ACL Avulsion Fractures
Introduction
An anterior cruciate ligament (ACL) avulsion fracture is a type of injury that involves the tearing away of a fragment of bone along with the attached ACL.
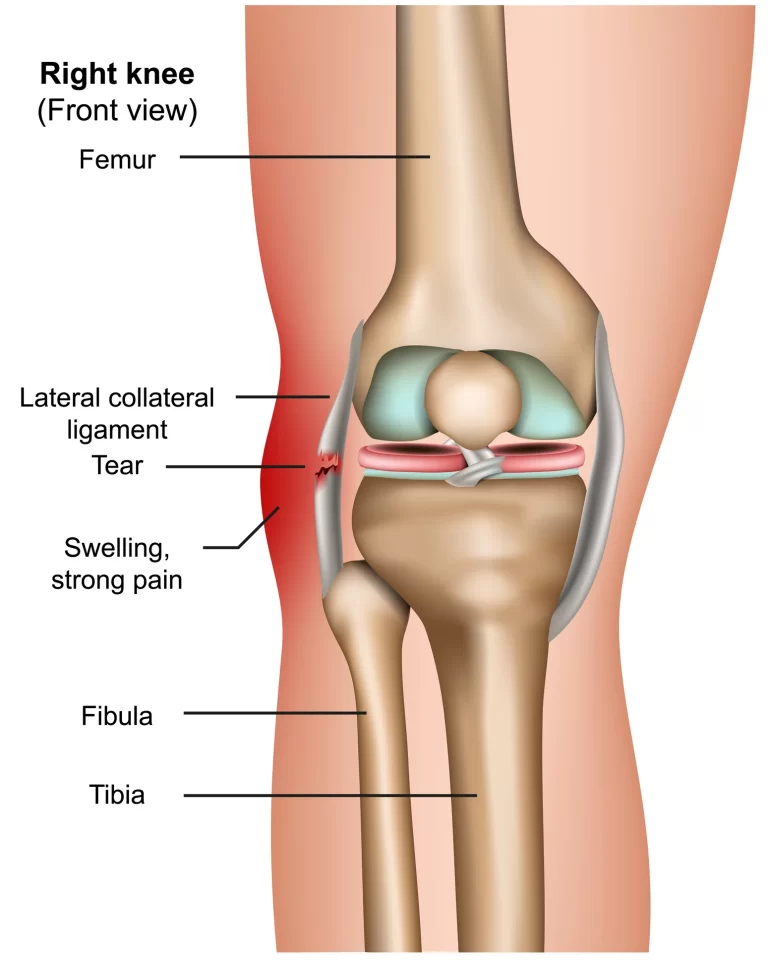
The ACL is a crucial ligament in the knee that helps stabilize and control the joint during various movements. When a significant force is applied to the knee, such as during a sudden twist or impact, the ACL may undergo excessive stress, leading to an avulsion fracture.
ACL avulsion fractures are most common in children and adolescents because their bones and growth plates are not fully hardened. The end of the femur and top of the tibia where the ACL attaches are areas of growth plate cartilage in youth. This cartilage is weaker than hardened bone. As such, during sports-related knee trauma, this is the most likely area for an avulsion fracture to occur.
Anterior cruciate ligament (ACL) tears are unfortunately a common knee injury, especially among athletes who play sports involving pivoting, jumping, and landing. The ACL is one of the key ligaments that stabilizes the knee joint. When the ACL is torn, the knee becomes less stable and more prone to “giving way” episodes. Additionally, an unchecked ACL tear can lead to further damage of the meniscus cartilage or articular cartilage over time.
One specific type of ACL injury is called an ACL avulsion fracture. This refers to when the ACL tears or peels away from the bone, pulling off a piece of bone with it. This occurs because the ACL attaches to the bones via Sharpey’s fibers. When enough tension builds on the ACL, these fibers can fail and a fragment of bone is torn away.
ACL avulsion fractures account for up to 7% of all ACL tears in the pediatric population. Prompt and accurate diagnosis is crucial, as these injuries can sometimes impair growth if treated poorly. Plain X-rays can usually confirm the diagnosis, while MRI can provide further details on displacement and anatomy. Most ACL avulsion fractures are treated surgically to restore the native anatomy and provide the best chance of recovery of ACL function.
