Bunions
What is a Bunion?
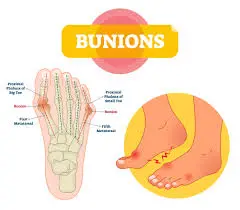
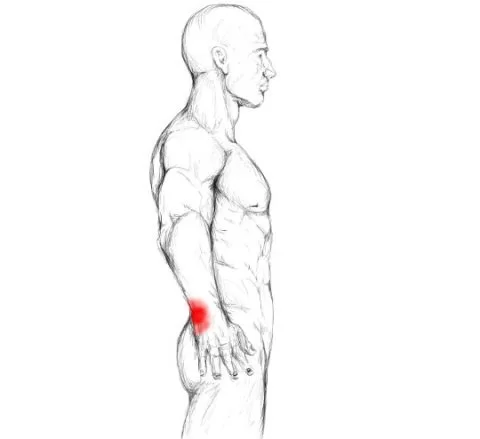
A bunion, medically known as hallux valgus, is a painful and unsightly bony protuberance that typically forms on the inner side of the foot, specifically at the joint of the big toe. Bunions often result from the gradual misalignment of the big toe, causing it to drift towards the smaller toes and the outer edge of the foot.
The discomfort associated with bunions arises primarily from the friction and pressure exerted by footwear on the prominent bony bump and the neighboring toes. This pressure, coupled with the altered mechanics in the front part of the foot, can lead to pain and discomfort.
The development of bunions is usually a slow and progressive process. The big toe joint experiences constant pressure, causing it to deviate from its normal position. Over time, this leads to changes in the alignment of bones, tendons, and ligaments, ultimately resulting in the characteristic bunion deformity. This deformity tends to worsen gradually and can make wearing shoes or walking painful and challenging.
Bunions tend to affect women more frequently than men. Remarkably, around 70% of individuals who develop bunions have a family history of the condition, highlighting a strong genetic predisposition. This genetic link is particularly evident in cases of adolescent bunions, which may manifest early in life. While most bunions develop during adulthood, there is a possibility that repetitive micro-trauma, such as wearing shoes with high heels and narrow toe boxes, can contribute to their formation.
In most instances, bunion-related pain can be alleviated by opting for wider shoes that provide adequate room for the toes. Additionally, various simple treatments can help reduce pressure on the big toe and offer relief. However, in cases where pain persists despite conservative measures, surgical intervention may be necessary to correct both the bunion and the associated hallux valgus deformity.
Anatomy of Bunions
The big toe consists of two key joints, with the larger of the two being the metatarsophalangeal joint (MTP), where the initial long bone of the foot (the metatarsal) connects with the 1st toe bone (the phalanx).
Bunions form at the MTP joint.
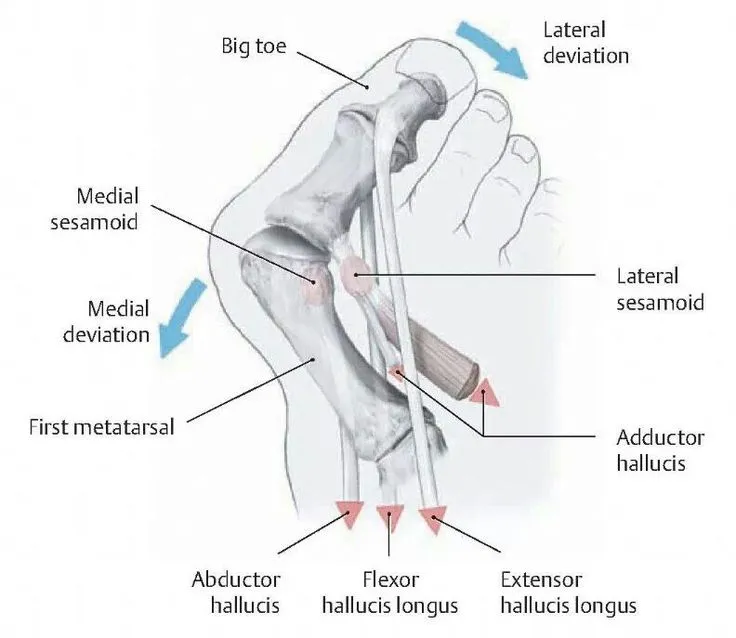
Bunions are most likely to develop when feet, which are predisposed to this condition, are consistently squeezed into tight, pointed-toe footwear. In such situations, the big toe exerts pressure on the adjacent toes, sometimes overlapping or diving beneath them. Consequently, the base of the big toe, known as the metatarsophalangeal (MTP) joint, protrudes or tilts away from the foot. To assess the severity of a bunion, medical professionals employ X-rays to measure specific angles between bones in the foot. Notably, they consider the hallux valgus angle (HVA), which is the angle formed between the first metatarsal and the big toe, and the intermetatarsal angle (IMA), which measures the angle between the first and second metatarsals. The upper limit of normal for HVA is 15 degrees, while for IMA, it’s 9 degrees.
