Trochanteric bursitis
Introduction
In many areas of the body, muscles and tendons must slide over and against one another during movement. At each of these places, a small sac of lubricating fluid helps the muscles and tendons move properly. One of these places is the hip. Usually, these sacs of fluid, called bursae, function to reduce friction, but if they become swollen and irritated, they can cause pain.
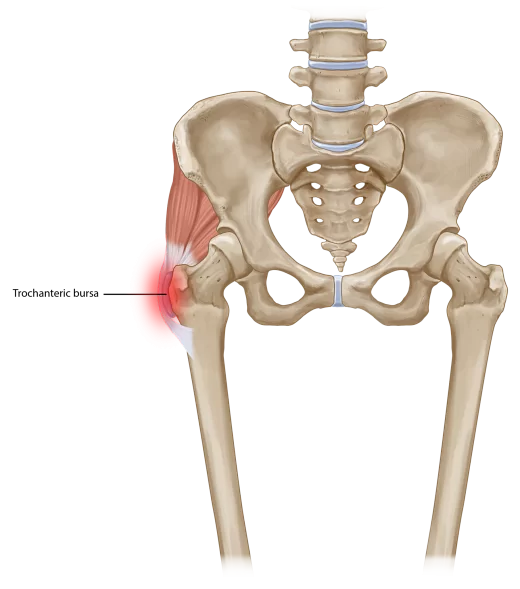
One common area where this occurs is the bursa on the outside of the hip (trochanteric bursa) creating a condition known as trochanteric bursitis. This condition is common in older individuals but may occur in younger patients who are extremely active.
What is trochanteric bursitis?
Definition: Trochanteric bursitis is inflammation (swelling) of the bursa (fluid-filled sac near a joint) at the outside (lateral) point of the hip known as the greater trochanter. When this bursa becomes irritated or inflamed, it causes pain in the hip. This is a common cause of hip pain.
Anatomy:
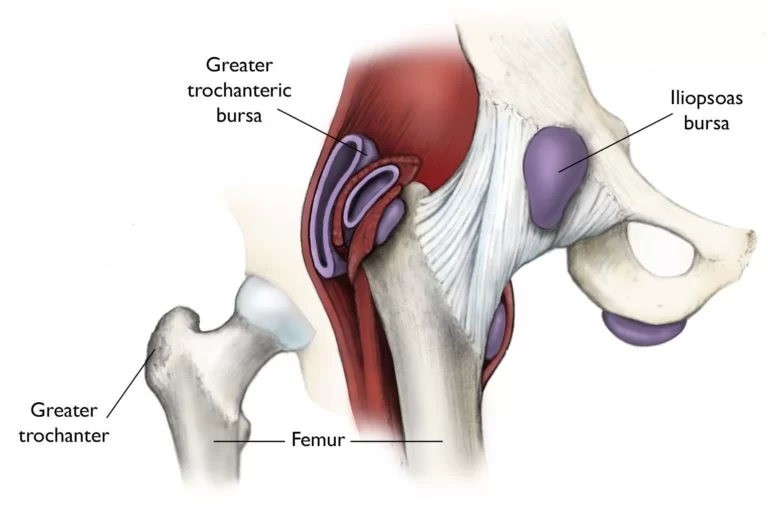
The hip socket is called the acetabulum and forms a deep cup surrounding the ball of the upper thighbone (femur), or femoral head. The hip is surrounded by the thick muscles of the buttock at the back and the thick muscles of the thigh in the front.
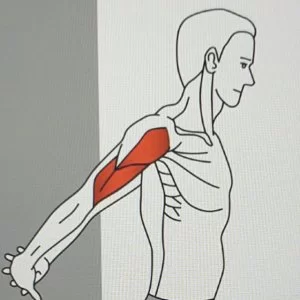
On the outside of the upper end of the femur is a large bump (greater trochanter). This bump is the point where the large buttock muscles that move the hip connect to the femur. These muscles help rotate and move the hip outward. Another layer of muscle, the gluteus maximus, slides over this bump and is attached further down on the thigh bone (femur).
Where friction must occur between muscles, tendons, and bones there is usually a structure called a bursa. A bursa is a thin sac of tissue that contains a bit of fluid to lubricate the area where the friction occurs. The bursa is a normal structure, and the body will even produce a bursa in response to friction.
Causes:
- Injury to the point of the hip. This can include falling onto the hip, bumping the hip into an object, or lying on one side of the body for an extended period.
- Play or work activities that cause overuse or injury to the joint areas. Such activities might include running up stairs, climbing, or standing for long periods of time.
- Incorrect posture. This condition can be caused by scoliosis, arthritis of the lumbar (lower) spine, and other spine problems.
- Stress on the soft tissues as a result of an abnormal or poorly positioned joint or bone (such as leg length differences or arthritis in a joint).