In summary, ACL avulsion fractures are a subset of ACL tears where a fragment of bone is pulled away with the ligament. They require specialized treatment and consideration compared to other ACL injuries. Correct diagnosis and management are essential for regaining knee stability and allowing normal growth and development.
Causes of ACL Avulsion Fractures
The cause behind ACL avulsion fractures relates to the vulnerability of growth plate cartilage in children and adolescents. The growth plates, known as physics, are areas of softer, weaker cartilage at the ends of bones in youth. They contain actively growing tissue and osteoblasts that allow the bones to lengthen over time.
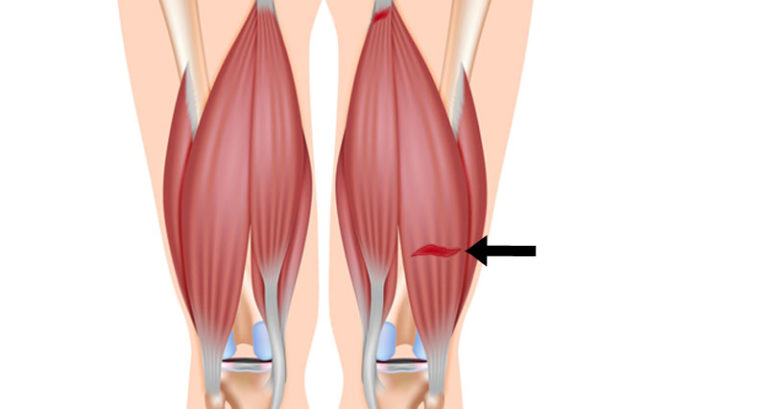
In particular, the distal femoral physis and proximal tibial physis are prone areas at the knee joint. During forceful rotational movements, the strong native ACL can essentially tear straight through this growth cartilage, pulling away a bone fragment in the process. This creates an ACL avulsion fracture.
The types of movements that can lead to avulsion fractures are similar to typical ACL tears – sudden changes in direction, landing from a jump and hyperextending the knee, pivoting while running, or sudden deceleration. The magnitude of the force on a relatively weak physis exceeds the tensile strength of the Sharpey fibers that anchor the ACL to the bone.
Epidemiology
ACL avulsion fractures are quite rare, accounting for less than 1% of all physical fractures. However, among prepubescent children with ACL tears, ACL avulsion fractures represent up to 7% of occurrences.
These injuries occur in a bimodal distribution – first in young children aged 8-12 years old who are still growing, and secondly in older teenagers aged 15-19 years who are nearing skeletal maturity.
Younger children are the most vulnerable because their growth cartilage and physiques are thicker and weaker. Older adolescents begin to ossify and their cartilage becomes thinner, but they are also stronger and faster, able to generate higher magnitudes of force during sports.
Males appear to be affected approximately 3 times as often as females across most age groups. This is thought to relate to differences in neuromuscular control, landing biomechanics, and rate of skeletal maturation during puberty. Certain female hormones may provide some protective effects.
ACL avulsion fractures mainly occur because of the vulnerability of growth plate cartilage in the youth of a certain age range. Forceful, rapid loading of the knee joint generates tensions that exceed the strength of the physis. These fractures represent a small but important subset of ACL tears in children and adolescents.
Pathophysiology
The pathophysiology of ACL avulsion fractures relates to the process of how the ACL tears directly through the weaker growth plate cartilage in the knee joint of children and adolescents.
As background, the distal femoral and proximal tibial physis contain growth plate cartilage that allows lengthening of the bones. In contrast, the native ACL ligament is a very tough and fibrous tissue that anchors to bone through Sharpey’s fibers.
When a large rotational force is applied across the knee, the strong ACL can generate tensile forces exceeding the strength of the bone-ligament interface. In particular, the physeal cartilage tissue fails before the Sharpey’s fibers or ACL fibers themselves.
A bone fragment at the end of the femur or top of the tibia is then ripped away as the ACL tears through the cartilage. This leaves a defect of exposed bone still attached to the ACL itself, with associated bleeding and inflammation. MRI scans clearly show the avulsed bony fragment.
Mechanism of ACL Avulsion Fractures
The precise mechanism relates to the direction of force that tears the ACL. Two main mechanisms predominate:
1. Hyperextension Injuries
Forced hyperextension of the knee creates anterior translation of the tibia. This stretches the ACL beyond capacity. The posterior aspect of the ACL attachment site fails as the physis fractures.