While shoes with narrow toe boxes can trigger bunions, they are not the root cause. Bunions tend to have a genetic component, as foot type (including shape and structure) is inherited, and certain foot types are more prone to developing bunions. Factors such as low arches, flat feet, and lax joints and tendons also increase the susceptibility to bunions. Additionally, the shape of the metatarsal head (the top of the first metatarsal bone) plays a role, as a rounded shape makes the joint less stable and more prone to deformation when constrained by narrow shoes.
High-heeled shoes can exacerbate the problem because they shift the body’s weight forward, forcing the toes into the front of the shoe. This may explain why bunions are approximately ten times more prevalent in women than men.
Certain occupations that involve extensive standing and walking, such as teaching and nursing, can make individuals susceptible to bunions. Ballet dancers, whose feet endure significant repetitive stress, are also at risk. Women may develop bunions and other foot issues during pregnancy due to hormonal changes that loosen ligaments and flatten the feet. Additionally, bunions are linked to arthritis, which can damage the joint’s cartilage.
It’s possible to alleviate pain and halt the progression of bunions through conservative measures that relieve pressure on the MTP joint and enhance foot mechanics. Generally, bunions do not necessitate surgery unless there is an underlying deformity that cannot be corrected by other means or if the pain becomes unbearable despite conservative treatments.
Description
A bunion takes shape when the components comprising the metatarsophalangeal (MTP) joint undergo a misalignment: the elongated metatarsal bone shifts inward towards the interior of the foot, while the phalanx bones of the big toe incline towards the second toe. Consequently, the MTP joint enlarges and protrudes from the inner aspect of the forefoot.
The enlarged joint frequently becomes inflamed due to irregular biomechanics and direct irritation. Interestingly, the term “bunion” originates from the Greek word for “turnip,” as the protuberance on the inner side of the foot often resembles a reddened and swollen turnip.
Bunion Progression:
Bunions typically commence as small anomalies but frequently progress over time. Since the MTP joint flexes with each step, the larger the bunion becomes, the more agonizing and challenging walking can be.
In advanced stages, a bunion can significantly alter the foot’s appearance. In severe cases, the big toe might angle either underneath or over the second toe. The pressure exerted by the big toe may displace the second toe, leading to contact with the third toe. This can result in hammer toe deformities affecting the smaller toes. Calluses may also form where the toes rub against one another, exacerbating discomfort and hindering mobility.
Health Issues Associated with Bunions:
Bunions can give rise to associated problems, including:
- Bursitis: The formation of a bunion can irritate and inflame the bursa, a fluid-filled sac that cushions the joint’s bones, leading to bursitis, which is often painful.
- Arthritis: Bunions may compel the bones in the foot to rub against each other at uncomfortable angles, potentially wearing away the cartilage, which serves as a protective cushion for bone ends. This friction can result in arthritis, a painful condition that can lead to the deterioration of bone tissue.
- Hammer Toe: Bunions can induce the adjacent toe to the big toe to abnormally bend, forming a hammer toe, further intensifying pressure and discomfort.
Foot Issues Linked to Bunions:
In some instances, an enlarged MTP joint may trigger bursitis, characterized by the inflammation of the bursa, a fluid-filled sac cushioning the joint’s adjacent bones. Moreover, it can contribute to persistent pain and arthritis if the smooth articular cartilage that coats the joint’s surfaces is damaged due to improper joint movement.
Adolescent Bunion
Apart from the common bunion, there exist other variants, including adolescent bunions. These are particularly prevalent in girls aged 10 to 15. While an adult’s bunion often restricts movement in the MTP joint, an adolescent with a bunion typically retains normal big toe mobility. Nonetheless, an adolescent bunion can still be painful and interfere with the ability to wear certain types of shoes.
