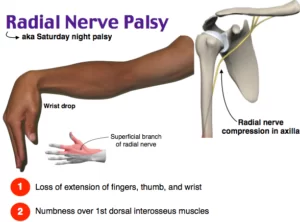
RADIAL NERVE INJURY(PARALYSIS)
RADIAL NERVE INJURY(PARALYSIS)
Introduction of Radial Nerve Injury
- Radial nerve paralysis, which can result from a complex humerus fracture, direct nerve trauma, compressive neuropathies, neuritis, or (rarely) malignant tumor formation, has been reported throughout the literature, with some controversy regarding its diagnosis and management.
- The appropriate management of any radial nerve palsy depends primarily on an accurate determination of its cause, severity, duration, and level of involvement. The radial nerve can be injured as proximally as the brachial plexus or as distally as the posterior interosseous or radial sensory nerve.
- The radial nerve is the most frequently injured major nerve in the upper extremity.1 Radial nerve paralysis generally can be divided into either open or closed injuries.
- All open injuries require exploration, whereas most closed injuries can usually be observed. The most common associated cause of radial nerve injury is a fracture to the shaft of the humerus. Iatrogenic injuries to the radial nerve may occur during complex and routine procedures of the upper extremity.
- Acute trauma from lacerations, missiles, injections, or traction can also result in radial nerve paralysis. Chronic or acute radial nerve compression can initiate a wide range of clinical symptoms, from weakness in wrist extension to complete radial nerve paralysis.
- Rarely, a neuritis or tumor of the radial nerve at levels as high as the brachial plexus will present with radial nerve palsy. Treatment options for radial nerve paralysis are dependent upon the primary cause and level of injury.
- A radial nerve paralysis without an associated laceration or penetration is considered“closed.”Fractures of the humerus may result in a closed radial nerve injury that is typically observed for a period of 3 months before surgical exploration.
- Idiopathic causes of radial nerve paralysis can be treated conservatively after treatable causes such as tumors have been excluded. The surgical options for open radial nerve injuries that result in a loss of nerve continuity include primary repair, nerve grafts, or tendon transfers.
- Recently, nerve transfer has been reported as a potential alternative to tendon transfer after the complete loss of radial nerve function or a significant delay in treatment.
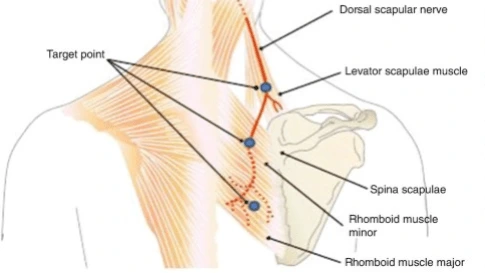
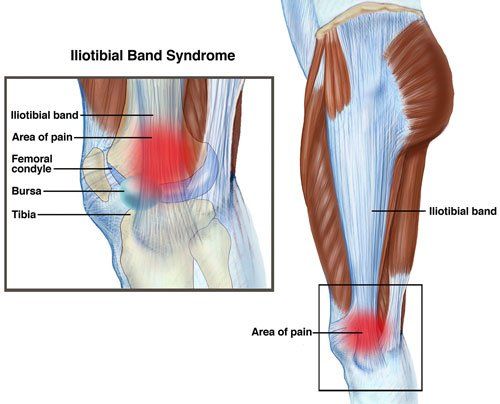
Anatomy Radial Nerve
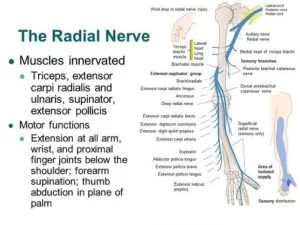
- The radial nerve is 1 of 2 terminal branches of the posterior cord of the brachial plexus with contributions
from C5, C6, C7, C8, and T1, traveling dorsal to the axillary artery and vein and closely abutting the shaft of the humerus near the spiral groove. - The nerve travels laterally deep to the long head of the triceps muscle and lies between the lateral and the medial heads of the triceps at the spiral groove, The radial nerve innervates the triceps before piercing the lateral intermuscular septum and entering the anterior compartment.
