Swollen Feet with Diabetes
Introduction
If you have diabetes, you may sometimes notice your feet becoming swollen or puffy. This swelling, medically known as edema, occurs when excess fluid accumulates in the tissues of your feet and ankles. Although occasional minor swelling can happen to anyone, having persistently swollen feet with diabetes is a problematic sign that needs medical attention.
When high blood sugar from uncontrolled diabetes starts damaging the blood vessels and nerves in the legs and feet, it impairs circulation in the lower limbs. Fluid can then readily build up and pool around the feet and ankles.
If left unmanaged over an extended period, this diabetic swollen foot condition can progress and lead to dire health repercussions – from skin infections to foot ulcers, nerve issues, and even amputation in worst cases!
What Causes Swollen Feet with Diabetes?
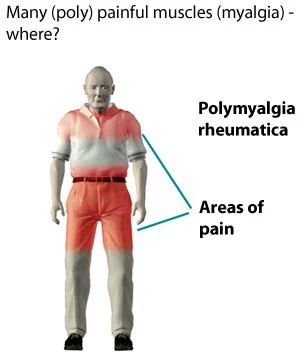
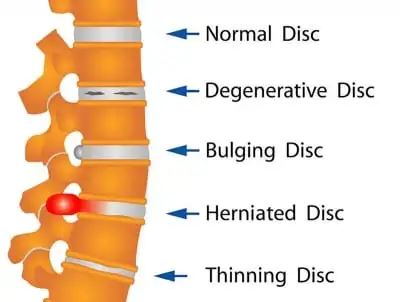
In people with diabetes, high blood sugar levels can damage the blood vessels and nerves in the legs and feet over time. This nerve damage (neuropathy) can make it hard to notice small foot injuries. Additionally, damaged blood vessels struggle to pump enough blood and fluid back up the legs.
Gravity then causes fluid to gather and leak out of capillaries into the lower extremities, resulting in swelling around the feet and ankles. Reduced circulation can also make feet appear reddened or inflamed.
- Over time, blood vessels and nerves are harmed by high blood sugar levels. Uncontrolled blood sugar can cause neuropathy and blood vessel issues in the legs and feet.
- Poor circulation and blood flow to the lower extremities. Compromised blood vessels cannot adequately pump blood and fluid back up to the heart. This results in pooling of fluid in the feet and ankles.
- Fluid leakage from capillaries into surrounding tissues. When small blood vessels in the feet are damaged, fluid leaks out into nearby tissues leading to swelling localized in the feet and ankles.
- Kidney damage from diabetes (diabetic nephropathy). If the kidneys are affected by diabetic complications, excess fluid cannot be properly filtered out. This excess fluid retention can cause generalized swelling including foot and ankle edema.
- Nerve damage in the feet (peripheral neuropathy). Neuropathy prevents the nerves in the feet from properly signaling the brain. This makes it difficult to sense pain, temperature changes, or injuries, which can all worsen foot swelling.
- Being overweight or obese. Excess weight applies additional pressure on the feet which can aggravate swelling. It also reduces circulation and compounds existing blood vessel issues.
In summary, the underlying causes of swollen feet stem from elevated blood glucose levels that eventually weaken blood vessels and nerves. This then leads to poor circulation, fluid retention, and nerve issues specifically isolated in the feet area. Keeping diabetes under control is key to preventing and managing these complications.
Signs and Symptoms
- Visible swelling in the feet and ankles may cause shoes, socks, or pants to feel too tight. Swelling is often more noticeable late in the day. Check for pitting edema by pressing gently on the skin to spot fluid build-up.
- Reddened or inflamed-looking feet – this can indicate circulatory issues or cellulitis skin infection which requires urgent care. The skin may appear shiny, warm, and tender.
- Tingling or numbness in the feet (diabetic neuropathy) – nerve irritation or damage can cause prickling pins and needles sensations or complete loss of sensation. This greatly raises injury risk.
- Skin cracks, blisters, or dryness around ankles and heels can worsen with swollen feet in shoes. This skin damage provides openings for bacteria to cause infection.
- A feeling of tightness or heaviness in the lower legs and calves due to fluid accumulation and decreased circulation. Leg cramps at night may also occur.
- Visible denting, pitting, or skin discoloration – apply gentle pressure on the swollen area for several seconds and observe if it leaves an indentation. Skin may appear darkened or purplish.
- Decreased ankle flexibility and mobility due to stiffness and fluid buildup around joint areas.
- Leg fatigue, tired muscles, or achiness that is relieved by rest and elevating the legs which aids gravity drainage.
Seeking timely treatment for swollen feet is crucial for people with diabetes. Catching it early not only manages swelling but also helps prevent major diabetic complications in the lower limbs going forward.
If you notice fluid retention and swelling around the feet and ankles, with or without discoloration or skin indentations, check in with your doctor. Diabetic swollen feet should not be ignored.
