Tibia Fracture
What is a Tibia Fracture?
The tibia which is also known as the shinbone, is the larger of the two bones in the lower leg. It’s one of the most common frequently fractured bones in the body.
Depending on the severity of your injury, the symptoms of a tibia fracture can range from bruising to excruciating pain in your lower leg.
What is a Tibia?
The long bone of the lower leg located medial to the fibula is called the tibia (shin bone). It is the second largest bone in the body after the femur, it also supports in the weight-bearing of the leg.
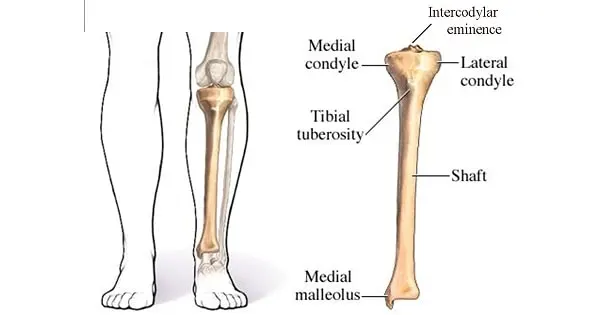
It contains 3 parts:
- Proximal, shaft, and distal.
- The proximal part helps in producing the knee joint.
- The distal part helps to produce the ankle joint.
- The tibial shaft
The proximal part:
The proximal part of the tibia forms the knee joint.
It contains:
- medial condyle
- lateral condyle
- intercondylar eminence
The shaft:
The shaft of the tibia is prism-shaped.
It has three borders and three surfaces; anterior, posterior, and lateral.
The distal part:
It includes,
The medial malleolus
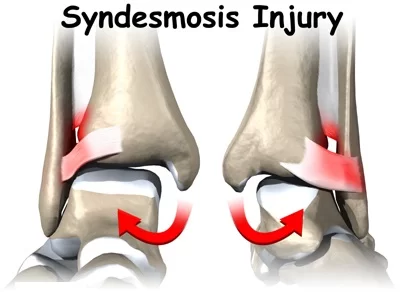
The fibular notch, where the fibula is bound to the tibia – forms the distal tibiofibular joint.
This part of the tibial helps in weight-bearing.
Causes of a Tibia Fracture
The most common cause of tibia fractures are:
High-energy trauma: It includes motorcycle or automobile accidents and can result in the most severe fractures.
Low-energy trauma: it includes fall which commonly results in elder patient
Twisting motions, such as pivoting: Sports such as snowboarding, skiing, and contact sports are common causes of this type of injury.
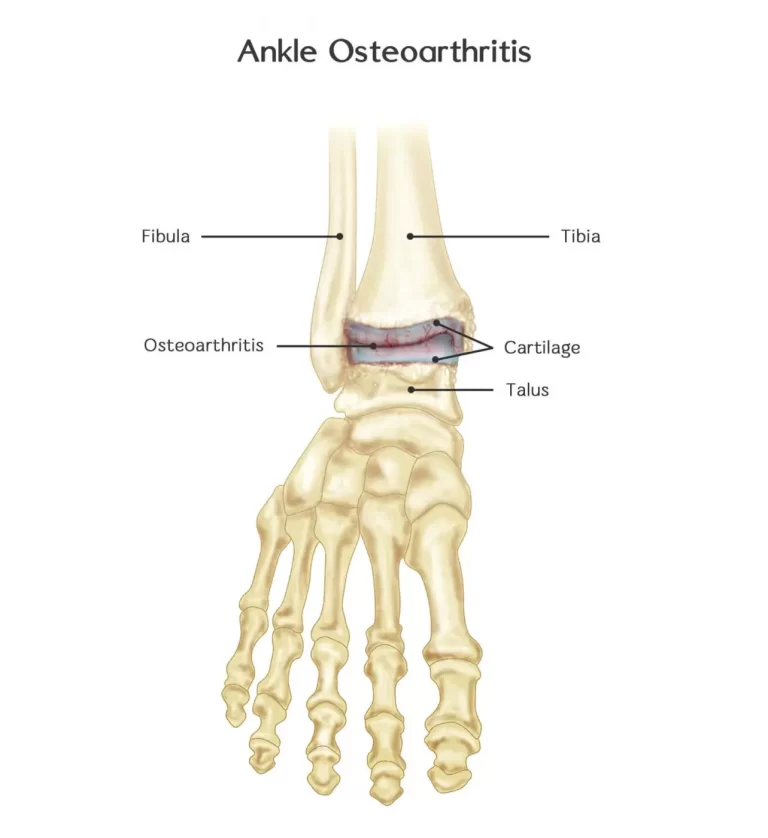
Health conditions may also affect your tibia fracture. It includes type 2 diabetes and pre-existing bone conditions such as osteoarthritis, osteoporosis, etc.
