Radius Bone
Introduction
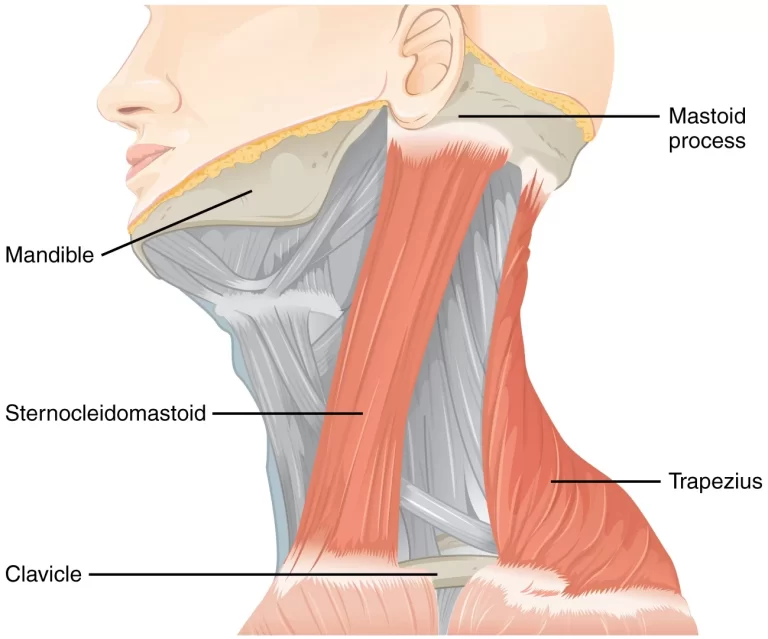
One of the bones in your forearm is your radius. It facilitates wrist and arm movement. Your injured radius may also affect the muscles and nerves that are connected to it.
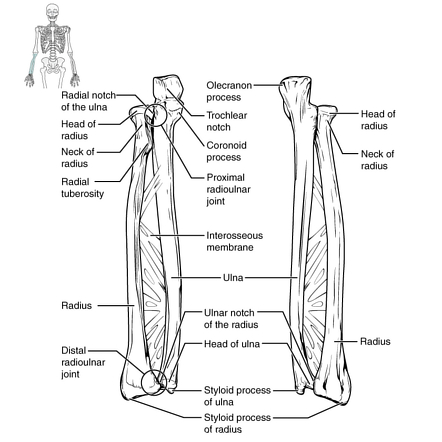
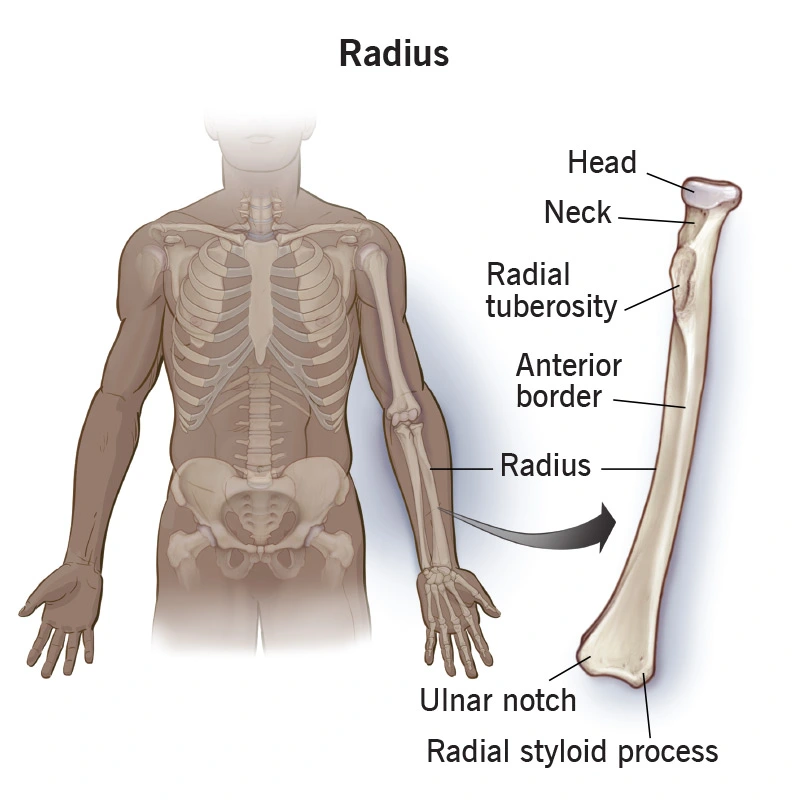
The radius is the longest bone in the forearm. It is situated parallel to and laterally to the ulna, the second forearm bone. At the proximal and distal radio-ulnar joints, movement is produced by the radius pivoting around the ulna.
The ulna and the radius are the two bones that together make up the forearm. At the wrist, it creates the radio-carpal joint, and at the elbow, the radio-ulnar joint.
When in the anatomical position, it is situated in the lateral forearm and resembles the tibia of the lower limb. The radius bone has an upper end, a lower end, and a shaft. It is smaller than the ulna.
One of the two long bones in the forearm, the radius (plural: radii) is situated laterally in the supinated anatomical position. From a smaller proximal end, it expands to a larger distal end (against the ulna).