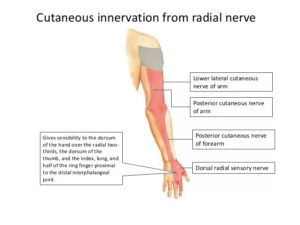
- The radial nerve gives off branches to the extensor carpi radialis longus and brachioradialis as it enters the antebrachial fossa between the biceps and brachialis medially and the brachioradialis laterally. As it passes over the elbow joint, it divides into a terminal motor and sensory branch at the level of the radiocapitellar joint, but the exact site may vary by as much as 5 cm. The motor branch is the posterior interosseous (or deep radial) nerve, and the sensory branch is the superficial radial nerve.
- The superficial branch of the radial nerve runs into the forearm under the brachioradialis before innervating the radial aspects of the dorsal wrist and hand. The posterior interosseous nerve travels a short distance over the radiohumeral joint, passing dorsolaterally around the radial head before entering the substance of the supinator. The nerve then winds around the neck of the radius to travel on the dorsal surface of the interosseous membrane.
- The posterior interosseous nerve supplies the majority of forearm and hand extensors (including the extensor carpi radialis brevis, supinator, extensor digitorum communis, extensor digiti quinti, extensor carpi ulnaris, abductor pollicis longus, extensor pollicis longus and brevis, and extensor indicis proprius), with the exception of the extensor carpi radialis longus and brachioradialis. The normal course of the posterior interosseous nerve is through the supinator brevis muscle.
MOTOR BRANCHES OF THE RADIAL NERVE:
- Arm:
- Triceps (Three Heads)
- Anconeus
- Elbow:
- Brachioradialus
- Long head of extensor carpi radialus
- Supinator
- Posterior interosseus nerve:
- Extensor Carpi Radialus (Short head)
- Extensro Digitorum Cmmunis
- Abductor Pollicis Longus
- Extensor Indicis Proprius
- Extensor Pollicis Longus
- Extensor Pollicis Brevis
Pathogenesis
- Radial nerve paralysis may not always have a clear origin. The radial nerve may be paralyzed at any point along its course from the brachial plexus to the hand, resulting in a similar clinical presentation regardless of the cause.
- Determining the level of injury often assists the physician in identifying the origin of the disorder. Several distinct causes of radial nerve paralysis have been clearly identified in the literature.
- A review of these potential causes will assist the physician in determining the most appropriate surgical option.
Causes
- Orthopedic injury:
- The radial nerve is injured through orthopedic trauma more than any other major nerve. Approximately 12 percent of humeral shaft fractures are complicated by a radial nerve paralysis.
- Spontaneous recovery within 8 to 16 weeks has been reported in over 70 percent of the cases.
- Rarely, the radial nerve can become entrapped in the bony fragments or callous after humeral fractures. In particular, spiral fractures of the distal shaft of the humerus with radial angulation have been associated with
radial nerve paralysis. - Radial nerve paralysis associated with dislocation of the radial head is believed to result mfrom traction on the nerve within the substance of the supinator, but the paralysis is usually transient.
- Tumor and inflammation:
- Radial nerve compression can occur as the result of either a benign tumor or a malignancy. The radial nerve is more susceptible to external compression near bones or joints where ganglions can form. Benign tumors arising from the elbow or at the upper end of the radius have been reported to cause posterior interosseous nerve paralysis. Lipomas are the most common tumors reported in the literature to cause radial nerve palsy.
- Radial nerve palsy may also result from nerve tumors. Peripheral nerve tumors can be classified into neoplasms of the nerve sheath, neoplasms nerve cell origin, metastatic tumors, neoplasms of nonneural origin, and neuromas.