2. Tibial Rotation Injuries
Aggressive inward rotation of the tibia (towards the body midline) increases strain on the ACL. The anterolateral aspect of the ACL attachment site fails as the physis fractures.
Excessive quadriceps contraction or hamstring deficiency may contribute to these mechanisms. Landing from a jump or rapid changes in direction during pivoting sports are common inciting events, as dynamic play generates substantial multiplanar knee forces.
Avulsion fractures mainly occur due to tensile overload of the ACL-bone interface as aggressive youth sports generate knee hyperextension or tibial rotation. The pathophysiology demonstrates why the weaker physeal cartilage fails first, avulsing a bone fragment.
Physical Examination
The physical exam of an acute knee injury suspected to be an ACL avulsion fracture will share features common to other ACL tears, with some additional key findings specifically suggesting a bony fracture.
Inspection of the knee may show swelling, bruising, or joint effusion indicating internal derangement. Palpation around the joint lines should be assessed for point tenderness. Compare symmetry to the uninvolved knee.
Assess knee range of motion both actively and passively – significant limitations in extension suggest a bony block to motion. Gently test ligamentous stability at 30 degrees of flexion using the Lachman test (anterior translation of the tibia), varus/valgus stress tests, and posterior drawer test.
A positive Lachman with a soft or mushy endpoint suggests ACL insufficiency. Concurrent clicking or catching during the range of motion can indicate a bone fragment or loose body in the joint.
Evaluation
Imaging confirms the diagnosis with further details:
- Plain X-rays can directly visualize avulsion fractures and detect loose fragments or blocks of motion. Comparison views of the uninjured knee are useful.
- MRI precisely images soft tissue and bone. It depicts edema patterns, disruption of the ACL fibers, exact location of bony fragments, and associated injuries (meniscus, cartilage, etc).
Sometimes MRI performed too early may miss very subtle fragments. Repeat advanced imaging in 10-14 days clearly shows the injury after some healing and resorption of blood products.
CT scans can provide enhanced detail of fracture anatomy when surgical decision-making depends on precise fragment size, displacement, comminution, and bone stock.
Thus clinical examination combined with advanced imaging diagnoses ACL avulsion fractures. MRI gives the greatest insight into soft tissue trauma patterns while CT better defines subtle bony detail.
Treatment of ACL Avulsion Fractures
Initial Nonoperative Treatment
- First-line treatment for most acute, non-displaced avulsion fractures without other complications involves attempting closed reduction of the fragment and joint. This is done via manipulation and splint/cast application in anatomic alignment.
- Initial immobilization protects injured structures while limiting pain and muscle spasms that displace fragments. The position also relaxes deforming muscle forces.
- Non-weight-bearing and ice application reduces inflammation and discomfort. NSAIDs help control pain as well.
- Frequent radiographic follow-up, even weekly initially, is key to ensure maintenance of reduction throughout healing. Repeat attempts at closed reduction may be required for early displacement.
- Range of motion is restricted initially depending on the location and forces acting on the injury. The protocol is loosened gradually based on clinical and radiographic evidence of healing over 6-12 weeks.
Indications for Surgery
- Open fractures require urgent debridement, irrigation, and fixation to prevent infection risk
- Incarcerated fragments must be extricated and fixed if unable to be reduced by closed means
- Any signs of neurovascular compromise like compartment syndrome necessitate immediate decompressive surgery
- Gross instability causing recurrent dislocations or functional impairment needs stabilized fixation
- Locations like the quadriceps tendon have high muscular distraction forces and will not heal without surgical intervention
- Tenting, blanching, or dusky skin over fragments may lead to necrosis and require removal of pressure
Goals of Surgery
- Anatomic open reduction and rigid internal fixation prevent nonunion and malunion
- Restoring articular surface smoothness lessens the risk of post-traumatic arthritis
- Fixation and soft tissue repair provide static and dynamic stability to enable motion
- Earlier rehabilitation is possible compared to nonoperative care
- Lower risk of stiffness, weakness, gait abnormalities, chronic pain, osteoarthritis
Techniques Include:
- Screw fixation for large, reducible fragments with bone stock
- Suture anchors or transosseous sutures for small or comminuted fragments
- Excision of fragments only if severely comminuted or inadequate bone stock
- Possible primary arthrodesis for some joints if chronic instability is inevitable
- Soft tissue augmentation procedures for ligamentous/capsular laxity
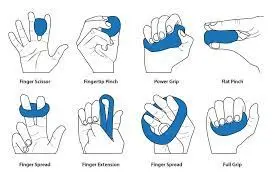
Rehabilitation Principles
- Initial protection of fixation and modulated immobilization balanced with preventing stiffness
- Gentle passive and active assisted range of motion exercises start early, within tolerance
- Muscle strengthening is usually delayed until adequate bone healing and stability achieved
- Functional training progresses from basic to sport-specific activities as the patient demonstrates readiness
- Return to play based on clinical milestones and radiographic bone healing, not simply time
The detailed and comprehensive treatment of avulsion fractures encompasses appropriate initial reduction, selecting surgical technique based on presentation, methodical follow-up for complications, and progressing activity based on healing phases to return patients to full function.
