Sacralization and Physiotherapy management
- Sacralization is a common irregularity of the spine, where the fifth vertebra is fused to the sacrum bone at the bottom of the spine. The 5th lumbar vertebra(L5) may fuse fully or partially on one side or on both sides. Sacralization is a congenital anomaly that develops in the embryo.
- Sacralization mostly has no symptoms. It’s sometimes associated with low back pain with related problems of posture, and limited low back movement. It’s also called the lumbosacral transitional vertebrae (LSTV).
Anatomy related to Sacralization
- The lumbosacral joint is an articulation between the fifth lumbar (L5) and first sacral (S1) vertebrae.
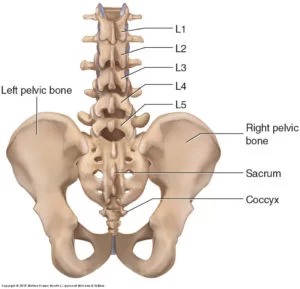
- The anterior intervertebral joint: a symphysis joint formed between the vertebral bodies of L5 and S1, separated by a large intervertebral disc and connected by vertebral ligaments.
- The facet joints: two zygapophysial joints formed between the articular processes of L5 and S1 vertebrae.
- Being inclined, the sacrum is connected with the fifth lumbar vertebra at an angle called the lumbosacral angle, which averages about 140°. The movements in this joint are limited to mostly flexion and extension, with a minimal amount of lateral flexion.
Movements
- The lumbosacral joint is the site of most movements of the lumbar spine. The movements occurring in this joint are mostly flexion and extension, and a minimal degree of lateral flexion. The degree of motion in the lumbosacral joint varies depending on age and individual characteristics.
- Before puberty, the lumbosacral joint accounts for about 75% of the total range of flexion and extension of the lumbar spine, which amounts to approximately 18°. The degree of lateral flexion is minimal and amounts to about 7° before puberty. The degree of these movements significantly decreases with age, especially after 35 years of age.
- Flexion is limited by the posterior part of the intervertebral disc and the ligaments of the vertebral column, namely the posterior longitudinal ligament, ligament Flava, interspinous and supraspinous ligaments. Extension of the joint is limited by the anterior longitudinal ligament, the anterior part of the intervertebral disc, and the close-packing of the facet joints.
Types of Sacralization
It has four main types, depending on the fusion seen on an X-ray, whether it is partial or total, and also depending on whether the fusion is on only one side (unilateral) or both sides (bilateral).
The most commonly used Castellvi classification is:
- Type 1: a fusion minimum of 19 mm in size with width on one (1a) or both sides (1b)
- Type 2: Partial fusion with a pseudo joint created on one side (2a) or both sides (2b)
- Type 3: full fusion of the L5 vertebrae to the sacrum on one side (3a) or the other (3b)
- Type 4: a combination of Type 2 and Type 3
Causes of Sacralization
- It occurs during embryonic development, when the vertebrae begin to ossify, in about the eighth week.
There may be a genetic predisposition involved.
There is not a proper statistic available that shows how many people have sacralization, mainly due to it being non-symptomatic. To diagnose this condition, imaging such as X-rays can help. You may not know you have this condition unless your doctor has other reason to X-ray of your back.
Symptoms of Sacralization
Mostly sacralization is non-symptomatic. If present following symptoms are seen:
- low back pain
- Arthritis at the fusion site
- bursitis
- disc degeneration
- difficulties in movement
- limits to the range of motion
- posture control problems
- scoliosis
- leg pain, buttock pain
Bertolotti’s Syndrome: When sacralization is associated with lower back pain, sciatica, and other related symptoms, it is called Bertolotti Syndrome. Symptoms of this condition usually appear in your 20s or 30s, such as:
- Lower back pain
- Back pain, stiffness, or difficulty moving
- Pain or discomfort in the back of your pelvis
- Pain is relieved when you sit or lie down.
- Muscle spasms only on one side
To diagnose Bertolotti’s syndrome, your doctor will require X-rays, a CT scan, and an MRI to check your lumbosacral joints. The doctor also examines you physically and does blood tests to rule out other related conditions and differentiate between them.
Incidence
The prevalence of sacralization in the general population has been estimated to range from 4 to 36 percent. The wide variation in estimations is a result of various diagnostic approaches and definitions.