Potential Risks and Complications
Skin Infections
- Bacterial infections like cellulitis
- Fungal infections like athlete’s foot
- Swollen feet create moist areas prone to microbial overgrowth. Cracks in the skin also raise infection risk.
Foot Ulcers
- Damaged skin tissues usually over areas of high-pressure
- Slow healing of wounds due to poor circulation
- Can worsen rapidly without proper treatment
Gangrene
- Death of body tissues from extensive infection or lack of oxygenated blood
- It begins with small areas but can spread across the feet if unchecked
- May ultimately require amputation to avoid systemic infection
Diabetic Foot Problems
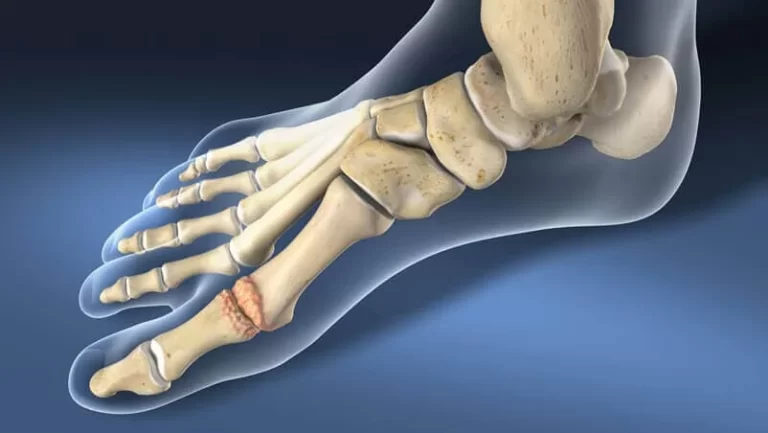
- Charcot foot changes the foot’s shape due to neuropathy
- Hammer toes and bunions arise over time requiring surgery
Loss of Limb Sensation
- Worsening neuropathy means injuries, wounds or objects in shoes can go unnoticed
- Increases risk of falls or unnoticed joint damage
Reduced Mobility
- Swelling and tenderness can limit activity levels long term
- Increases risks of blood clots due to prolonged sitting/non-movement
As the risks above demonstrate, the complications stemming from diabetic swollen feet can be severe, from non-healing foot ulcers to limb amputation. However, diligent foot care and working closely with your podiatrist can successfully lower these risks and catch foot issues early. Controlling blood sugars also helps slow the advancement of neuropathy and circulatory impairment underlying these complications.
Caring for Your Feet
While swollen feet can happen sporadically, they can often be prevented through healthy daily foot care and lifestyle habits:
- Check blood sugar levels routinely and keep them under control through medication or insulin adjustment with your doctor. High blood sugar can contribute to foot swelling.
- Examine your feet every day; if necessary, use a mirror. Look for any cuts, blisters, red spots, or swelling, and contact your doctor if you observe any changes or abnormalities.
- Wash feet in lukewarm water, using gentle soap. Dry everything completely, including the spaces between your toes.
- Apply lotion on feet while avoiding spaces between the toes – moisture can lead to infection.
- Trim toenails straight across to prevent ingrown nails. Seek guidance from your podiatrist or doctor for trimming.
- Wear clean, properly fitted socks and shoes. Ensure adequate wiggle room for toes.
- Exercise regularly to improve circulation. Move ankles up and down and take short walks periodically if sitting for long periods.
- Elevate swollen feet on a stool when possible to improve drainage.
- Lose excess weight through dietary changes and exercise under your doctor’s care. Extra weight puts pressure on feet.
See Your Doctor
Schedule an appointment if you notice persistent swollen feet for several days, with or without pain. Seek urgent care if you observe red skin, wounds, numbness, tingling, or your feet turning blue – these require immediate medical attention to prevent complications.
Your doctor can evaluate your symptoms, adjust medications impacting swelling, provide foot care advice, and refer you to a podiatrist if needed for foot-related complications. Custom shoes and orthotics may be prescribed to alleviate swelling. Ongoing foot care is key for people with diabetes!
Treatment
Control Blood Sugar Levels
- Check glucose levels routinely through finger sticks and A1C blood tests
- Stick closely to your medication regimen or insulin schedule
- Maintain better sugar control to prevent vessels and nerve damage
Proper Foot Care
- Clean feet daily and use moisturizer to prevent skin cracks
- Inspect feet and look in between the toes for any wounds or red areas
- See a podiatrist regularly for check-ups, calluses removal, potential orthotics
Exercise and Stretching
- Low-impact activities like walking, swimming, stationary bike to boost circulation
- Stretching, yoga, ankle rolls to ease stiffness and increase mobility
Elevate Legs
- Lie down and raise your feet slightly above the heart level for 30 minutes daily
- Use pillows for elevation when sitting or sleeping
Diuretic Medications
- Water pills (diuretics) rid the body of excess fluid through increased urination
- Help reduce general or isolated limb swelling
Compression Stockings
- Special stockings to provide gradient pressure improving venous circulation
- Reduce pooling of fluid in feet and legs
Lose Extra Weight
- Consult your doctor to develop a supervised diet and fitness plan
- Gradual weight loss minimizes pressure and strain on the feet
Avoid Constipation
- Straining to pass hard stools applies unwanted and unsafe abdominal and foot pressure
Surgery
- Angioplasty to improve blood flow to the lower limbs
- Amputation if gangrene tissue develops, to avoid septicemia
The above treatments focus on alleviating existing swollen feet while also targeting the poor circulation and high blood sugar causing the swelling. A combination approach works best through the coordinated efforts of one’s medical team.