Physical therapy rehabilitation
Phase 1 (0-2 weeks after surgery)
Goals:
- Protect graft fixation
- Control inflammation and pain
- Prevent muscle inhibition
- Restore full knee extension
- Initiate quadriceps activation
Treatment:
- Brace locked in extension, transition to gentle PROM exercises
- Patellar mobilizations if lacking full knee extension
- Cryotherapy, electrical stimulation for swelling, and pain control
- Quadriceps sets and NMES to prevent a shutdown
- Gait training with crutches, and weight-bearing as tolerated
Phase 2 (2-6 weeks)
Goals:
- Single-leg standing without compensation
- Normalize gait mechanics
- Quad and hamstring strength to 60% function
- Increase knee ROM to 0-90 degrees
Treatment:
- Open brace to 90 degrees as quad control improves
- Progress squat range and closed kinetic chain exercises
- Blood flow restriction training for quad hypertrophy if poor control
- Initiate proprioception: single leg balance with support
- Normalize gait, wean off crutches
Phase 3 (6-12 weeks)
Goals:
- Single leg squat strength >70% uninvolved side
- Stride length and symmetry normalized
- Hop tests >70%, quad strength >80% of uninvolved
- Cardiovascular endurance recovery
Treatment:
- Open brace, continue vigorous strengthening
- Perturbation training response
- Balance on unstable surfaces
- Impact control exercises: jump downs, lateral hops
- Stationary bike, treadmill, swimming
Phase 4 (>12 weeks)
Goals:
- Quad strength >90% uninvolved
- Hop tests showing <10% limb symmetry deficit
- Neuromuscular control and dynamic knee stability
- Confident cutting motions and landing mechanics
Treatment:
- Sport/activity-specific agility drills
- Multiplane plyometrics
- Gradual return to sports program based on functional criteria
- Maintenance strength and flexibility program
Thus rehabilitation progresses across phases based on graft healing constraints to safely return to high-level function. Periodic re-evaluation determines patient advancement.
Prevention
While contact ACL injuries cannot always be prevented, several factors may reduce the risk of non-contact ACL tears and associated avulsion fractures:
- Neuromuscular training programs: Exercises focusing on body control, balance, plyometrics, and strengthening help optimize muscle recruitment patterns and joint positioning. This stabilizes the knee dynamically during athletic maneuvers.
- Encouraging soccer and basketball athletes to use proper landing mechanics and minimize excessive valgus stress can protect the ACL.
- Bracing: Prophylactic knee braces may prevent some ACL injuries, especially in athletes with previous ACL reconstructions, by resisting tibial internal rotation and anterior translation forces. However, bracing acceptance is low.
- Identifying and correcting modifiable risk factors: Lower extremity anatomic variations, muscle imbalances, core weakness, and lower limb malalignment can increase ACL strain. Addressing deficits may reduce injury risk.
- Education on unsafe movements: Coaching proper pivoting, cutting, and landing techniques minimizes risky knee positioning. Reducing fatigue and being aware during peak injury risk scenarios protects the ACL.
Differential Diagnosis
The key differential diagnoses to consider when evaluating a suspected ACL avulsion fracture include:
- Segond Fracture – This refers to the avulsion of the lateral capsular ligament complex of the lateral tibial plateau. It is pathognomonic for an ACL tear but must be distinguished from ACL bony avulsions.
- Meniscus Tear – Complex meniscus tears often occur in combination with ACL rupture. Signs include joint line tenderness, catching/locking of the knee, and limited range of motion. MRI distinguishes this.