One of the two big forearm bones—the other being the ulna—is the radius, sometimes known as the radial bone. It runs parallel to the ulna, which is longer and larger than it and stretches from the lateral side of the elbow to the thumb side of the wrist.
It is a long, prism-shaped bone with a small longitudinal curvature. The head of the ulna, the radial notch, and the capitulum of the humerus are the points at which the radius articulates. The tibia is the equivalent bone in the lower leg.
“Ray” is what the Latin word radius means. A ray can be conceptualized as rotating around an axis line that runs diagonally from the center of the capitulum to the center of the distal ulna in relation to the radius bone.
Overview
One of the two main bones of the forearm, the other being the ulna, is the radius, sometimes known as the radial bone (plural: radii or radiuses).
It runs parallel to the ulna and extends from the lateral side of the elbow to the thumb side of the wrist. Although the radius is thicker, the ulna is longer. The radius is a long, prism-shaped bone with a small longitudinal curvature.
The radius is a component of the wrist and elbow joints. It joins the humerus at the elbow and, at the radial notch, the ulna.
At the wrist, the radius and ulna bones connect.
What is radius Bone?
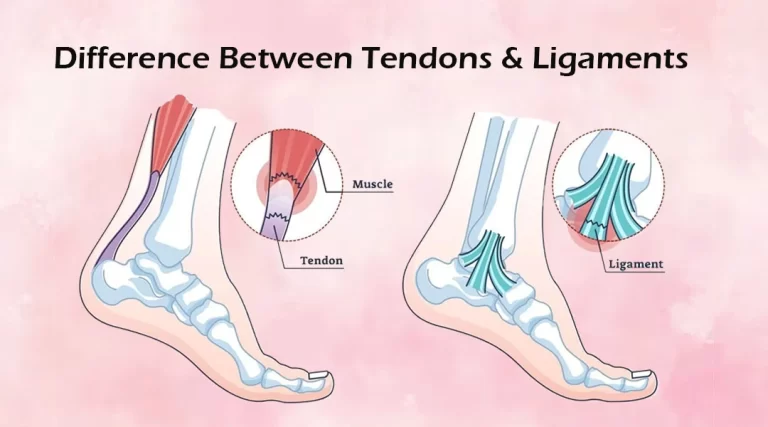
One of the bones in your forearm is the radius. It facilitates wrist and arm movement. Your radius supports a number of important muscles, tendons, ligaments, and blood vessels.
If you sustain a fractured (broken) radius, you may require both physical therapy and surgery to help you restore your strength and range of motion.
Osteoporosis can affect any bone, even the radius.
Your radius is linked to a great number of muscles and nerves, therefore injury to one can frequently have an impact on the others.
The ulna and the radius are the two long bones that together make up the human antebrachium. The radius is prismoid shaped, with the base being wider than the anterior border, and it has three borders and three surfaces.
The radial notch of the ulna and the capitulum of the humerus articulate proximally at the elbow joint. It articulates with the ulna at the ulnar notch and the articular surfaces of the lunate and scaphoid carpal bones at its distal end.
The radius’s closest point to the user is known as the radial head. The cylindrical head contains the articular disc, which articulates with the humeral capitulum and the radial notch of the ulna.
The biceps brachii muscle attaches to the oval-shaped neck of the radius and radial tuberosity, which is located distal to the radial head.
The radius shaft, which is distal to the radial tuberosity, is where the pronator teres, pronator quadratus, supinator, and extrinsic hand muscles attach.
Distal radius fractures represent 8% to 15% of all adult bone-related injuries and are among the most frequent low-energy fractures observed in ambulatory orthopedics.
It is the most frequently fractured bone in the elderly, second only to the hip.
Pediatricians also frequently see injuries such as subluxation of the annular ligament, which stabilizes the proximal radius.
Anatomy
The radius is commonly regarded as the larger of the two long bones in the forearm because it is wider at the wrist and narrower at the elbow than the ulna.
Most persons have an inch or so more of ulna length than radius length, though there are wide variations in length.
The radius is more prone to fracture than the ulna among the two forearm bones. Over half of all forearm fractures in children involve only the radius, 6% only the ulna, and 44% both.
Adults also frequently suffer from radius fractures. Up until their mid-40s, men and women experienced similar cases of radius fractures; after that, women experienced them far more frequently than men.
Location of Radius in body
One of the two bones in your forearm is your radius. Your ulna is the other one. On the lateral (thumb) side of your forearm, the radius is located in opposition to your ulna.
When you extend your arm straight out in front of you, palms down, your radius spins over your ulna. Your arms are more parallel to one another when you hold them straight out and face up.
The forearm, or the portion of the arm between the elbow and the wrist, contains the radius. The radius is positioned parallel and lateral to (outside of) the ulna in the anatomical position, with the arms straight and the palms facing forward at hip level.
The distal (far) ends of the radius and ulna cross when the body is at rest, such as when your hands are on a keyboard, with the radius resting on top of the ulna.
At the distal end of the humerus, the elbow joint’s lateral (outside) margin is composed of the proximal end of the radius. The radius’s distal end joins the wrist immediately in front of the thumb.
The wrist can rotate at the distal radioulnar joint due to the ulna’s and radius’s revolving motion. The ulna and humerus perform the majority of the effort at the radiohumeral joint, however, the radius facilitates motion and stabilizes the elbow hinge joint.
The proximal radioulnar joint is a region of movement that exists between the proximal ends of the radius and the ulna.