Bunionette
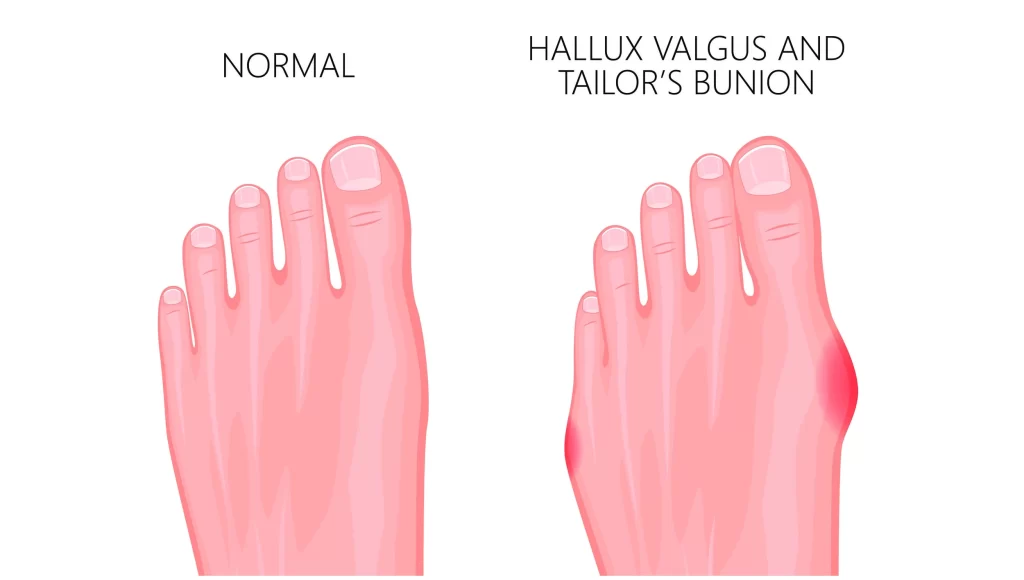
A bunionette, often referred to as a “tailor’s bunion,” manifests on the outer side of the foot near the base of the little toe. Despite its location, a bunionette closely resembles a regular bunion. It can lead to painful bursitis and the development of a tough corn or callus over the bony prominence.
Causes of Bunions
Bunions result from a complex interplay of factors that influence the condition’s severity. According to the American Podiatric Medical Association (APMA), the following factors contribute to bunion formation:
- Abnormal Foot Mechanics and Structure: Disrupted force balance on foot joints and tendons can stem from irregular foot mechanics and structure.
- Inherited Foot Mechanics: Inherited traits, such as loose ligaments, can exert abnormal pressure on the metatarsophalangeal (MTP) joint, contributing to bunions.
- Foot Injuries: Past foot injuries can play a role in the development of bunions.
- Flat Feet or Low Arches: Individuals with flat feet or low arches may be more susceptible to bunions.
- Neuromuscular Disorders: Conditions like cerebral palsy, affecting neuromuscular function, can influence bunion formation.
- Congenital Deformities: Certain congenital deformities, including flat feet from birth, may predispose individuals to bunions.
- Arthritis and Inflammatory Joint Diseases: Arthritis and inflammatory joint diseases can alter joint mechanics and contribute to bunion development.
- Ill-Fitting Shoes: Wearing shoes that do not provide adequate toe space, such as high heels or ill-fitting footwear, can exacerbate the risk of bunions.
- Occupational Factors: Professions that place significant pressure on the feet, such as ballet, can increase the likelihood of bunions.
- Pregnancy: During pregnancy, the release of the hormone relaxin can lead to ligament laxity, including in the foot ligaments, potentially contributing to bunion formation.
Risk Factors for Bunions
Bunion-related risks can vary from person to person. Dr. Levine highlights the following common risk factors:
- Skin Breakdown and Infection: Skin breakdown near the bunion can create an entry point for bacteria, potentially leading to infection.
- Rheumatoid Arthritis: Rheumatoid arthritis can affect foot joints, increasing the susceptibility to developing bunions.
- Ankle, Knee, and Gait Problems: Bunions may be associated with issues in the ankle and knee joints and gait abnormalities.
- Overall Foot Pain: Bunions can contribute to generalized foot pain.
- Local Toe Pain: Discomfort may specifically manifest at the enlarged big toe joint or at the base of the foot.
