Avascular necrosis of talus and physiotherapy treatment
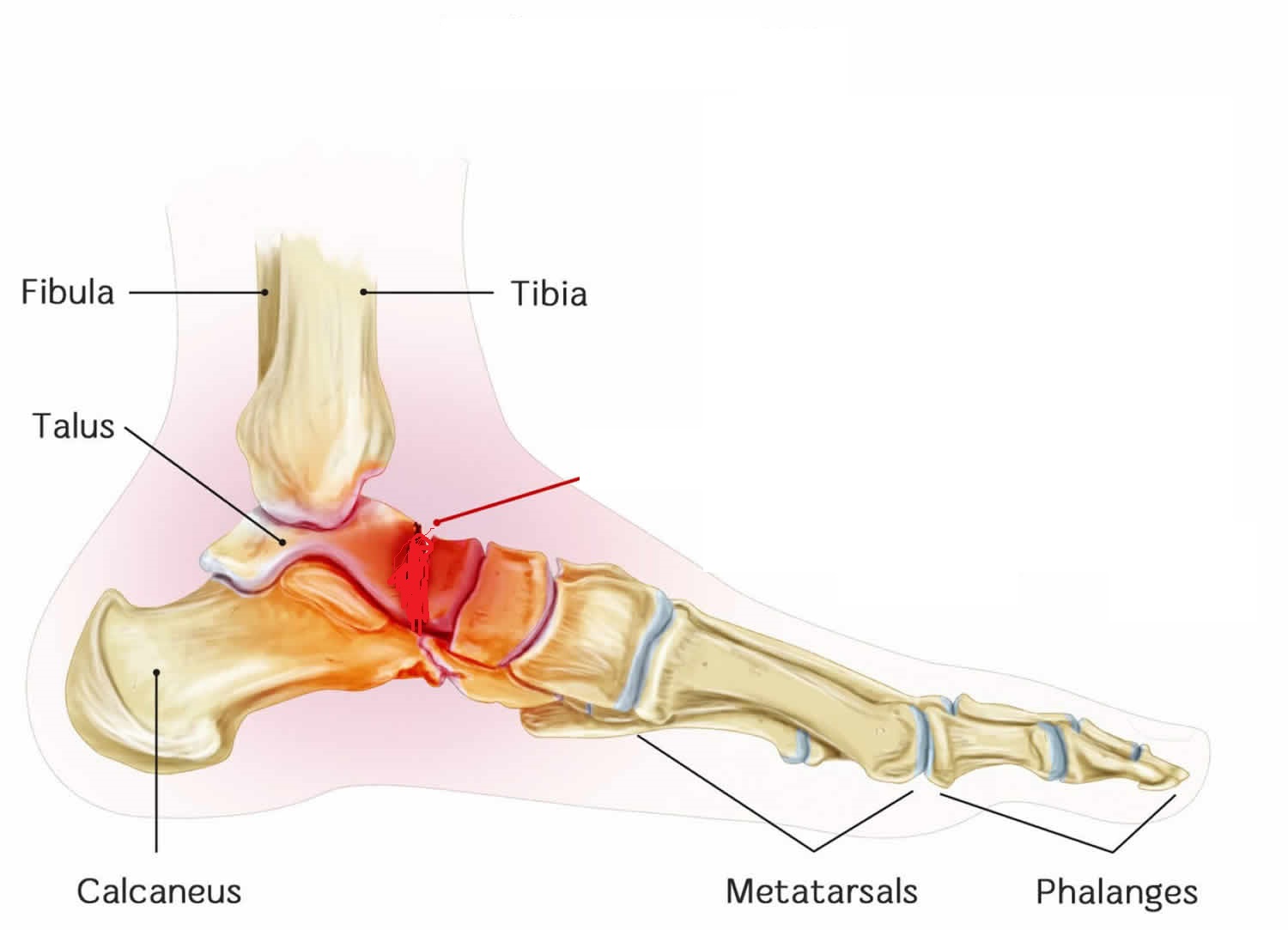
- Avascular necrosis of talus is a condition in which talus deprives of adequate blood supply. Avascular necrosis occurs due to the temporary or permanent loss of the blood supply to an area of bone.
- As a result, the bone tissue dies and the bone collapses. If AVN involves the bones of a joint (e.g.: the talus) it often leads to the destruction of cartilage, resulting in arthritis and pain. In the case of the talus, three joints can be affected:
- Ankle joint
- Talonavicular joint (a joint in the middle of the foot)
- Subtalar joint (the joint below the ankle)
- The ankle joint allows up and down movement of the foot, while the subtalar and talonavicular joints allow in and out the movement of the foot. The normal function of the subtalar joint is to allow walking on uneven surfaces, inclined surfaces, ladders, etc. without falling.