Connecting the radius and ulna is a thick layer of fibrous tissue called the interosseous ligament, sometimes referred to as the interosseous membrane. Between the proximal ends of the radius and ulna is a smaller ligament.
Its fibers run in the opposite direction of the interosseous ligament, giving it the names “oblique ligament” and “oblique cord.”
How does the radius appear?
Three sections make up your radius: a long, slightly curved shaft in the center; a small end where it joins the humerus, the upper arm bone; and a bigger end where it meets the wrist.
It is thicker and a little bit shorter than your ulna.
Despite being a single long bone, your radius is actually composed of several pieces.
The robust wall of compact bone encloses the long, narrow medullary cavity. Similar to how it is thinnest at the extremities and broadest at the interosseous border, it is also cup-shaped across the head’s fovea or articular surface.
The spongy tissue’s trabeculae have a slightly curved upper end and rise from the shaft’s compact layer to the humerus’s cup-shaped articulatory notch, the fovea capituli.
Other trabeculae cross these above, parallel to the fovea’s surface. There is some similarity in the arrangement at the bottom end. As with radial aplasia, it is absent.
There are two extremities and a body on the radius. The radial tuberosity, neck, and slightly cylindrical head that articulates with the ulna and humerus make up the upper extremity of the radius.
The ulna, scaphoid, and lunate bones have articular surfaces on the lower extremity of the radius, which is typically quadrilateral in shape. The radius’s body is self-explanatory.
The styloid process and Lister’s tubercle on the ulnar side are the two palpable points formed by the distal end of the radius.
The proximal and distal radioulnar articulations, as well as the radius, are joined to the ulna by an interosseous membrane that extends medially throughout the length of the radius body.
Structure of the Radius Bone
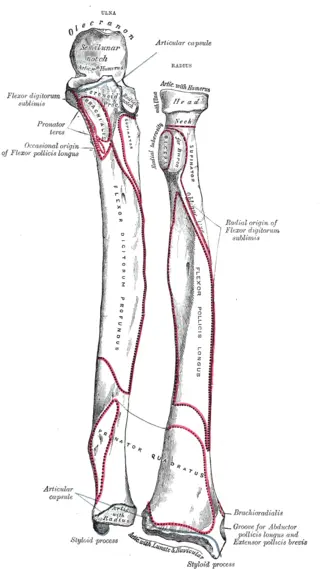
Hyaline cartilage covers the cylindrical radial head, which articulates with the humerus’s capitellum at the elbow joint.
The radial head’s circumference is made to precisely fit into the socket formed by the annular ligament and the radial notch of the ulna, establishing the superior radioulnar joint.
The forearm can supinate or pronate as a result of this joint’s ability to rotate the head within the annular ligament.
The proximal end of the Radius Bone
Your radius’s higher (proximal) end is attached to your humerus.
The proximal end is the:
Head
The radial head is cylindrical in shape, and it contains a shallow cup-shaped area on top called a fovea that is used to articulate with the humerus’s capitulum (also known as the capitellum).
The head’s circumference is smooth; where it joins the radial notch of the ulna, it is broad medially; the remainder of its circumference, which is covered by the annular ligament, is narrow.
When the body pronates or supinates, a cam effect is produced because the deepest point in the fovea is not axisymmetric with the long axis of the radius.
A disk-shaped structure with a concave articulating surface. Where it participates in the proximal radioulnar joint, medially, it is thicker.
Neck
The neck, which is spherical, smooth, and constricted and has a small hump on the back where a segment of the supinator muscle inserts, supports the head.
The neck is a small region of bone that sits between the radial tuberosity and the radial head.
Radial tuberosity
The bony protrusion known as the radial tuberosity is where the biceps brachii muscle attaches.
The radial tuberosity is an eminence located on the medial side beneath the neck.
Its surface is divided into two parts: an anterior smooth area that houses a bursa between the tendon and the bone, and a posterior rough region where the biceps brachii muscle tendon insertion is located.
Body of the Radius Bone
A lengthy stretch of bone that extends away from the neck and radial tuberosity is known as the radius shaft. It is a little up close but gets bigger as it gets closer to the wrist, where it widens to create the distal end of the radius.
For the majority of its length, the radial shaft has a triangular cross-section with a small lateral curvature. The radius shaft has a small curvature that makes it convex from the body.
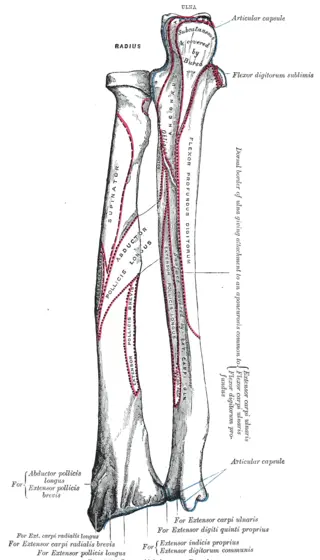
The anterior, posterior, and interosseous boundaries encircle the bulk of the shaft.
The radius’s body, also known as its shaft, has a prism shape, is convex lateralward, and is narrower above than below.
The radius has three surfaces—volar, dorsal, and lateral—as well as three borders—volar, dorsal, and internal.
The dorsal border separates the lateral and posterior surfaces from the volar and volar surfaces, the internal (interosseous) boundary separates the volar and dorsal surfaces from the lateral and volar surfaces.