- Increased Risk of Falls: Due to potential foot instability caused by bunions, there is an elevated risk of falling.
Understanding these causative factors and risk factors is crucial for managing and preventing bunions effectively.
Symptoms of a Bunions
A hallmark symptom of a bunion is the emergence of a noticeable bump at the base of the big toe, though similar bumps can also appear at the base of the little toe, in which case it is often diagnosed as a bunionette or colloquially referred to as a “tailor’s bunion.”
Bunion symptoms may encompass the following:
- Pain and Discomfort: Individuals with bunions often experience pain and soreness in the affected area.
- Numbness: Some may report numbness in the vicinity of the bunion.
- Burning Sensation: A burning sensation can be present around the bunion.
- Swelling: Swelling is expected at the joint of the affected toe, contributing to its distinctive appearance.
- Increased Skin Thickness: The skin at the base of the affected toe may thicken over time.
- Hardened Skin: Hardened or callused skin can develop beneath the foot due to the altered weight distribution caused by the bunion.
- Redness: Redness is often observed around the bunion, adding to the discomfort.
- Corns or Calluses: The presence of corns or calluses is not uncommon as friction between the toes or against footwear intensifies.
- Limited Toe Movement: The affected toe may experience restricted mobility, reducing its range of motion.
It’s worth noting that wearing narrow shoes and high heels or standing for extended periods can exacerbate these symptoms. Initially, bunions manifest as small lumps but tend to progress over time, leading to increased pain and difficulties with walking.
Stages of Bunions
Bunions progress through four distinct stages, and if you suspect you have one, it’s crucial to consult a Podiatry Center for a proper diagnosis. Podiatrists can accurately determine the stage of your bunion, recommend appropriate treatments, and explain everything in simple terms. Regardless of the stage, effective treatment options are available to alleviate the discomfort associated with this common foot condition.
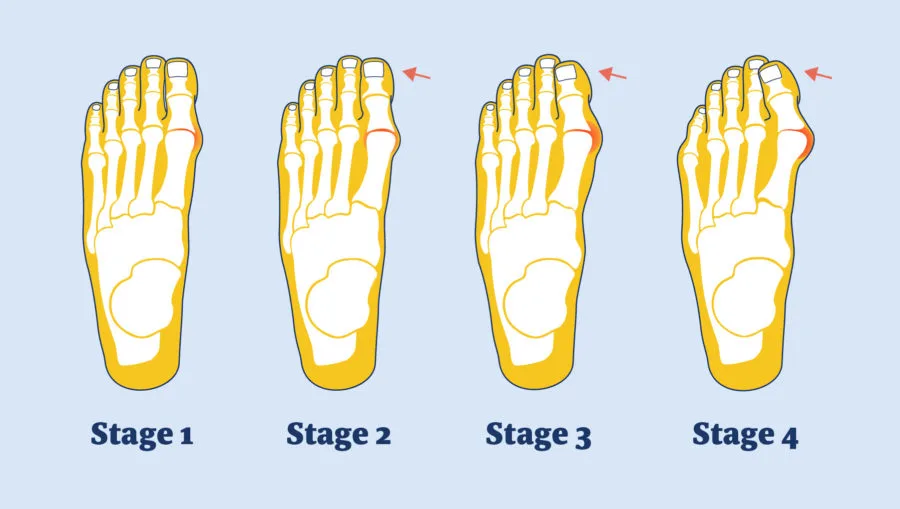
Stage 1: Inflammatory
In the initial stage, a bunion appears mildly. There is a small “bump” on the side of the 1st metatarsophalangeal (MTP) joint, and the big toe slightly turns towards the second toe without touching it.
- Symptoms include pain, heat, swelling, erythema, and minimal deviation of the big toe, but there’s a noticeable medial prominence at the MTP joint.
- Joint pain results from inflammation of a small bursa formed over the medial eminence.
- The thickening of the bursa wall accentuates the prominence.
- Consult a Podiatrist for a proper diagnosis, ruling out other conditions like gout, arthritis, or infection, and initiate corrective treatment to prevent worsening. Early intervention is recommended.
Stage 2: Mild
In this stage, the big toe continues to deviate from the MTP joint, and it may begin to touch the second toe.
- Usually asymptomatic, meaning no pain is experienced.
- The big toe gradually points outward towards the second toe.
- The first bone (phalanx) of the big toe remains aligned with the MTP joint, anchoring it.