Symptoms of tibia fracture:
- Pain at fractured site
- difficulty in walking, running, or kicking
- numbness or tingling in the foot
- can not able to bear weight on the injured leg
- deformity in the lower leg, knee, or ankle area
- bone protruding through a skin break
- limited flexion of the knee
- swelling around the site of injury
- bruising and blueness on the injured leg
Types of Tibia Fracture:
Based on the cause of the fractured bone, the severity and type of fracture may vary.
- Stable fracture: In this type of fracture, bone is in the aligned position. The broken parts of the tibia maintain their correct position during the healing process. This is also called a non-displaced fracture.
- Displaced fracture: In this type of fracture bone fragments break in several fragments and are not in the aligned position. To correct this type of fracture and realign the bones back together surgery is needed.
- Stress fracture: This fracture is also known as a hairline fracture. It occurs due to overuse injuries.
- Spiral fracture: Due to twisting movement spiral fracture of the bone occurs.
- Comminuted fracture: When the bone breaks into three or more pieces, this is called a comminuted fracture.
Diagnosis of Tibia Fracture:
Medical history and physical examination:
The doctor will ask History of the patient which includes the type of injury and causes of injury. The doctor will also ask for any other medical condition, such as diabetes that the patient may be suffering and inquire about any medication that the patient might be taking.
Physical examination which includes checking for:
- Obvious deformity
- Skin breaks
- Bony protrusions under the skin
- Swelling
- Bruising
- Instability
- Sensations
- Muscle strength
Imaging test:
X-Rays: Most common test to diagnose fracture which provides a clear image of bones and helps to find out the location of fracture.
CT-Scan: If the doctor needs more information n after seeing an X-ray patient needs to undergo for CT-scan.
Treatment of Tibia Fracture
According to the types of fractures, treatment may vary.
There are two methods of treatment
- non-surgical method
- surgical method
Non-surgical treatment
Non-surgical treatment may be given to patients who have a closed fracture.
Initially, a splint may be provided for some support and comfort for your leg. Most tibia fractures involve significant swelling, and to reduce swelling the splint will be given to the patient
Once the swelling has reduces, casting and bracing may be given.
The fracture site needs to be immobilized in a cast for 6-8 weeks. After 6-8 weeks, the cast replaces with a removable brace. The brace keeps the fracture protected. The brace can be only removed during hygienic physical therapy sessions.
Brace:
The brace should not be worn at all times (day and night) placed fully straight for the first week after
surgery except when showering, or doing exercises.
Ice therapy
Start ice immediately after surgery.
Ice is applied for 20 minutes a minimum of four times daily, or more often if you prefer, but no more often
than 20 minutes every hour. To prevent frostbite be sure there is always something between the ice pack and your
skin and do not apply ice for longer than 20 minutes at a time.
Surgical treatment
Patients who have an open or comminuted fracture, or a fracture that is not fully healed following non-surgical therapy, may need surgical treatment.
Depending upon the location and severity of the fracture different methods are used.
- Internal fixation: In this method metal pins, plates, or screws are placed into the bone to keep the fractured ends aligned.
- External fixation: This surgery involves inserting metal pins or screws into the bone above and below the fracture location. The pins and screws are then attached to a bar outside the skin to give support.
- Intramedullary nailing: A long, straight metal rod is inserted from the knee into the center of the bone during this procedure to stabilize the bone.
Complications
Tibial fractures can cause other injuries and complications, including the following:
Broken bones frequently have sharp ends that have the potential to cut or tear the surrounding muscles, nerves, or blood vessels.
It’s possible to get acute compartment syndrome.
When the pressure in the muscles rises to dangerous levels, this painful condition develops. Blood flow can be impeded by this pressure, preventing nutrients and oxygen from reaching muscle and nerve cells.
To relieve pressure, your surgeon will cut holes in your skin and the muscle coverings during the procedure.
The bone is exposed to the outside environment by open fractures.
Complications from Surgery
- Infection
- Injury to nerves and blood vessels
- Blood clotting
- Malalignment of the broken fragments
- Delayed union or nonunion
- Angulation (with treatment by external fixation)
Physiotherapy Treatment
Initially, only full bed rest with Brace and an ice pack is used until the fracture is fully healed. Mostly Tibia fractures are healed within 6 to 8 weeks after that exercise will be started.
