcing inflamed joints into action may result in joint injured.
You can still exercise areas of the body that aren’t sensing soreness. For example, if your hands need a break completely, try walking or exercising in the pool and doing something. You can still exercise your arms and shoulders if your toes feel unwell.
An ice pack can help to decrease joint swelling. Some tips involve:
- Apply one for ten minutes every pair of hours but don’t put ice straight on your skin.
- Use an ice pack covered in a towel.
- You can try alternating between putting cold and heat but wait for a pair of hours between each one.
- If you find that icing makes arthritis aggravate, ask your doctor or physician for other suggestions.
Ache during or after exercise means that you’re pushing too extreme. Exercise should never cause aches.
Take it easier next time while you work up to a more severe workout. Some exercise can cause few soreness, however, which should go far in under forty-eight hours.
Muscle soreness will be most prominent when you first start a new variety of exercises. While it will reduce as time goes on, some soreness when exercising is normal.
Surgery
Most patients with psoriatic arthritis will never be necessary surgery. However, severely harmed joints may require joint or junction replacement surgery. The aim of surgery is to restore function or movement, relieve aches, increase movement, or enhance the physical appearance of the involved area.
Differential Diagnosis
- Osteoarthritis-OA
- Rheumatoid Arthritis-RA
- Reactive Arthritis
- Gout
- Lupus
- Mallet finger due to traumatic injury
- Ankylosing spondylitis
- Fibromyalgia
Lifestyle changes and home remedies
Some things you do on your own can decrease psoriatic arthritis symptoms:
- Keep a healthy weight. Carrying additional pounds puts more stress on your joints or junctions. It may also affect how well your drugs work.
- Stop smoking. This is 1 of the best things you can do for your general health.
- Limit alcohol. It can also affect how your management work.
- Exercise. It’s a great path to protect your joints or junctions and keep your weight in check. Stronger muscles can also assist your joints. Low-impact exercises such as swimming or walking are easier on them. Ask your doctor or physician about an exercise plan.
- Try physical or occupational therapy. Your doctor might suggest that you see a specialist who can assist you learn to manage your symptoms. This can include exercises, body alignment, hot therapy, cold therapy, and tips for changing the path you do certain things. A physical therapist or occupational therapist can also assist you to pick assistive instruments such as braces or splints to support your joints.
- Use acupuncture or massage therapy. These treatments are natural ways to relieve pain and stiffness.
Psoriatic arthritis diet
- While no single food or diet will cure Psoriatic Arthritis PsA, a nutrient-dense and balanced diet can assist to decrease inflammation and relieving symptoms.
- Helpful correction to your diet can pay off tremendously for your joints or junctions and body in the long run.
- In short, eat more fresh fruits and fresh vegetables. They assist to decrease inflammation and manage your weight.
- Excess weight puts more stress on joints or junctions that are already sore.
- Limited eating of sugar and fat, which are inflammatory.
- Put an emphasis on things of healthy fats, such as fish, seeds, and nuts.
Psoriatic Arthritis Flare Triggers
Certain things could trigger psoriatic arthritis, involving:
- Not taking your drugs
- A skin lesion, such as a scrape or sunburn
- Infection
- Lack of sleep
- Stress
- Extra weight
- dry skin
- cold, dry weather
- smoking
- heavy drinking
FAQ
Which parts of the body are affected by psoriatic arthritis?
Psoriatic arthritis can be seen in any part of the body. However, the knees, fingers, toes, and spine are generally involved. Psoriatic arthritis can also cause aches in areas where ligaments and tendons connect to the bone, like at the heel or around the elbows. Arthritis can shift to various locations in the body over time.
Who is most likely to develop the disease?
Individuals with psoriasis can get psoriatic arthritis. In fact, up to thirty percent of males and females with psoriasis are estimated to have the disease. Psoriatic arthritis generally first appears between ages 30 and fifty but can start at any time. In a few cases, arthritis develops before the skin disease occurs. Those who have family members with psoriatic arthritis are also more likely to occur this disease.
Why is it important to seek treatment?
In extra to controlling symptoms, certain drugs can actually slow or protect the disease from injuring the joints. This can markedly increase the quality of life. Postponing management can result in preventable joint or junction pain and disability.
What type of doctor or physician should I see for treatment?
Whenever possible, work with a rheumatologist doctor, who can assist to evolve a treatment plan that’s effective for your problems and needs. A rheumatologist is a doctor who has specific training and experience in arthritis and other joint disorder.
Why do you suggest Homeopathy for PA?
PA is a deep-seated auto-immune disease, which requires management at a deeper level. Conventional management alone is not enough, in most patients, it causes immunosuppression which is not the most desired path to treat PA, immune correction seems to be the right path, Homeopathy just does this for patients.


13 Comments