Stage 3: Moderate
At this point, a significant bony protrusion forms at the base of the big toe, and a bone spur develops. The big toe also starts rotating away from the body’s midline.
- The metatarsal head of the big toe becomes displaced.
- The sesamoid bone is also displaced, roughly 75% away from beneath the metatarsal head.
- The first bone (phalanx) of the big toe starts dislocating from the MTP joint anchoring it.
Stage 4: Severe
In the advanced stage, the 1st MTP joint completely dislocates, causing the 1st toe to under-ride or override the 2nd toe. Additionally, the 2nd toe may develop a hammer toe deformity.
- There is a significant metatarsus primus varus.
- Complete dislocation of the sesamoid bones is observed.
- Pronation of the big toe is prominent, with overlapping onto the second toe.
- Soft tissues become contracted.
- The big toe bones are entirely misaligned with the big toe (MTP) joint.
- This stage is often associated with rheumatologic or neuromuscular diseases.
Diagnosis of a Bunions
Diagnosing a bunion involves several key steps to ensure an accurate assessment and treatment plan:
- Physical Examination: Your doctor will start by discussing your medical history, overall health, and any symptoms you’re experiencing. A thorough examination of your foot will be conducted. While the appearance of your toe and your reported symptoms can be indicative, a physical examination is essential.
- X-rays: X-rays are valuable diagnostic tools as they provide detailed images of dense structures like bones. They serve several crucial purposes in bunion diagnosis:
- Assess Toe Alignment: X-rays help your doctor assess the alignment of your toes and detect any damage to the metatarsophalangeal (MTP) joint. Your foot’s bone alignment can vary when you are sitting, standing, or bearing weight. To accurately evaluate the misalignment of foot bones, your doctor may take X-rays while you are standing.
- Detect Arthritis: X-rays can reveal if there’s any arthritis associated with the bunion, which can influence treatment decisions.
- Determine Bunion Severity: They also aid in gauging the extent of the bunion deformity and guide the choice of the most suitable corrective measures.
- CT Scan or Other Imaging: In some cases, a CT scan or additional imaging studies may be recommended. A CT scan provides a comprehensive view of both bone and soft tissue, offering a more complete perspective of the bunion’s structure and potential impact.
- Blood Tests: While less common, blood tests may be ordered to rule out any underlying medical conditions that could contribute to the development or progression of the bunion. These tests help ensure a comprehensive assessment of your foot health.
Nonsurgical Treatment for Bunions
Non-surgical methods are often effective in managing many bunions, particularly when identified early. Collaborative efforts among your healthcare team members, including your doctor and physical therapist, ensure a tailored approach to your care. Here are various non-surgical options:
- Footwear Selection: Opt for well-fitting footwear with a spacious toe box that comfortably accommodates your toes without undue pressure. Shoes with low heels and adequate padding, such as athletic footwear, are recommended.
- Padding: Alleviate discomfort from skin irritation by applying moleskin or gel bunion pads, readily available at your local pharmacy.
- Taping and Splinting: Your healthcare provider can teach you how to tape your toes to encourage proper alignment. Some individuals find relief by wearing a splint at night to maintain toe positioning.
- Pain Medication: Over-the-counter anti-inflammatory medications can help reduce pain and inflammation. If arthritis is contributing to your bunion discomfort, your doctor may prescribe specific medications to address it.
- Custom Foot Orthotics: Orthotic shoe inserts are customized to support your foot and control its positioning. These inserts can provide pain relief and help prevent further bunion progression.
- Physical Therapy: Physical therapy interventions, such as ultrasound therapy, whirlpool treatments, massage, heat therapy, and cold compresses, can offer relief from bunion-related pain.
- Injections: Your healthcare provider may administer injections with medications aimed at minimizing pain and inflammation, thereby improving joint mobility.
It’s important to note that nonsurgical treatments are primarily designed to manage pain and prevent the worsening of the condition rather than to cure the bunion itself.
Changes in Footwear:
Properly fitting shoes with a wide or open-toe box that doesn’t compress the toes can significantly alleviate bunion pain. Some shoes can be modified using a stretcher to reduce pressure on the toes. Your doctor can guide you on proper shoe fit and recommend suitable footwear.
Padding:
Silicone pads placed inside your shoes can provide cushioning for the painful bunion area. However, it’s advisable to test these pads for short periods initially, as their size may inadvertently increase pressure on the bump, potentially exacerbating your discomfort.