An estimated 18.5 percent of people under 30 have sacralization.
According to a 2017 review, racial differences may exist in the incidence of sacralization. Studies cited in this analysis show incidences ranging from a low of 4% in China to 35.9% in Turkey.
Diagnosis of Sacralization
- Diagnosis based on the present history and clinical examination and confirmatory diagnosis done by x-ray, x-ray in lumbar flexion, and extension will be more beneficial to rule out.
- MRI provides a high-resolution image of your lower back.
Treatment of Sacralization
- Pain relief anti-inflammatory drugs (NSAIDs)
- muscle relaxants
- steroid injections
- Physiotherapy Treatment
Physiotherapy Treatment of Sacralization
Pain relieving modalities
- SWD: short wave diathermy is a deep heating modality that uses heat to provide pain relief, it improves the blood supply to targeted muscles, and removal of waste products.

- IFT: Interferential current therapy produces a low-frequency effect at targeted tissue, it inhibits transmission of pain impulses, stimulates the endogenous opioid system, increases blood supply, relieves oedema, and removes the waste products.
- TENS: transcutaneous electrical nerve stimulation is an electrical modality that provides pain relief by providing pain modulation.TENS closes the gate mechanism at the anterior grey horn in the spinal cord. also stimulates the endogenous opioid system which prevents the release of substance p at the anterior grey horn.
MOBILITY EXERCISE OF THE LUMBAR SPINE
Mobility Exercise of the low back will improve the mobility of the lower back
- KNEE TO CHEST :

- Lie on the back on the floor.
- Bend the knees, keeping both feet flat on the floor.
- Use both hands to pull one knee in toward the chest.
- Hold the knee against the chest for 5 seconds, keeping the abdominals tight and pressing the spine into the floor.
- Return to the starting position.
- Repeat with the opposite leg.
LOWER BACK ROTATION :
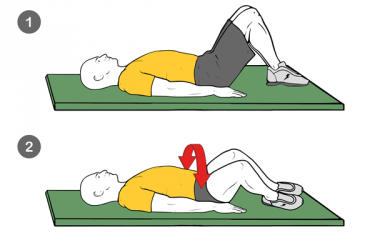
- Lie back on the floor with bent knees and feet flat on the ground.
- Keeping the shoulders firmly on the floor, gently roll both bent knees over to one side.
- Hold the position for 5–10 seconds.
- Return to the starting position.
- Gently roll the bent knees over to the opposite side, hold, and then return to the starting position.
PELVIC TILT EXERCISE
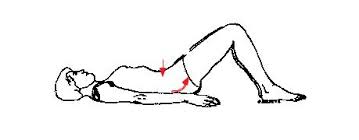
- The pelvic tilt is a beneficial exercise for your L5 vertebra. It reduces lower back pain by strengthening your abdominal muscles and inhibiting your lower lumbar para-spinal muscles.
- Lie on your back with your knees bent and your feet flat on the floor. Rest your hands on your pelvic bones on either side of your body. Contract your abdominal muscles and tilt your pelvis up to the ceiling by pressing your lower back into the floor. Release and repeat.
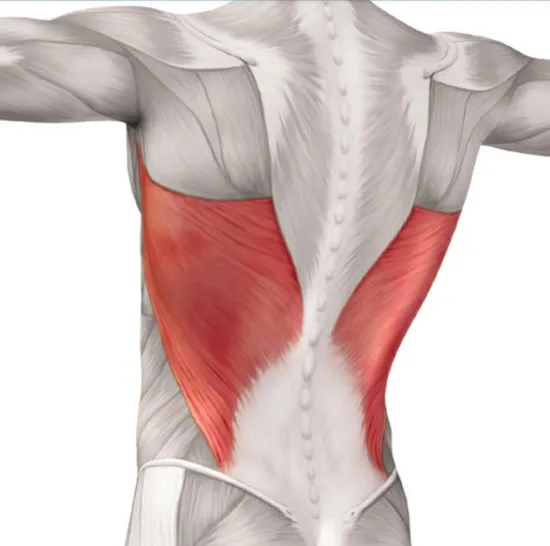
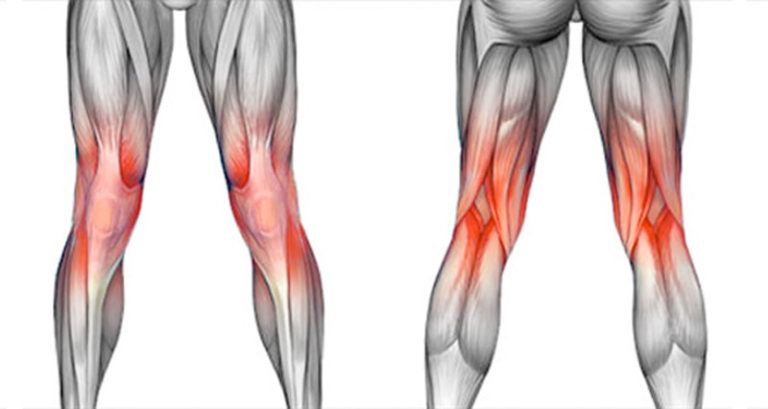
HAMSTRING STRETCHING :

- The hamstring stretch can help stabilize your lumbar spine. Lie on your back with your knees bent, keeping your spine in a neutral position.