- Other diseases or conditions. These may include rheumatoid arthritis, gout, psoriasis, thyroid disease, or an unusual drug reaction. In rare cases, bursitis can result from infection.
- Previous surgery around the hip or prosthetic implants in the hip.
- Hip bone spurs or calcium deposits in the tendons that attach to the trochanter.
- Other causes of trochanteric bursitis include:
- muscle tears
- hip injuries
- hip surgery complications
- poor posture
- diseases such as gout (a form of arthritis with sudden, sharp attacks of pain, often at the base of the big toe)
Sometimes a bursa can become inflamed because of too much friction or because of an injury to the bursa which can result in pain.
Friction can occur in the bursa during walking if the long tendon on the side of the thigh is tight. It is unclear what causes this tightening of the tendon. The gluteus maximus attaches to this long tendon. As you walk the gluteus maximus pulls this tendon over the greater trochanter with each step. When the tendon is tight, it rubs closely against the bursa with each step. The rubbing causes friction to occur in the bursa, leading to irritation and inflammation. Friction can also start if the outer hip muscle (gluteus medius) is weak, if one leg is longer than the other, or if you run on banked surfaces.
Most cases of trochanteric bursitis appear gradually with no obvious underlying injury or cause. Trochanteric bursitis can occur after the artificial replacement of the hip joint or other types of hip surgery. This may be a combination of changes in the way the hip works, the way it is aligned, or the way scar tissue has formed from the healing incision. Trochanteric bursitis can also occur as a result of repetitive motion injuries from activities such as running.
A fall on the hip can injure the bursa. This may cause bleeding into the bursa. The bleeding is not serious, but the bursa may react to the blood by becoming inflamed. The inflammation causes the bursa to become thickened over time. This thickening, constant irritation, and inflammation may result in the condition becoming chronic, or long-lasting.
Symptoms:
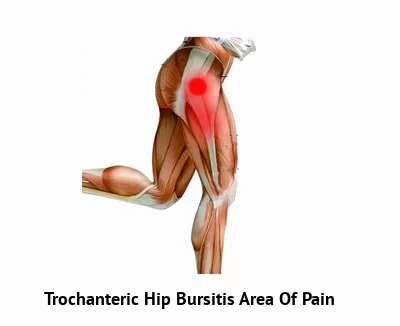
- Pain on the outside of the hip and thigh or in the buttock. The pain may be sharp, but with time, it may turn into a dull ache.
- If left untreated, the pain may start going down your upper leg. You’ll likely feel it when you lay on the side of your affected hip and when getting up from a chair. The joint becomes stiff, and the bursa itself is sensitive to touch.
- In extreme cases, your hip joint may become red and swollen and you may even have a fever.
- Pain when lying on the affected side.
- Pain when you press in or on the outside of the hip.
- Pain that gets worse during activities such as getting up from a deep chair or getting out of a car.
- Pain with walking upstairs.
- As the problem progresses, the symptoms include the development of a limp when walking and stiffness in the hip joint.
- Eventually, the pain will also be present at rest and may even cause a problem with sleeping.
Diagnosis:
The diagnosis of trochanteric bursitis begins with a history and physical examination. In fact, this is usually all that is necessary to make the diagnosis. Your doctor will want to know when the pain began and which motions cause the pain. A physical examination will be done to determine how much stiffness you have in the hip and if you have a limp. Once this is done, X-rays will most likely be ordered to make sure that there are no other abnormalities in the hip.
She may order X-rays to rule out other issues since bursitis itself doesn’t show up on X-rays. You could get an ultrasound test, and you may get an MRI if your hip isn’t responding to treatment.
Diagnostic Injection
One simple way that the diagnosis of trochanteric bursitis can be made is with an injection of local anesthetic directly into the bursa. This is a procedure that can easily be performed in the office. To perform this procedure, you will probably be asked to lay on the examining table on your side with the sore hip up. Once the skin is cleansed with antiseptic, a long needle is used to inject ten to twenty milliliters of medication such as novocaine directly into the trochanteric bursa. If the injection removes the pain immediately, then the diagnosis is probably trochanteric bursitis. Most physicians will also add a bit of cortisone medication into the novocaine to help treat the condition at the same time.
Treatment:
Treatments are generally nonsurgical and easy to do at home. They might include:
Ice. Apply ice packs to your hip every 4 hours for 20 to 30 minutes at a time. Cold numbs the area, which can reduce pain and may cut down on swelling and inflammation.
Anti-inflammatory medications. Over-the-counter medications such as ibuprofen (Advil, Motrin) and naproxen (Aleve), and prescription pain relievers such as celecoxib (Celebrex) can reduce pain and swelling. Be sure to check with your doctor before taking them, however.