Orthotics and Other Devices:
To relieve pressure on the bunion, your doctor may suggest:
- Over-the-counter or custom-made shoe inserts (orthotics).
- Toe spacers to separate the toes.
Nighttime splints that position your big toe straighter, potentially offering relief. Note that braces or splints are not typically a permanent solution for bunions.
Medications:
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, can help manage pain and reduce swelling. In cases where bunions are aggravated by arthritis, other prescribed medications may be recommended to address pain and inflammation effectively.
Tips for Proper Shoe Fit
Ensuring that your shoes fit correctly is crucial, especially if you have bunions. Here are some general guidelines and tips to consider when selecting footwear:
General Guidelines:
- Prioritize Comfort: Opt for shoes with wide insteps, broad toe boxes, soft soles, and good stability. These features promote comfort and reduce pressure on your bunions.
- Avoid Tight and Pointed Shoes: Steer clear of shoes that are too short, excessively tight, or sharply pointed. High-heeled shoes, with heels taller than a couple of inches, should also be avoided as they increase forefoot pressure and the risk of foot problems or injury.
- Consider Rocker Bottom Shoes: If you experience pain in the metatarsophalangeal (MTP) joint during motion, shoes with a slight rocker bottom can be beneficial. These shoes assist in smooth gait and reduce stress on the MTP joint.
Tips for Shoe Selection:
- Size Variation: Do not rely solely on the size marked inside the shoe, as sizes can vary among brands and styles. Focus on how the shoe fits your foot.
- Conforming Fit: Select shoes that closely match the shape of your foot.
- Regular Measurements: Have your feet measured regularly because foot size can change as you age.
- Measure Both Feet: Measure both feet, as one foot is often larger than the other. Choose shoe sizes based on the larger foot.
- End-of-Day Fitting: Fit shoes at the end of the day when your feet are at their largest due to daily activities and gravity.
- Standing Fit: Stand during the fitting process and ensure there is ample space (approximately 3/8″ to 1/2″) for your longest toe at the end of the shoe.
- Ball of Foot Fit: Confirm that the ball of your foot sits comfortably in the widest part (ball pocket) of the shoe.
- Avoid Tightness: Do not purchase shoes that feel too tight, expecting them to stretch over time. Shoes should provide immediate comfort.
- Heel Fit: Ensure your heel fits comfortably in the shoe with minimal slippage.
- Test Walk: Walk in the shoes to assess their fit and comfort. Remember that stylish shoes can also be comfortable if selected wisely.
When to Consider Bunion Surgery
The decision to undergo bunion or bunionette surgery is typically considered when, despite attempting changes in footwear and other nonsurgical treatments over a period of time, you continue to experience persistent pain and walking difficulties.
Bunion surgery aims to alleviate pain by repositioning the affected bone, ligaments, tendons, and nerves to restore the big toe to its proper alignment. Surgery is generally recommended for bunions that are causing significant pain.
Various surgical options are available to address bunions, with the choice depending on the bunion’s size and severity. Smaller surgical procedures are appropriate for minor bunions, while more extensive interventions are required for severe cases. Your doctor will recommend a specific type of bunion surgery based on your X-ray results and the findings from your physical examination.
Bunion surgery is typically performed as an outpatient procedure, allowing patients to return home on the same day without requiring a hospital stay. However, it’s important to note that bunion surgery often involves a lengthy recovery period. The post-surgery recovery process can vary depending on the type of bunion surgery you undergo. Some procedures permit immediate weight-bearing with the use of a rigid-soled shoe, while others may necessitate a brief period of immobilization without weight-bearing.
In the case of adolescent bunions, surgical intervention is generally discouraged unless the bunion causes severe and unrelenting pain that persists despite adjustments in footwear or the incorporation of orthotic devices. If an adolescent undergoes bunion surgery, particularly before reaching skeletal maturity, there is a substantial likelihood that the bunion may return. Therefore, surgery for adolescent bunions should be carefully considered and approached with caution.