Borders
- The volar border
The volar border, also known as the margo volaris, anterior border, or palmar, divides the volar from the lateral surface. It runs from the lower portion of the tuberosity above to the anterior section of the styloid process base below.
Because of its oblique direction, its upper third is very noticeable and is referred to as the radius’s oblique line. It is where the flexor digitorum superficialis and flexor pollicis longus muscles originate, and a portion of the supinator muscle inserts on the surface above the line. The middle part of the volar border is rounded and unclear.
The brachioradialis muscle tendon is placed into the tiny tubercle at the end of the prominent lower fourth, which also serves as the attachment point for the dorsal carpal ligament and the insertion point of the pronator quadratus.
The medial aspect of the bone is where the anterior border is located. It begins at a point that is relatively distal to the radial tuberosity and travels diagonally to the shaft’s lateral face.
- The dorsal border
The posterior and lateral surfaces are separated by the dorsal border, often referred to as the posterior border or margo dorsalis.
It starts above the rear of the neck and terminates below the posterior portion of the styloid process base.
It is clearly visible in the central part of the bone but is hardly noticeable above or below.
Located on the posterior portion of the radius, the posterior boundary is most visible at the center of the shaft.
- The interosseous border
The interosseous border (also known as the internal border, crista interossea, or interosseous crest) starts at the back of the tuberosity and is rounded and indistinct in its upper part.
As it descends, it becomes sharp and prominent and splits into two ridges at the lower part, which continue to the anterior and posterior margins of the ulnar notch.
The lower portion of the interosseous membrane is linked to the posterior of the two ridges, and a portion of the pronator quadratus muscle is inserted into the triangle that forms the space between the ridges.
The volar is separated from the dorsal surface by this crest, which also connects to the interosseous membrane. Actually, it’s called a syndesmosis joint, and it joins the two bones.
The ulna is medially faced by the acute interosseous boundary. The fibrous interosseous membrane connects this border to the ulna’s interosseous border, establishing the middle radioulnar joint.
Surfaces
- The volar surface
The volar surface, also known as the anterior surface or facies volaris, is broad and flat in its lower fourth and provides insertion for the Pronator quadratus muscle.
It is concave in its upper three-fourths and gives origin to the flexor pollicis longus muscle. The volar radiocarpal ligament attaches to a triangular rough surface between the inferior border and a conspicuous ridge that limits the insertion of the pronator quadratus below.
At the meeting point of the volar surface’s middle and upper thirds lies the nutritional foramen, which points obliquely upward.
Between the anterior and interosseous boundaries is its anterior surface.
- The posterior surface
The posterior surface, also known as the facias dorsalis, is covered by the supinator and has a convex upper third that is smooth.
Its wide, somewhat concave middle third is the source of the extensor pollicis brevis muscle below and the abductor pollicis longus muscle above.
The tendons of the muscles that subsequently run in the grooves on the bottom end of the bone cover its broad, convex lower third.
Between the posterior borders and the interosseous surface is the posterior surface.
- The lateral surface
The lateral surface, which is situated between the anterior and posterior borders, has a modest convexity.
Known as the convexity of the radius, the lateral surface (facies lateralis; exterior surface) is convex over its whole extent and curves outward to be convex at the side.
The supinator muscle inserts into its upper third. There is a rough ridge around the center of it where the pronator teres muscle inserts.
The tendons of the extensor pollicis brevis and abductor pollicis longus muscles cover its small bottom portion.
The distal end of the Radius Bone
The radius’s shaft enlarges to create a broad, four-sided distal end that is rectangular in shape and extends beyond the ulna’s distal end.
Your wrist joint is formed by the distal, or lower, end of your radius. Where it joins the lunate (the wrist or carpal bones) and scaphoid, it is wider than the remaining segment of your radius.
Radius’s distal end are:
Styloid process
- In contrast, the distal radius has a rough lateral surface that extends inferiorly as the radial styloid process.
Ulnar notch
- The distal radius has a smooth, concave anterior surface that is inclined anteriorly. The medial surface concavity known as the ulnar notch, which retains the head of the ulna, forms the distal radioulnar joint.
These sections and labels serve primarily as a tool for your healthcare professional to identify areas of your body where you are experiencing pain or other problems.
Your healthcare professional may refer to the area of your bone damage using some of this terminology if you ever break your radius or suffer a radial fracture.
Joint surfaces
It has two articular surfaces: one on the medial side for the ulna and one below for the carpus.
The concave, smooth, triangular carpal articular surface is divided into two parts by a tiny ridge running anteriorly and posteriorly. Of them, the triangular lateral one articulates with the scaphoid bone, while the quadrilateral medial one with the lunate bone.
The ulnar notch, that is, the sigmoid hollow of the radius, is the ulna’s articular surface. It is smooth, concave, and thin, and it articulates with the ulna head.
The base of the triangular articular disk, which divides the wrist joint from the distal radioulnar articulation, is related to the conspicuous ridge that divides these two articular surfaces.
Other surfaces
- Lateral articular surface
It goes on to create the styloid mechanism.
The lateral surface extends downward at an oblique angle to form the styloid process, a strong, conical projection that attaches to the wrist joint’s radial collateral ligament at its apex and the brachioradialis tendon at its base.