Causes of Avascular necrosis of the talus
- AVN can be caused by two large categories:
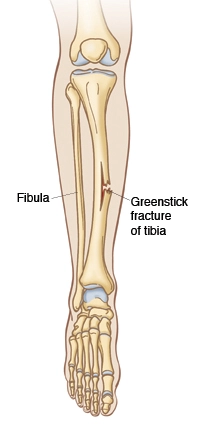
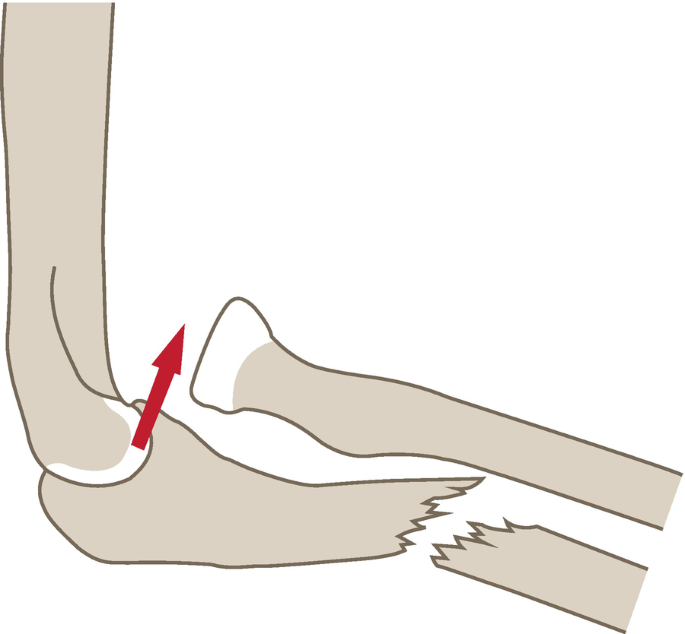
- Trauma – a fracture (breaking) of the bone disrupts the blood supply to the bone.
- Nontraumatic – include idiopathic (no cause is ever found), steroids (e.g.: anabolic and high dose corticosteroids (prednisone) given for such diseases as rheumatoid arthritis, lupus, and cancer), excess alcohol consumption, sickle cell anemia, radiation treatments, and chemotherapy.
- Avascular necrosis of the talus can be quite devastating and lead to a total loss of the ankle joint with arthritis, deformity, and pain. The development of AVN is determined to a large extent by the type of talus fracture.
- There are those fractures that are not very severe (they do not shift or displace much), and in these fractures, the incidence of AVN is lower. However, when the talus dislocates out of the ankle socket, the incidence of AVN is very high, almost 100%.
- The development of AVN is related to the type of fracture and not the manner in which it is treated. This is because of the blood supply to the talus, which is torn with certain fracture types, and not with others, and regardless of how the talus is put back together, the blood supply cannot change. Interestingly, however, the presence of AVN does not change the rate of healing of the fracture.
- The healing of the fracture is called a “union”. If the fracture does not heal at all, this is a “non-union”, and if the fracture heals in a poor position, this is called a “mal-union”.
- Even in fractures where AVN does develop, the fractured bone invariably goes on to union. There seems to be just enough blood supply left coming across the fracture to heal it, but not enough to maintain the blood supply for a totally viable talus. This is important when planning treatment following treatment of the fracture.
- The care of the limb after any fracture in the foot and ankle is based upon the premise that a limited amount of standing, walking and bearing weight on the foot is permissible.
- This makes sense, since pressure on the fracture with walking before the fracture has healed will lead to a shift in the bones resulting in a non-union, or a malunion.
- This has particular relevance with the fracture of the talus where one is concerned about the development of AVN, since the surgeon is understandably concerned about the consequences of bone healing if AVN occurs.
- If AVN does occur, the talus can break up into small pieces, fragment and collapse. This is not predictable. The majority of fractures that develop AVN do not go on to collapse, and the AVN is limited to small segments of the talus.
- Once the fracture has healed, the bearing of weight on the leg is actually permissible. There is no evidence to suggest that the patient has to remain off the foot using crutches for an indefinite period of time to prevent the talus from collapsing further.