| Bunion surgery option by Category | |
| Category | Surgical treatment |
Mild bunion | Shaves the metatarsal head’s outermost bony growth. realigns the joint’s ring muscles, tendons, and ligaments. Wearing a postoperative shoe is typically required during recovery, which lasts 3–4 weeks. may not treat the bunion’s underlying deformity. |
Moderate bunion | The same as for a small bunion, plus cutting (osteotomy) the metatarsal head to realign it. Screws or pins are used to secure the bone in place. 4-6 weeks are needed for recovery, depending on the surgery. You might need to use crutches and wear a brief cast. |
Severe bunion | Removes the extra bony growth at the metatarsal bone’s head. realigns the metatarsal bone, which is held in place with screws or pins, by removing a wedge-shaped section of bone. tendons and ligaments are adjusted. It takes 6–12 weeks to recover. You might need to use crutches and wear a brief cast. A synthetic joint may be used to replace the damaged one if it cannot be repaired. |
Bunion Surgery Recovery Duration:
The recovery period following bunion surgery varies depending on the specific procedure performed:
- Distal Chevron Procedure: Patients who undergo a distal chevron procedure can begin bearing some weight on the foot as early as the day following surgery.
- Scarf Procedure: Those who have had a scarf procedure typically start partial weight-bearing at around two weeks post-surgery, often relying on crutches for support during this period.
- Lapidus Procedure: For individuals undergoing a Lapidus procedure, a cast is typically worn, and crutches are used for eight weeks. Swelling can persist for an extended period, gradually diminishing over the course of the first year after surgery.
Regardless of the specific procedure, individuals who have had a distal chevron, scarf, or crescent osteotomy can usually transition to wearing some form of shoe or sneaker after approximately 6 to 7 weeks.
In contrast, those undergoing the Lapidus fusion procedure may need to wait longer, typically around 10 to 12 weeks, before they can comfortably wear shoes.
Formal physical therapy is often unnecessary, as patients are typically provided with range of motion exercises for the affected toe. Physical therapy is considered only if progress in regaining motion is slower than expected.
Overall, bunion surgery has a high success rate. However, it’s worth noting that orthopedic surgeons at the Foot and Ankle Service at HSS occasionally treat patients who have experienced unsatisfactory outcomes from bunion surgeries performed elsewhere. While these issues can be addressed, the likelihood of success is significantly higher when the appropriate procedure is expertly performed the first time.
If you are contemplating bunion surgery, it is strongly recommended to consult with an experienced orthopedic surgeon proficient in a wide range of surgical techniques, encompassing both straightforward and complex procedures. This ensures that you receive the most suitable surgical intervention for your condition, as well as appropriate post-surgery recovery and rehabilitation guidance.
Outcomes and Complications of Bunion Surgery:
The evaluation of bunion surgery outcomes can be complex due to variations in toe-joint deformities and surgical techniques. While some studies suggest that approximately 85% to 90% of patients are content with their surgical results, others have found that up to a third of patients may express dissatisfaction, even if their pain and toe alignment improve. Unrealistic expectations can contribute to this, as some patients mistakenly anticipate that the surgery will yield a completely straight big toe and enable them to wear narrower shoes immediately. Additionally, patients may expect quicker relief from post-surgical pain and swelling than the actual recovery timeline allows.
The most prevalent complication following bunion surgery is the recurrence of the bunion, reported in as many as 16% of cases. This can occur when the procedure focuses solely on shaving the bony prominence without addressing the underlying deformity.
Occasionally, the rejoining of cut bones can be delayed or, in rare instances, fail to occur altogether. This condition, known as nonunion, typically necessitates a second surgery. Other potential complications include irritation stemming from the pins or screws used to stabilize the bones, as well as excessive scarring or stiffness. While post-surgical swelling generally subsides within two months, it may persist for six months or longer, and joint stiffness can endure for several months. Although rare, nerve damage and persistent pain can prolong recovery and potentially require further surgical intervention. The risk of infection is lower than 1%.
Deciding to undergo bunion surgery is not a simple choice. It entails a careful consideration of potential benefits and risks. The positive aspect is that bunion surgery is not an urgent medical procedure, affording individuals the time to explore their options, gather information, and, if desired, seek a second opinion.
Bunions typically start as small deformities that progressively worsen over time if left untreated. As they grow, they can become increasingly painful and hinder walking. In severe cases, the big toe may extend over or under the second toe, exerting pressure that misaligns the second toe and pushes it against the third toe.
Without intervention, bunions may also lead to associated conditions, including:
- Bursitis: Inflammation of the bursa, a fluid-filled sac that cushions bones, tendons, and muscles near joints, particularly in the big toe.
- Hammer toe: An abnormal bending of the toe joint.