For the tendons of the extensor pollicis brevis and abductor pollicis longus muscles, this process’ lateral surface is identified by a flat groove.
- The medial articular surface
features an ulnar notch that is concave and articulates in pronation with the ulnar head.
- The posterior articular surface
convex and has a noticeable ridge known as Lister’s tubercle
There are three grooves on the dorsal surface, which are convex and allow attachment to the dorsal radiocarpal ligament.
From the side that faces you, listed are:
- The lateral of these two channels conveys the tendon of the extensor carpi radialis longus muscle, while the medial channel transmits the tendon of the extensor carpi radialis brevis muscle. The first groove is shallow, broad, and separated into two by a minor ridge.
- The second is deep but thin, with a sharply defined ridge enclosing it laterally. It is directed laterally and obliquely downward from above, transmitting the tendon of the extensor pollicis longus muscle.
The dorsal tubercle, also known as Lister’s tubercle, is a noticeable bony projection on the posterior aspect of the distal radius that is located in between the grooves that carry the tendons of the forearm muscles.
- Anterior articular surface
It extends from the anterior margin of the radial tuberosity to the styloid process, where it forms a distinct and smooth margin.
The volar radiocarpal ligament can be attached to the uneven and rough volar surface.
- Distal articular surface
articulates with the scaphoid laterally and the lunate medially.
- Inferior articular surface
Two facets on the inferior surface, also known as the carpal articular surface, articulate with the carpus’s scaphoid and lunate bones.
Attachments on The Radius
At the Elbow joint
In the synovial pivot joint, the radius and ulna articulate. Pronation of the forearm results from the rotation of the radial head within the annular ligament & radial notch on the ulna.
Supination is also produced by the distal articulation of the ulna and radius in the opposite direction of their elbow articulation. This movement takes place when the ulna’s head enters the radius’s ulnar notch.
At the Wrist joint
The radio-carpel joint is formed by the radius’s articulation with the first row of carpal bones, primarily the scaphoid laterally and the lunate medially.
The triquetral bone only occasionally makes contact during ulnar abduction.
The radio-carpel junction is an ellipsoid joint in which the convex surface of the scaphoid, lunate, and triquetral bones articulates with the concavity of the distal radius.
Attachments on the Bone
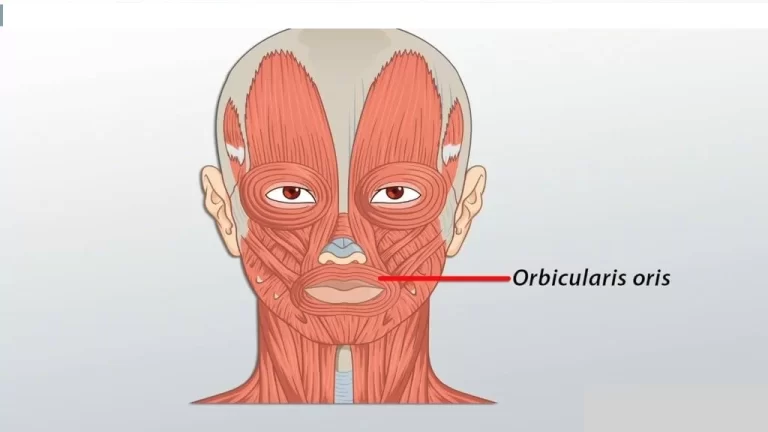
Muscle Attachment on the Bone
- Radial tuberosity:
Biceps brachii
- Styloid process:
- Middle surface:
Flexor digitorum superficialis
Flexor pollicis Longus
Pronator quadratus
- Lateral Surface:
Supinator
Pronator Teres
- Posterior Surface:
Longus Abductor Pollicis
Brevis Extensor Pollicis
There are two compartment
The anterior and posterior compartments comprise the forearm muscles. The muscles that enable forearm supination, finger extension, and wrist extension make up the majority of the posterior compartment.
The majority of the muscles responsible for wrist flexion, finger flexion, and forearm pronation are found in the anterior compartment.
- Anterior
The superficial, middle, and deep layers comprise the divisions of the anterior compartment. The flexor carpi ulnaris, palmaris longus, flexor carpi radialis, and pronator teres are the muscles of the superficial layer.
The flexor digitorum superficialis is the only muscle found in the intermediate layer. The deep anterior layer is composed of the flexor digitorum profundus, flexor pollicis longus, and pronator quadratus.
- Posterior
There are superficial and deep layers in the forearm’s posterior compartment. The brachioradialis, extensor carpi radialis brevis, extensor carpi radialis longus, extensor digitorum, extensor digiti minimi, extensor carpi ulnaris, and anconeus muscles are the muscles of the superficial layer.
the posterior layer is:
- Supinator
- Abductor pollicis longus
- extensor pollicis brevis
- extensor pollicis longus
- extensor indicis muscle
Ligaments and Joints:
The lateral collateral ligament complex, made up of four challenging-to-separate ligaments, is the collective name for the lateral ligaments of the elbow.
The lateral collateral ligament (also known as the “radial collateral ligament”) first joins the annular ligament at the lateral epicondyle of the humerus. The lateral collateral ligament shields the antebrachium from varus stress by connecting the radius and humerus.
Pronation and supination of the radial head are made possible by the annular ligament, which encircles the ulna from the anterior to the posterior radial notch.