- Unless they are associated with significant compression, benign nerve tumors such as schwannomas, neurofibromas, or intraneural lipomas rarely result in complete nerve paralysis. Nerve tumors that do result in paralysis should be fully evaluated because, although rare, they are more likely to be malignant (as with malignant schwannomas or nerve sheath fibrosarcomas). An unusual benign surgical entity of the nerve also worth noting is hypertrophic neuropathy (or “onion whorl disease”), which is characterized as a localized enlargement of the nerve resulting in the progressive loss of nerve function.
- Anatomic compression:
- Nontraumatic radial nerve palsy is rare compared with paralysis resulting from orthopedic
trauma. The cause of spontaneous paralysis of the posterior interosseous nerve or the radial nerve is often unknown. - Nevertheless, acute nerve paralysis requires investigation to rule out treatable causes of the disease such as neuritis, tumors, or compression. Neuritis, for example, is usually associated with several weeks of severe pain.
- The radial nerve can be compressed at multiple points along its course. At the elbow, for example, it can be compressed by the fibrous bands proximal to the radial tunnel, the vascular leash of Henry (the radial recurrent artery), the tendinous margin of the extensor carpi radialis brevis, and the arcade of Frohse (the
tendinous superficial head of the supinator). - Open wounds:
- The radial nerve is seldom divided in traumatic lacerations because of the deep position of the motor component of the nerve.
- Nevertheless, penetrating wounds associated with radial nerve palsy require surgical exploration to rule out axonotmesis.
- When the radial nerve is sharply divided, the clinical results after primary repair have been good to fair in most instances, if the nerve is explored early and repaired without tension. It is of particular interest that the radial nerve has been found to be transected in up to 50 percent of patients following gunshot wounds associated with humeral fractures.
- The treatment of postoperative radial nerve palsy requires a great deal of consideration. To identify nerve injuries in advance and to avoid any questions of origin after surgery, it is important to do a complete upper extremity nerve exam before any invasive procedure is performed in proximity to major nerves. The radial nerve can be injured inadvertently during orthopedic or vascular access procedures.
- A previous surgical scar or an exploration of the arm without the aid of am tourniquet often prevents a clear identification of nerves during dissections. Radial nerve paralysis may occur as the result of a traction injury or compressive neuropraxia after surgery. A thorough and honest reflection by the surgeon is required when radial nerve paralysis is noted after surgery. If there is any chance that the nerve may have been severed or partially transected, immediate re-exploration is indicated to ensure the best clinical outcome.
- Other causes:
- Radial nerve paralysis has been reported in association with the use of a tourniquet or with injection injuries.
- The radial and sciatic nerves are those most commonly injured by injections. The high percentage of injuries to these nerves can be attributed to their proximity to common intramuscular injection sites.
- Tourniquets are used routinely in the operating room to provide a bloodless field, and nerve paralysis after tourniquet use is 2.5 times more common in the upper extremity than in the lower extremity. Upper extremity nerve paralysis is estimated to occur in one out of 13,000 applications. The radial nerve is the nerve most susceptible to tourniquet trauma, with its involvement present to some extent in up to 96 percent of upper extremity tourniquet injuries.
- Postoperative radial nerve palsies can also be related to patient positioning or to blood pressure cuffs. Radial nerve paralysis may develop during sleep, especially when the patient is intoxicated, such as in a “Saturday night palsy.”
- Traction injuries after motor vehicle accidents or other blunt traumas may result in prolonged paralysis
of the radial nerve. Most of these nerve lesions can be treated conservatively if they are “closed” and if axonotmesis is not suspected. Patients who develop a spontaneous neuropathy may also have a susceptibility to other compressive neuropathies (i.e., hereditary neuropathy).
Classification of Radial Nerve Palsy
- Open versus closed: Injury is distinguished as either penetrating or nonpenetrating.
- High: Injury occurs above the distal insertion of the pectoralis major.
- Intermediate: Injury occurs between the insertion of the pectoralis major and the posterior interosseous nerve.
- Low: Injury involves the posterior interosseous or radial sensory nerve.