- The foot may need to be protected, using a boot or a brace, and certain activities with an impact on the leg may need to be restricted, but walking should be acceptable.
- Once the collapse of the talus occurs, then problems begin, including arthritis and deformity. These are very difficult to correct surgically, but with newer reconstructive treatments available, have been very successful.
Symptoms of Avascular necrosis of the talus :
- In its early stages, AVN usually doesn’t have symptoms. As the disease gets worse, it becomes painful.
- At first, it might only hurt while bearing weight on the affected leg. Then, pain may become constant. If the bone and surrounding joint collapse, there may have severe pain that makes it unable to use joint.
- The time between the first symptoms and bone collapse can range from several months to more than a year.
Diagnosis of Avascular necrosis of the talus :
Diagnosis of avascular necrosis of the talus may involve:
- MRI
- X-ray
- CT Scan
Conservative treatment
Medications
- Blood thinners. if AVN is caused by blood clots.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). These will help with the pain.
- Cholesterol drugs. They cut the amount of cholesterol and fat in the blood, which can help prevent the blockages that lead to AVN.
Treatment options for avascular necrosis of the talus include:
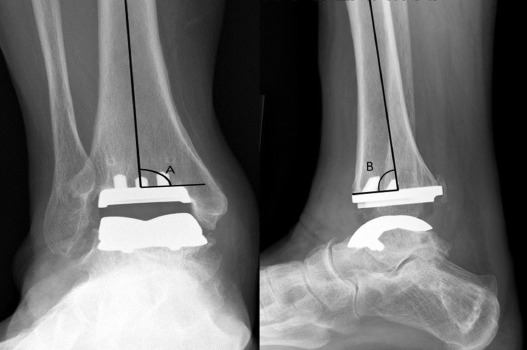
- Ankle Fusion – traditionally, when arthritis of the ankle joint occurs after AVN and talus fracture, a fusion of the ankle may be recommended. This fusion is a complicated operation and the results of the fusion are not always predictable and ankle motion is lost. For this reason, alternative treatments are desirable.
- Core Decompression – a surgical procedure in which a hole is drilled in the talus, which may lead to decompression of the bone and resultant healing of the talus because it increases the blood supply to the talus. It can only be used at the early stages of AVN.
Physiotherapy Treatment
- Appropriate treatment for avascular necrosis is necessary to prevent further deterioration of the joint. If untreated, most patients will experience severe pain and limitation of movement within two years.
Nonoperative treatment involves three main goals:
- Relief of symptoms
- Prevention of disease progression
- Improvement of functionality
- the patient should avoid bearing weight on the affected leg
- fully prohibited to walk on uneven surfaces
- Nonoperative treatment begins with patient education and addressing known risk factors, such as smoking and alcohol abuse. In addition, corticosteroids should be avoided.

- TENS: transcutaneous electrical nerve stimulation is an electrical modality that provides pain relief by providing pain modulation.TENS closes the gate mechanism at the anterior grey horn in the spinal cord. also stimulates the endogenous opioid system which prevents the release of substance p at the anterior grey horn.

- IFT: Interferential current therapy produces a low-frequency effect at targeted tissue, it inhibits transmission of pain impulses, stimulates the endogenous opioid system, increases blood supply, relieves edema, and removes the waste products.
ankle joint Range of motion exercise
- dosiflexion
- plantarflexion
- eversion
- inversion
- To assist the patient in regaining function and relieve painful symptoms, crutches or other gait aids can be introduced. The physiotherapist should instruct the patient on how to properly use these devices.
- By using crutches, the load that the talocalcaneal joint bears, will be decreased. This weight-bearing restriction is an important conservative treatment.
- Physiotherapy treatment focuses on exercises to maintain joint mobility and strengthen the muscles around the affected joint. During physiotherapy, excessive compressive and shear forces on the joint should be avoided. The outcome depends on the lesion’s size and stage at the initiation of the treatment.

- In order to maintain joint mobility, both passive and active exercises should be initiated. Passive exercises contain passive movements of the ankle joint.
- Active exercises consist of an active range of motion of the ankle. In the next stage, strengthening exercises are added. These exercises will focus on the muscles of the ankle and knee joints. To improve functionality it is important to implement endurance training and coordination training in a more advanced stage of the therapy.
- Physiotherapy after surgery is also a key component of recovery. It starts immediately the day after surgery. They prepare the patients for discharge by showing them how to do their everyday activities like getting in and out of bed and walking with a walker or crutches.
some other related topics :




One Comment