The ulnar supinator crest and the lateral epicondyle of the humerus are where the lateral ulnar collateral ligament is attached. The antebrachium is shielded from valgus stress by the lateral ulnar collateral ligament.
Lastly, to add even more support to the joint, the accessory lateral collateral ligament connects the inferior edge of the annular ligament to the supinator crest.
This interosseous membrane lies between the medial border of the radius and the lateral border of the ulna, dividing the anterior and posterior compartments of the antebrachium.
The interosseus membrane permits force distribution throughout the forearm and acts as a point of attachment for muscles. Forearm supination teaches the interosseous membrane fibers, which stabilize the proximal and distal joints.
Similar to the lateral collateral ligament complex, the interosseous membrane is made up of several difficult-to-separate ligaments.
The proximal oblique cord, accessory band, central band, dorsal oblique accessory cord, and distal oblique bundle are the five ligaments of the interosseous membrane.
The articular disc sits between the distal ulna and radius, and the palmar radioulnar ligament (volar radioulnar ligament) attaches the anterior radius to the anterior ulna.
Known also as the posterior radioulnar ligament, the dorsal radioulnar ligament is attached between the posterior ulna and posterior radius. These anatomical features facilitate the distribution of weight and permit the second pivot during forearm pronation and supination.
The long and short radio lunate ligaments serve as the attachment points between the distal radius and the lunate bone. When the wrist is extended, these ligaments stop the lunate bone from hyperextending.
The radioscapocapitate ligament joins the volar side of the radius to the scaphoid and capitate carpal bones, while the radial collateral ligament of the wrist connects the distal radius to the scaphoid.
Last but not least, the dorsal radius is joined to the dorsal scaphoid, lunate, and triquetrum by the broad dorsal radio triquetral ligament.
Development
Three centers serve as the ossification points for the radius: one for the body and one for each extremity. In the 8th week of fetal life, the body appears in the vicinity of the bone’s center.
Ossification starts in the lower extremities between the ages of 9 and 26 months. By the 5th year, the upper-end ossification center is visible.
At 17 or 18 years old, the upper epiphysis merges with the body, while the lower epiphysis unites with the body at twenty years old.
A second center that occasionally develops around 14 or 15 years is located in the radial tuberosity.
Ossification foci
Ossifies from three points:
Body: First visible in the eighth week of fetal life
Proximal extremity: starts to appear at age 5 and combines with the body between 17 and 18 years old.
Distal extremity: Develops between the ages of 9 and 26 months and merges with the body at the age of 20.
Function of The Radius
Pronation and supine postures, as well as adduction, abduction, extension, flexion, and circumduction of the wrist, are all made possible by the radius of the hand and forearm.
The complex articulation that causes pronation and supination involves the cylindrical radial head, which is secured to the ulnar notch by the annular ligament
This configuration facilitates proximal rotation of the radial head, resulting in anteromedial distal radius displacement. To enable pronation of the wrist and hand, the distal radius inverts and passes over the distal ulna. This movement can be reversed to enable supination.
At the elbow joint, three articulations permit extension and flexion in addition to pronation and supination. The elbow joint consists of three joints: the humeroulnar articulation, the proximal radioulnar joint, and the pivot joint (radiocapitellar articulation).
The radius and humerus’s capitulum articulate as well. The antebrachium can flex and stretch with the brachium thanks to the olecranon of the ulna’s articulated trochlea of the humerus.
The biceps and brachialis contract, creating flexion and allowing the two bones to move as one unit. The two bones remain close to one another during this flexion because of the annular ligament. Facilitating pronation and supination is the main function of the proximal radioulnar joint.
Supination and pronation are made possible at a pivot joint located distally by the articulation of the ulnar head and the ulnar notch of the radius. The scaphoid and lunate bones allow the radius to articulate with the wrist.
The wrist can move in two planes due to this articulation, which is a condyloid or “ellipsoidal” joint. The wrist can bend, extend, circumduct, adduct, and abduct thanks to the radiocarpal joint.
The radius permits arm mobility, particularly the complete range of motion of the hand and wrist.3.Together, the ulna and radius offer leverage for object manipulation, including lifting and rotation.
The radius can also aid in providing mobility when crawling.
The study of embryology
The lateral plate mesoderm, which is the source of all long bones, is where endochondral ossification in the development of the radius starts.
The process by which bone replaces hyaline cartilage is known as endochondral ossification. Mesenchymal cells produced from mesoderm multiply quickly to form chondrocytes, which serve as a template for new bone formation.
Collagen and fibronectin are added to the matrix by chondrocytes in the model’s core, enabling calcification. The calcification stops nutrients from getting to the chondrocytes about week six of pregnancy.
At some point, the chondrocytes experience apoptosis. As chondrocytes leave behind voids, blood vessels multiply and finally form the medullary cavity.
Osteoblasts create the periosteal collar, a thick zone of compact bone in the diaphysis that marks the beginning of ossification, approximately during the 12th week of pregnancy.
Proliferating chondrocytes found in the epiphyseal plates (growth plates) at either end of the bone cause the bone to continue growing longer until adolescence.
Sex hormones trigger the formation of secondary ossification centers during puberty, and the epiphyseal plates ossify concurrently with the diaphysis.
Blood Flow and Lymphatic System
The radial and radial recurrent arteries provide the majority of the blood flow to the proximal radius.