- Compressive: Injury involves chronic or acute anatomic compression.
- Delayed presentation: Injury involves a delay in presentation that significantly limits the available treatment options.
Symptoms of Radial Nerve Injury

- The hallmark of a radial nerve injury is wrist drop. Flexor tone overpowers the nonfunctional wrist extensors, and the hand is pulled into a flexed position. The wrist may be passively placed into extension, but the patient is unable to hold this posture, and the hand cannot be maintained in a functional position.
- In addition, extension of the fingers and thumb is lost, robbing the patient of the ability to open the hand prior to initiating grasp, and thereby rendering tasks requiring coordinated manual dexterity extremely difficult. If the lesion is distal to the origin of the PIN, ECRL function will be intact and the wrist will be pulled into radial deviation with attempts at extension.
Treatment of Radial Nerve Injury
- An algorithm for the treatment of radial nerve palsy was developed to determine the need for surgical reconstruction based on a concise and clinically relevant classification system. The first step in determining treatment is to classify the lesion as either open or closed.
- All radial nerve palsies associated with open wounds should be explored surgically. If the nerve is found to be in continuity at the time of the exploration, it is treated as a closed injury. If the radial nerve has been sharply transected, but there is adequate nerve length and minimal soft-tissue injury, then it should be repaired primarily.
- A primary nerve repair should be performed without tension by mobilizing the nerve both proximally and distally.
- Neurorrhaphy and Nerve Grafting: The radial nerve is the most suitable for neurorrhaphy of all major nerves because the fascicles are largely motor and the most common site of injury is close to motor end plates.
- Tendon transfers: Tendon transfers provide good results if nerve reconstruction fails in patients with radial nerve palsy.
- Nerve transfer: The use of nerve transfers for severe brachial plexus injuries when other options were not available.
Physiotherapy Treatment of Radial Nerve Injury
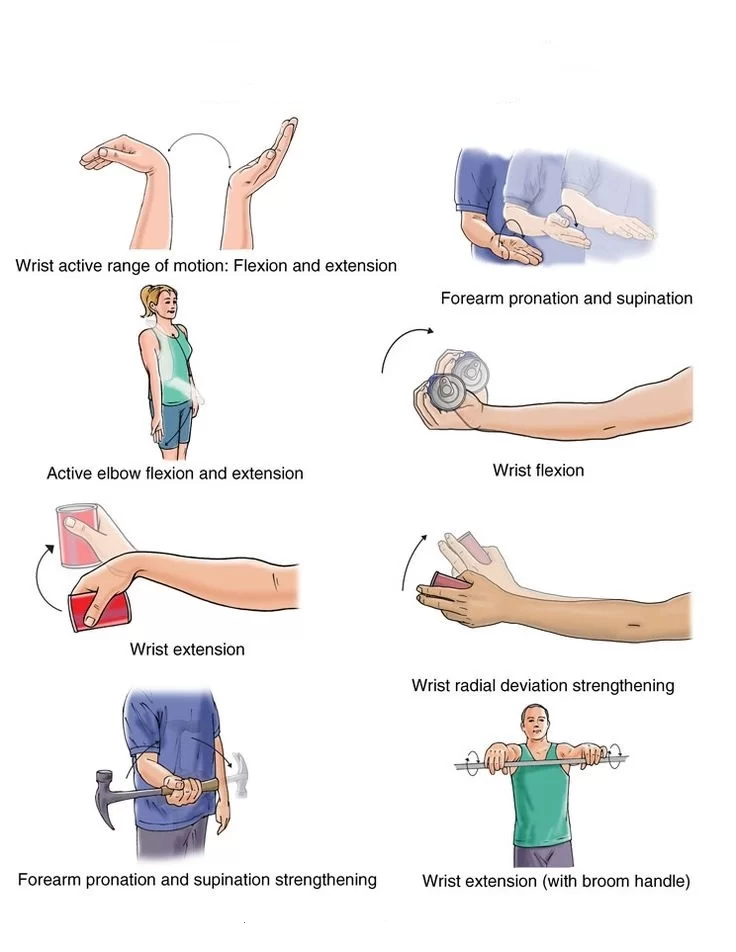
- Physiotherapy helps strengthen your arms, to avoid risk of radial nerve injury. It teaches proper balance exercises, to avoid falls. The correct posture at the workplace and during sleep is also taught to the patient.