- Raise your left leg into the air and straighten it by lifting your heel toward the ceiling. Hold your leg behind the upper thigh using both hands and gently pull the leg closer to your body. Hold the stretch for up to 30 seconds, then release and repeat on the opposite side.
Surgery
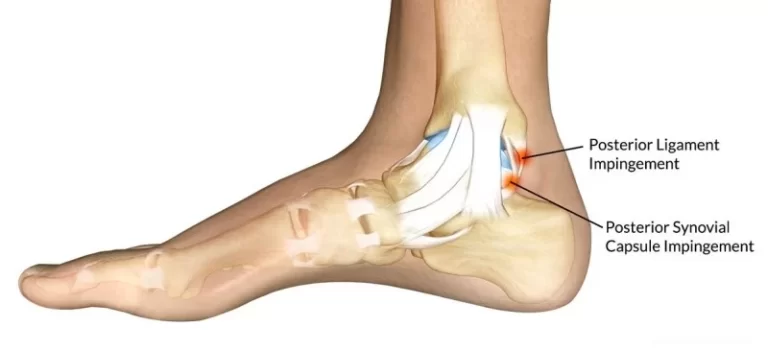
Surgery may be recommended to correct a specific disc or other problem created by the sacralization. Such as, Sacralization may cause extra strain on the disc between the 4th and 5th vertebrae, causing a slipped disc or early degeneration. It can also cause compression of the spinal nerve roots and pain in your spine, as well as referred pain in your legs, scoliosis, or sciatica.
Summary:
Sacralization is a common congenital spinal deformity that mostly has no symptoms. This condition may sometimes be associated with lower back pain and other related symptoms. If you have any pain or other related symptoms, conservative and surgical treatment options are available.
FAQs
What causes sacralization?
There is no particular cause for sacralization. It occurs during embryonic development, when the vertebrae start to ossify, nearly about the 8th week. There may be a genetic predisposition possible.
What does sacralization of L5 mean?
Sacralization is a congenital deformity in which the lowest lumbar vertebra (L5) becomes abnormally fused to the sacrum. The 5th lumbar vertebra (L5) may fuse fully or partially on one side or on both sides. Sacralization is a congenital anomaly that develops in the embryo.
How do you reduce sacralization?
Lifestyle modifications, such as avoiding activities that increase pain.
Pain-relieving medication, mainly non-steroidal anti-inflammatory drugs (NSAIDs),
Physical therapy treatment and exercises
Steroid injections to relieve symptoms
is the sacralization of l5 serious?
The sacralization of L5 refers to a condition where the last lumbar vertebra (L5) fuses with the sacrum, which is the triangular bone at the base of the spine. This condition is not necessarily serious, as it is a relatively common anatomical variation that affects about 4 to 5% of the population.
In most cases, sacralization of L5 does not cause any symptoms and does not require treatment. However, in some cases, it may be associated with lower back pain, sciatica, or other spine-related issues.






Nice article. Very informative.
Thank’s
Very very nice, clear informative and pictures are fantastic
Omg it helped me a lot. I’m suffering from a disc damage caused by this deformation, it’s so much pain everyday.
Very detail information.