Traveling proximally, the radial recurrent artery connects with the radial collateral artery. The radial, posterior interosseous, & anterior interosseous arteries deliver blood to the middle and distal radius.
The deep lymphatic vessels, which trail the deep veins like the brachial, ulnar, and radial veins, drain the lymph from the radius. The lymph nodes in the humeral axilla are the draining veins.
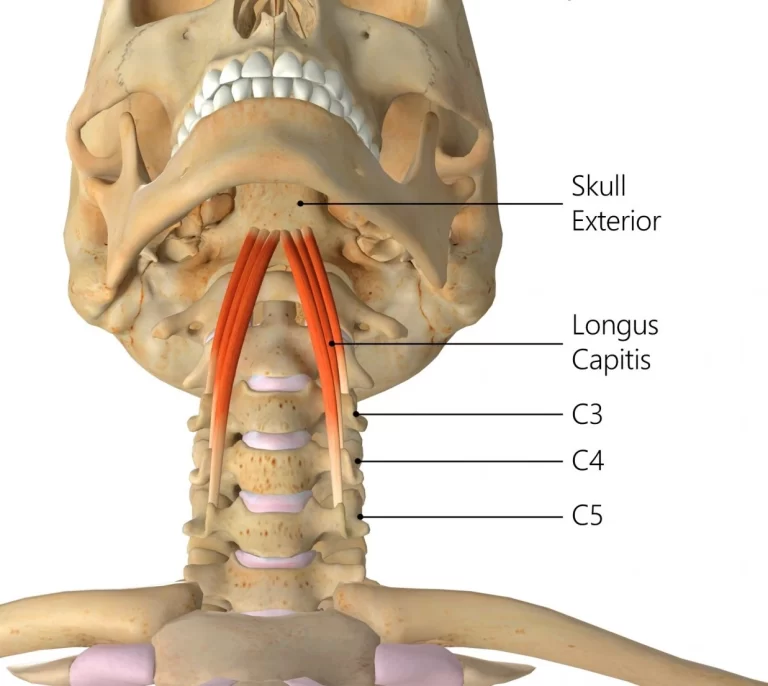
Nerves
The antebrachium receives motor and sensory innervation from the brachial plexus nerves.
- Extensor carpi radialis brevis
- abductor pollicis longus
- extensor carpi radialis longus
- supinator
- extensor carpi ulnaris
- abductor pollicis brevis
- extensor pollicis longus
- extensor pollicis brevis
- brachioradialis
- extensor indicis
- extensor digitorum
- extensor digiti minimi muscles
All these are innervated by the radial nerve, which also supplies sensory innervation for the posterior forearm.
The anteromedial and anterolateral forearms receive sensory innervation from the medial and lateral antebrachial cutaneous nerves, respectively.
The biceps brachii receive their motor innervation from the musculocutaneous nerve.
- Pronator teres
- flexor carpi radialis
- palmaris longus
- flexor digitorum superficialis
- flexor pollicis longus
- pronator quadratus
- flexor digitorum profundus muscle’s lateral half
All these muscle is innervated by the median nerve.
The flexor digitorum profundus and flexor carpi ulnaris muscles receive motor input from the ulnar nerve.
Clinical Pathologies and Anatomy
Fracture of the radius
A fracture is the most frequent medical problem affecting the radius. Despite being slightly thicker and shorter than the ulna, the radius fractures more frequently.
It would seem that greater force would be imparted to the longer ulna during falls or other injury processes. But among all age categories, the radius is the most frequently broken bone.
The radius receives the majority of the pressure during weight distribution during a ground-level fall in which the patient breaks the fall with their hands down. One can shatter the forearm’s radius alone, the ulna alone, or both of them.
The most typical kind of fractures of the radius bone are distal radial fractures. When a patient falls onto an outstretched hand, they are more likely to be elderly or pediatric patients than young adults.
Radial head fractures, which affect the proximal end of the radius, which forms part of the elbow, are common in elderly people.
Radius Common Fracture’s are:
The distal radius is also hurt in a colles fracture. The most common way that an avulsion fracture happens is when someone falls on an outstretched hand with their forearm pronated.
The bone fragment has moved dorsally, and the annular ligament has subluxed.
Clinically, It is called dinner fork deformity.
- Smith fracture.
A direct strike to the dorsal wrist or forearm frequently results in a distal radius Smith fracture.
An additional way to get hurt is to fall on a flexed wrist. In contrast to a Colles fracture, where the fragment is displaced dorsally, the fracture is displaced ventrally.
In contrast to nursemaid’s elbow, which usually exclusively affects patients in their pediatric years, distal radius fractures typically affect people who are younger than eighteen and greater than 50.
- Greenstick fracture.
Because young bone tissue is more malleable than mature bone tissue, pediatric patients are more susceptible to incomplete fractures, often known as “greenstick fractures.”
Patients who are not yet adolescents run the additional danger of harming the growth plate, or epiphyseal plate. A growth plate injury may lead to long-term malformation.
- Barton fracture.
Colles fracture and Barton fracture are extremely similar. It occurs most commonly when someone falls on an outstretched hand with their arm pronated. The distal radius shears as a result of the impact.
The radiocarpal ligaments are not damaged; instead, the fracture advances dorsally. The distal radius’s articular surface is still in touch with the scaphoid. What separates the Colle’s fracture from the Barton fracture is this distinction.