- Physiotherapy can help you manage medical conditions, such as diabetes and kidney stones, thus, preventing risk of radial nerve injury.
- A physiotherapist uses modalities such as electrical stimulation (TENS), to help with the pain from the radial nerve. The electrical impulses sent from the TENS unit help desensitize the radial nerve endings.
- Physical therapy involves the use of massage therapy. Massage therapy can help reduce any swelling that compresses the radial nerve. This happens because massage therapy helps drain fluids from lymph channels.
- Most importantly, physical therapy facilitates the recovery of an injured radial nerve, by improving blood circulation. It also returns mobility to the wrist and fingers through gripping exercises. These gripping exercises help with conditions such as wrist drop.
POSTOPERATIVE REHABILITATION:
- A cock-up wrist splint is used as long as a wrist drop persists to prevent the development of a wrist flexion
contracture. The splint may be removed during therapy to allow for wrist range of motion exercises. - Dynamic splinting is another option, especially for highly motivated and engaged patients. Use of the
wrist splint is discontinued only after active wrist extension has been regained. The development of a permanent 15-degree elbow flexion contracture is not uncommon, but this risk can be minimized by avoiding
excessive flexion of the elbow during nerve repair and postoperative immobilization.
Prevention
- Avoid repetitive arm movements. Do not stay long in cramped spaces or positions that restrict your arm movement. At the workplace and during sleep, adopt a healthy posture and switch between tasks often.
- Radial nerve injury can aggravate to radial nerve palsy, a much more serious condition. Get in touch with an expert physiotherapist if you notice symptoms of radial nerve injury.
FAQs
What happens when the radial nerve is injured?
lack of finger coordination and muscle weakness. Having trouble elbow-straightening the arm. difficulty gripping the hand or bending it back at the wrist. In the areas the nerve regulates, there may be pain, numbness, diminished sensation, tingling, or burning.
What is the most common site of radial nerve injury?
The most common site of radial nerve injury is in the upper arm, specifically in the region known as the “radial groove” or “spiral groove” of the humerus bone. The radial groove is a shallow groove located on the back (posterior) aspect of the humerus, and it serves as a pathway for the radial nerve as it travels from the upper arm to the forearm.
What muscles are affected by radial nerve palsy?
muscles are affected by radial nerve palsy are:
Triceps brachii
Brachioradialis
Extensor carpi radialis longus
Extensor carpi radialis brevis
Extensor digitorum
Extensor digiti minimi
Extensor pollicis longus
Extensor pollicis brevis
What are the symptoms of radial injury?
Radial nerve palsy symptoms and signs are:
From the triceps to the fingertips, numbness or decreased sensation.
Loss of motor control: issues with wrist or finger extension.
Muscle Weakness issues with grasping and pinching.
weakness or lack of control of the triceps-to-fingers range of muscles.
Wrist drop occurs when the patient is unable to move their wrist upwards
Muscle atrophy
Pain and inflammation
How do you treat a radial nerve injury?
Treatment for a radial nerve injury may depend on the severity and location of the injury. Rest, Medication, Physical therapy, Nerve gliding exercises, and splinting are common conservative treatments for radial nerve injury.
In severe cases, where the nerve is severely compressed or damaged, surgical intervention may be necessary to release the pressure on the nerve or repair the injured nerve.
How do you test for radial nerve injury?
The patient is placed in a supine while being subjected to the ULNT2b, an upper limb neurodynamic test for the radial nerve. The joints are manipulated sequentially until they reach their maximum range of motion or until symptoms appear.