- Patellar Dislocation – An acute knee injury with findings of effusion and patella alta on x-ray should prompt evaluation for possible transient patellar dislocation. This can occur in isolation or concurrently with ACL/patellar tendon trauma.
- Tibial Eminence Fracture – Avulsion of the ACL from its tibial attachment in the intercondylar notch may be confused with tibial spine fractures. Careful evaluation of fracture pattern and displacement is needed.
- Patellar Tendon Rupture – Distal patellar tendon avulsions may have a similar presentation to ACL avulsions but have distinct MRI findings. The continuity of the quadriceps mechanism must be assessed.
Prognosis
With appropriate diagnosis and treatment, the prognosis for ACL avulsion fractures is generally good. However, several factors influence patient outcomes:
- Open physics – Growth disturbance is a risk if surgical fixation is not anatomic. Repeat MRI at maturity can assess for growth arrest.
- Articular incongruity – Malreduction may accelerate degenerative joint changes. Even 1-2 mm offsets lead to poorer function.
- Chondral/meniscal damage – Concurrent cartilage or meniscal pathology predicts worse outcomes and higher reoperation rates. This is assessed with MRI and arthroscopy.
- Limb malalignment – Existing lower extremity malalignment increases loads on the ACL graft, placing the patient at higher risk of recurrent rupture or instability symptoms.
- Patient activity level – Outcomes are superior with strict adherence to rehabilitation protocols. Highly competitive athletes have higher re-injury rates than less active patients.
Thus, the prognosis after ACL avulsion fracture is good with primary surgical repair but requires careful assessment for associated injuries and anatomical risk factors that may predispose patients to worse function or failed stability.
Summary
ACL avulsion fractures are an uncommon subset of ACL ruptures accounting for up to 7% of pediatric knee injuries. The ACL can tear straight through the weak growth cartilage in the distal femur or proximal tibia of young athletes, pulling away a bone fragment in the process. These fragments must be reduced to prevent growth disturbance and preserve knee stability.
Presentation is similar to acute ACL tears but also includes findings suggestive of an intra-articular fracture like clicking, catching, or knee extension blocks. Imaging confirms the diagnosis, while MRI gives the greatest insight into fracture displacement and associated soft tissue trauma.
The first line of treatment is surgical fixation to restore anatomy and ACL function. Various techniques cater to the specifics of the injury and the patient’s skeletal maturity. Early protected weight-bearing and rested range of motion is initiated post-operatively. Rehabilitation advances in phases depending on clinical and radiographic evidence of healing. If diagnosed and managed appropriately, outcomes are generally good and the native ACL can be preserved. However, growth arrest, poor fracture reduction, existing limb malalignment, concomitant injuries, and high activity levels predict a worse prognosis. Prevention focuses on neuromuscular training, technique coaching, bracing, and correcting biomechanical deficits.
FAQs
How are ACL avulsion fractures diagnosed?
Careful history, physical exam, and plain radiographs provide initial suspicion. MRI precisely depicts fracture displacement, ACL tear location, and associated injuries, and guides treatment planning. CT better defines subtle bony detail
What are the goals of surgery for ACL avulsion fractures?
The goals are restoring articular congruity, fixing displaced fragments, dynamically stabilizing the ACL tear, regaining early motion, enabling accelerated rehabilitation, and preventing complications like nonunion.
What prevents a successful return to sports after surgery?
The most common causes are graft failure from non-anatomic fixation, untreated associated injuries, underlying malalignment, poor rehabilitation compliance, returning too early before regaining muscle strength, and inadequate neuromuscular control with pivoting/cutting.
How long until young athletes can return to sports post-operatively?
Timelines are highly individualized and based on clinical criteria rather than a rigid timeframe. For pre-adolescent children, at least 6 months is advised with repeat MRI assessing physical status. Adolescents require 9-12+ months for graft incorporation with the maintenance of symmetry on functional testing.
REFERENCES
- McCoy, J. S. (2023, August 7). Avulsion Fractures. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK559168/
- Anterior Cruciate Ligament (ACL) Injury or Tear. (2021, November 16). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/acl-injury-or-tear
- Annemarie, B. A. S. E., Louren, G. L. M., & Jos, V. R. J. J. A. M. (2020, April 1). An avulsion fracture of the anterior cruciate ligament attachment to the lateral femoral condyle in an elderly patient: a rare finding. Journal of Surgical Case Reports. https://doi.org/10.1093/jscr/rjaa054