Subluxation
One of the most frequent pediatric injuries treated by ambulatory orthopedics is subluxation of the annular ligament, often known as nursemaid’s elbow or radial head subluxation.
It happens when a youngster under five years old has their hand or forearm suddenly pulled in a longitudinal direction. The ligament is stuck between the capitulum and the radial head when there is an abrupt traction that causes the radial head to slide out from under it.
The youngster typically exhibits a pronated forearm and a modest bending of the elbow when presenting, refusing to utilize the affected limb.
Holt-Oram syndrome (HOS).
Heart and upper limb abnormalities are caused by the autosomal dominant mutation in the TBX5 gene known as Holt-Oram syndrome (HOS).
The triphalangeal thumb or absence of thumbs, aplasia or hypoplasia of the radius, or union of the carpal and thenar bones are examples of upper-limb abnormalities.
Aberrant wrist adduction and abduction, as well as aberrant pronation and supination of the forearm, are caused by aplasia or hypoplasia of the radius.
Osteoporosis
Because osteoporosis weakens bones, unexpected and sudden fractures are more prone to occur. Osteoporosis usually doesn’t show any symptoms, so many individuals don’t know they have it until a bone breaks.
Adults over 65, women, and those allocated to the feminine gender at birth are more likely to develop osteoporosis. To prevent fractures and detect osteoporosis early, ask your doctor regarding a bone density test.
Nursemaid’s elbow
For young children, nursemaid elbow is a frequently occurring injury. Another name for it could be a “pulled elbow.” When a child’s radius contacts their elbow, it becomes slightly dislocated.
Kids’ ligaments are looser than adults’, which is why it occurs. A nursing mother’s elbow is caused by pulling on your child’s hand or arm. Usually, it occurs unintentionally as a result of actions like playfully picking up your child by the hands or pulling their arm to prevent them from walking into the street.
Maintaining the health of your radius
You may maintain good bone health (as well as general health) by proper diet, frequent exercise, and doctor visits.
If you are older than 50 or if osteoporosis appears in your family, talk to your doctor about having a bone density scan.
To lower your chance of injury, heed the following general safety advice:
- Wear your seatbelt at all times.
- When taking part in any sport or activity, wear the proper protective gear.
- Ensure that nothing might injure you or others in your house or business.
- Use the proper tools or equipment whenever you reach for anything at home. Never stand on chairs, tables, or worktops.
- Adhere to an exercise and dietary plan that will support the health of your bones.
- If you are prone to falls or have trouble walking, use a cane or walker.
FAQs
What type of bone is the radius?
Among the four different types of bones in the body is the long radius. A long bone is one that is sturdy, thick, and longer than it is wide. The shaft of a long bone is called the diaphysis, while the end is called the epiphysis.
Where is the radius bone located?
Your radius is one of the two forearm bones. Your ulna is the other one. On the thumb side of your forearm, the radius is located in opposition to your ulna. When you extend your arm outwards in front of you, palms down, your radius spins over your ulna.
What is Barton’s fracture?
A Barton fracture occurs when a wrist break occurs in one segment and knocks out another section. Usually, it occurs when you trip and fall on your bent wrist. Your distal radius, which breaks off from your wrist, is also a portion of your forearm. The most often fractured arm bone is your radius.
What is the distal radius in osteology?
The metaphyseal and epiphyseal zones are located in the distal portion of the radius, which has a quadrilateral cross-section. The distal radius has four surfaces—anterior, lateral, posterior, and medial—as well as the styloid process and the dorsal tubercle.
What is Smith’s fracture?
A Smith fracture is a distal radius fracture that is characterized by angulation or volar displacement of the distal fragment. Because the more common Colles fracture has a dorsally displaced distal fracture fragment, this condition is also referred to as a reverse Colles fracture.
What is Galeazzi fracture?
A distal third of the radius shaft fracture combined with a concurrent displacement of the distal radioulnar joint (DRUJ) is known as a Galeazzi fracture-dislocation. These injuries are typically caused by axial force on an extended arm, and the fracture’s angulation is determined by the wrist’s pronation or supination.
Reference
- Emt-P, R. B. (2023, June 6). The Anatomy of the Radius. Verywell Health. https://www.verywellhealth.com/radius-anatomy-4587596
- Bair, M. M. (2023, July 31). Anatomy, Shoulder and Upper Limb, Forearm Radius. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK544512/
- Professional, C. C. M. (n.d.). Radius. Cleveland Clinic. https://my.clevelandclinic.org/health/body/24528-radius
- Radius (bone). (2023, October 15). Wikipedia. https://en.wikipedia.org/wiki/Radius_(bone)
- The Radius – Proximal – Distal – Shaft – TeachMeAnatomy. (2020, May 10). TeachMeAnatomy. https://teachmeanatomy.info/upper-limb/bones/radius/
- Radius. (n.d.). Physiopedia. https://www.physio-pedia.com/Radius
- MSc, E. O. M. (2023, October 30). Radius and ulna. Kenhub. https://www.kenhub.com/en/library/anatomy/the-radius-and-the-ulna
- Baba, Y., & Olivier, M. (2014, April 28). Radius. Radiopaedia.org. https://doi.org/10.53347/rid-29037
- Micheau, A., & Hoa, D. (2024, January 15). Radius. e-Anatomy – IMAIOS. https://www.imaios.com/en/e-anatomy/anatomical-structure/radius-1537018740