- Metatarsalgia: Inflammation of the ball of the foot, causing pain and discomfort.
Prevention of Bunions
Taking proactive steps can aid in preventing or mitigating the advancement of bunions:
- Select Proper Footwear: Avoid shoes with narrow toe boxes that compress the toes. Opt for footwear with a spacious toe area that allows your toes to spread comfortably.
- Supportive Shoes: If you have excessive flattening of the foot arches, ensure you wear supportive shoes. If needed, consult with a podiatrist to obtain custom orthotics tailored to your foot’s unique needs.
- Early Intervention: At the first signs or symptoms of a bunion deformity, consult with your podiatrist promptly. Early treatment and intervention may effectively halt or slow down the progression of the bunion.
By being proactive and making informed choices about your footwear and foot health, you can reduce the risk of developing bunions and potentially prevent their worsening.
FAQ
What is the main cause of bunions?
Bunion. Long-term foot pressure that compresses the big toe and forces it toward the second toe is typically what leads to bunions. As additional bone develops where the base of the big toe meets the foot over time, the condition may become uncomfortable.
How do I fix my bunion?
A bunion can only be removed surgically. Exercise and other alternatives, such as orthotics, can also lessen pain. Your big toe has a noticeable lump called a bunion. Your toe’s joint at the bottom is where it happens.
Can a bunion go away?
Bunions can’t be repaired & don’t vanish on their own. If you already have a bunion, it will likely get worse over time. Fortunately, a lot of people can treat their bunions without surgery. Home cures, orthotics, and other treatments are options for pain management.
Who suffers from bunions?
Bunions are more familiar in females than in males. Women who frequently wear high heels or footwear that is excessively snug near the toes are more likely to develop bunions. Bunions might get worse during pregnancy and menopause.
At what age do bunions develop?
Although bunions can develop at any age, we have seen them in children as young as 4-5 years old. The severity of the deformity may worsen and the necessity for more intensive treatment may increase with the early age of beginning of this type of hump.
Is bunions good or bad?
The function of the foot can be severely hampered by a bunion at this vital intersection of bones, tendons, and ligaments. A bunion on the big toe, for instance, can harm the other toes. They could get twisted and form hammertoes under the strain of the big toe.
Is bunion surgery painful?
Each person reacts to bunion surgery differently, varying in their level of pain. The majority of people will feel uncomfortable for three to five days. Following your foot and ankle surgeon’s recommendations to the letter will help you reduce swelling and pain following your bunion surgery.
Are bunions normal?
Approximately 23% of those between the ages of 18 and 65 and 36% of those over the age of 65 report having bunions. As a result, many individuals could consider them unimportant and unnecessary. Bunions can, however, lead to long-term issues for your feet in addition to pain and suffering if they are not treated.
Is walking good for bunions?
Both yes and no, is the answer. Walking barefoot on occasion can help with bunion management. If your bunion is particularly painful or tender, for instance, you should always attempt to wear shoes that fit well and don’t rub against them while you walk.
Can bunions be treated at home?
Despite the fact that bunions cannot be healed naturally, natural bunion treatment can assist in reducing the discomfort and pressure they bring. If a person has serious discomfort from a bunion or other problems, they should consult a doctor. To help ease the strain on the big toe, people should apply cushioning and put on cozy shoes.
Reference
- Bunions – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/bunions/
- What to do about bunions. (2020, July 2). Harvard Health. https://www.health.harvard.edu/diseases-and-conditions/what-to-do-about-bunions
- Whnp-Bc, L. S. M. B. (2019, February 18). What you need to know about bunions. https://www.medicalnewstoday.com/articles/310096#prevention
- Bunions: Overview of Types and Treatments. (n.d.). Hospital for Special Surgery. https://www.hss.edu/conditions_bunions-overview.asp
- Bennington-Castro, J. (2023, January 27). What Are Bunions? Symptoms, Causes, Diagnosis, Treatment, and Prevention. EverydayHealth.com. https://www.everydayhealth.com/bunion/guide/
- Bunions Symptoms & Treatment | Aurora Health Care. (n.d.). Aurora Health Care. https://www.aurorahealthcare.org/services/orthopedics/conditions/bunions
- Jesner, L. (2023, June 21). What Are Bunions? Symptoms, Causes, Treatments And More. Forbes Health. https://www.forbes.com/health/conditions/bunions/






One Comment