Tibia Fracture Rehab: Weeks 1-6
Your therapist will begin immediately with steps to decrease inflammation, reduce pain, and begin to facilitate healing.
To prevent further pain and re-injury the therapist focuses on maintaining knee extension and non-weight-bearing movement.
Exercises like active and passive movements of the knee and ankle are performed.
strengthening exercises like isometric exercise (static quadriceps exercise) perform.
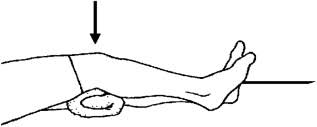
Static quadriceps exercise:
Lie on your back with your legs straight. Gently press the back of your knee flat against the ground. Hold for 10 seconds and release. Repeat 10 to 15 times.
Tibia Fracture Rehab: Weeks 6-12
The main goals at this point are to work with the patient to normalize gait without an assistive device.
initiate to regain full range of motion in the knee, and begin to strengthen the lower body.
progressive strengthening exercises may include squats, bridges, and straight leg raises.
weight bearing on the fractured leg will start from this stage
Squats:
Place your back flat against a wall or stand straight with your feet shoulder-width apart and your heels one and a half feet from the wall.
Try to place your knees directly above your heels.
Bend your back against the wall as you squat down, moving as low as you can pain-free, without dropping your buttocks below knee height. Make sure that your knees are placed in line with your heels. Press off of your heels to get back up.

Straight leg raises:
Make the quadriceps as tight as possible (similar to a quad set) While keeping your knee straight, raise your heel 4 to 6 inches off the ground. Maintaining as much tightness as possible in the quad, gently lower the leg back to the ground. Now unwind, take a brief break, and do it again.

Tibia Fracture Rehab: Week 12 – 6 Months
The goal at this point in physiotherapy is to achieve a full range of motion in the knee and to fully normalize your gait without any assistive devices.
Strengthening exercises for lower limbs like isometrics and progressive resisted exercises performed.
Tibia Fracture Rehab: 6-12 months
Non-athletes can return to their regular activities after 6 months.
Athletes will also initiate sports exercises such as plyometrics, unilateral exercises, and running on the treadmill for cardiovascular recuperation. It may take up to 12 months to fully return to sports.
Recovery
Recovery from a tibial fracture varies depending on the severity of the fracture.
A person will often heal within 4 to 6 months. Recovery time may be longer for a complete rupture compared to a partial one and may take longer if a person has poor health for other reasons.
Sometimes It may take a longer time for a person to be able to return to their normal activities. Patients have to follow their doctor’s suggestions about when to start walking, exercising, and engaging in other physical activities after a tibia fracture.
Certain exercises can help to take the stress off the tibia bone, such as exercises that strengthen the hips, calves, and thighs. protection such as a brace may also prevent future injuries from happening.
FAQs
What causes Tibia Fracture?
High-energy trauma: It includes motorcycle or automobile accidents and can result in the most severe fractures.
Low-energy trauma: it includes fall which commonly results in elder patient
Twisting motions, such as pivoting: Sports such as snowboarding, skiing, and contact sports are common causes of this type of injury.
Health conditions may also affect your tibia fracture. It includes type 2 diabetes and pre-existing bone conditions such as osteoarthritis, osteoporosis, etc.
What are the complications of the Tibia Fracture?
Infection
Injury to nerves and blood vessels
Blood clotting
Malalignment of the broken fragments
Delayed union or nonunion
Angulation (with treatment by external fixation
How long does recovery take?
Recovery time is based on the location and type of fracture.
A person will often heal within 4 to 6 months. Recovery time may be longer for a complete rupture compared to a partial one and may take longer if a person has poor health for other reasons.
What are the surgical methods for Tibia fracture?
Depending upon the location and severity of the fracture different methods are used.
Internal fixation: In this method metal pins, plates, or screws are placed into the bone to keep the fractured ends aligned.
External fixation: This surgery involves inserting metal pins or screws into the bone above and below the fracture location. The pins and screws are then attached to a bar outside the skin to give support.
Intramedullary nailing: A long, straight metal rod is inserted from the knee into the center of the bone during this procedure to stabilize the bone.
How long will it take to walk without any assistive device after Tibia fracture?
It takes 6-12 weeks to heal bones properly and for the structure of the knee to be stable sufficiently to start weight-bearing through the fractured leg.
After 6-12 weeks the patient can walk without an assistive device.





One Comment