Prevention
Check Blood Sugars Routinely
- Monitor glucose levels through regular finger stick tests and A1c lab tests
- Keeping blood sugars controlled prevents vessel and nerve damage over time
Inspect Feet Daily
- Look for any wounds, blisters, edema, or redness.
- Especially inspect between the toes and bottom of the feet
- Use a mirror to see all areas if needed
Proper Foot Hygiene
- Especially in between the toes, properly wash and dry your feet.
- Apply moisturizing lotion daily, avoiding spaces between toes
- Soak feet in warm water then scrub with a soft towel to increase circulation
Trim Toenails Properly
- Trim toenails evenly to avoid uncomfortable ingrown nails
- Seek guidance from a podiatrist on proper trimming
Wear Properly Fitted Footwear
- Shoes that are too tight can worsen swelling
- Ensure adequate room for toes without too much space
- Consider custom orthotics or special diabetic shoes
Exercise Regularly
- Low-impact activities like walking, swimming, cycling
- Helps stimulate blood flow to feet and prevent stiffness
Lose Excess Weight
- Consult your doctor to develop a healthy diet and fitness plan
- Gradual weight loss reduces foot pressure and strain
Elevate Your Feet
- Rest feet slightly above the level of the heart for 30 minutes daily
- Try with pillows under the feet or legs elevated when sitting
Avoid Ankle Crossing
- Keep ankles uncrossed whenever seated to allow proper circulation
Summary
Diabetes can sometimes lead to swelling, or edema in the feet and ankles, which if left unchecked can cause major complications. The swelling stems from high blood sugar damaging blood vessels and nerves over time. This impairs circulation and causes fluid build-up in lower limbs.
Swollen feet signs like skin discoloration, numbness, and skin infection risks should never be ignored. They require urgent medical care to heal tissue damage and prevent issues like foot ulcers or gangrene. With consistent blood sugar control and diligent at-home foot care under a doctor’s guidance, patients can successfully manage swelling or even avoid episodes altogether.
Treatment options range from daily cleaning and elevating feet to special shoes, medications, and even surgery for enduring cases. Create a personalized plan with your healthcare provider addressing both the swelling itself and the poor circulation triggering it. Consistent self-care paired with empowering lifestyle changes makes all the difference in negating the risks of diabetic swollen feet.
FAQs
Are swollen feet common with diabetes?
Yes, foot and ankle swelling are common occurrences with diabetes, resulting from internal blood vessels and nerve impairment over time.
Can I make lifestyle changes to reduce swelling?
Yes, daily exercise, frequent foot inspection regimes, wearing appropriate footwear, and losing excess weight can all help minimize swelling episodes.
When should I urgently contact my doctor about swelling?
Seek urgent medical care if you have excessive swelling for over 2 days without relief, or if you notice redness, skin wounds, numbness, or skin color changes, which indicate infection or nerve damage.
Can diabetic swollen feet be cured permanently?
While aggravating factors can be controlled, the blood vessel and nerve damage is lifelong. However, sticking to treatment plans dramatically reduces the occurrence of severe swelling and prevents the progression of foot complications long term. Consistency is vital.
What role does my blood sugar have in my swollen feet?
High blood sugar levels directly damage soft tissue over the years. In the feet, nerves and tiny blood vessels get destroyed over time. This process underlies swelling and must be continually managed through sugar testing, diet, exercise, and medications if needed.
How long until I see my swelling subside through treatment?
With comprehensive treatment, most will see some swelling relief within 1-2 weeks as circulation, blood flow, and structure pressure on the feet improve. But foot health needs consistent lifelong self-care.
References
LeBrun, N. (2022, September 21). Can Swollen Feet Be a Symptom of Diabetes? Verywell Health. https://www.verywellhealth.com/diabetes-and-swollen-feet-6503070
Higuera, V. (2023, October 17). 10 Tips to Treat Swollen Feet from Diabetes. Healthline. https://www.healthline.com/health/diabetes/diabetes-swollen-feet
Fletcher, J. (2023, February 14). How can diabetes affect the feet? https://www.medicalnewstoday.com/articles/317504
Burns, A. (2022, January 5). Can diabetes cause swollen feet? Arizona Foot Doctors. https://arizonafootdoctors.com/swollen-feet-and-ankles-diabetes/