Rest. If you can stay off your hip, you can give it time to heal. Using walkers, crutches, and other tools may help as well.
Physical therapy. An expert therapist can give you exercises to improve flexibility and strengthen your muscles.
Cortisone shots. Cortisone is a powerful anti-inflammatory medication. Athletes sometimes use these to reduce swelling and pain.
Low-energy shock wave therapy. Acoustic shock waves are passed through the skin with a targeted device. One analysis showed that more than two-thirds of patients given shock wave therapy were cured or greatly improved after 4 months.
Surgery. Though surgery is rarely needed, the bursa can be removed if it is beyond repair. It’s usually an outpatient procedure, meaning no overnight hospital stay. A surgeon will use an arthroscope — a kind of camera — and tiny instruments, as with common knee and elbow surgeries.
How do you prevent trochanteric bursitis?
Because most cases of bursitis are caused by overuse, the best treatment is prevention. It is important to avoid or modify the activities that cause the problem. Underlying conditions such as leg length differences, improper posture, or poor technique in sports or work must be corrected.
Apply these basic rules when performing activities:
- Take it slow at first and gradually build up your activity level.
- Use limited force and limited repetitions.
- Stop if unusual pain occurs.
Some tips:
- Avoid repetitive activities that put stress on the hips.
- Lose weight if you need to.
- Get a properly fitting shoe insert for leg length differences.
- Maintain strength and flexibility of the hip muscles.
- Use a walking cane or crutches for a week or more when needed.
When should you seek medical advice?
Most cases of bursitis improve without any treatment over a few weeks. See your healthcare provider if you have any of the following signs or symptoms:
- You experience pain that interferes with your normal day-to-day activities or has soreness that doesn’t improve despite self-care measures.
- You have a recurrence of bursitis.
- You have a fever or the area affected appears red, swollen, or warm.
In addition, see your doctor if you have other medical conditions that may increase your risk of an infection, or if you take medications that increase your risk of infection, such as corticosteroids or immunosuppressants.
You can stop trochanteric bursitis from becoming worse or never have it at all if you take care of your hips (and the rest of your body) properly. Among the things you can do:
- Exercise the right way. It’s great being active, but training properly. That means stretching, warming up, and listening to your body.
- Wear proper orthotics or inserts. One cause of trochanteric bursitis is having one leg shorter than the other. Inserts can even out your gait.
Exercises:
Trochanteric Bursitis Treatment
PHASE I – Pain Relief & Protection
You are managing your pain. Pain is the main reason that you seek treatment for trochanteric bursitis. In truth, it was the final symptom that you developed and should be the first symptom to improve.
You are managing your inflammation. Bursa inflammation is best eased via ice therapy, cortisone injections, supportive taping techniques or exercises that encourage your muscles to decompress the bursa.
Your physiotherapist may use an array of treatment tools to reduce your pain and inflammation. These can include ice, electrotherapy, acupuncture, de-loading taping techniques, soft tissue massage, and temporary use of a mobility aid (e.g. cane or crutch) to off-load the affected side.
PHASE II – Restoring Normal ROM, Strength
As your pain and inflammation settle, your physiotherapist will turn their attention to restoring your normal hip function. This treatment may include your joint range of motion, muscle length and resting tension, muscle strength and endurance, proprioception, balance, and gait (walking pattern).
Hip researchers have discovered the importance of your hip muscle recruitment patterns with a standard order of deep, then intermediate, and finally, superficial muscle firing patterns in healthy pain-free hips. Your physiotherapist will assess your muscle recruitment pattern and prescribe the best exercises for you, specific to your needs.
PHASE III – Restoring Full Function
The final stage of your rehabilitation aims at returning you to your desired activities. Everyone has different demands for their hips that will determine what specific treatment goals you need to achieve. For some people, it only is to walk around the block. Others may wish to run a marathon.
Your physiotherapist will tailor your hip rehabilitation to help you achieve your own functional goals.
PHASE IV – Preventing a Recurrence
Trochanteric bursitis does tend to return. The main reason is due to insufficient rehabilitation.
In addition to your muscle control, your physiotherapist will assess your hip biomechanics and start correcting any defects. It may be as simple as providing you with gluteal or deep hip rotator exercises to address any biomechanical faults in your leg. Your physiotherapist will guide you based on your assessment.
You are fine-tuning your hip stability and function by addressing any deficits in core strength and balance, learning self-management techniques, and achieving the ultimate goal of safely returning to your previous sporting or leisure activities.
The home exercise regime has the following sections:
- stretches of the surrounding area including low back
- specific strengthening exercise for muscles around the hip
- balance exercise to activate the muscles around the hip and low back
You can do the first 3 stretches to begin stretching the muscles that run along the outside of your hip. You can do the strengthening exercises when the sharp pain lessens.
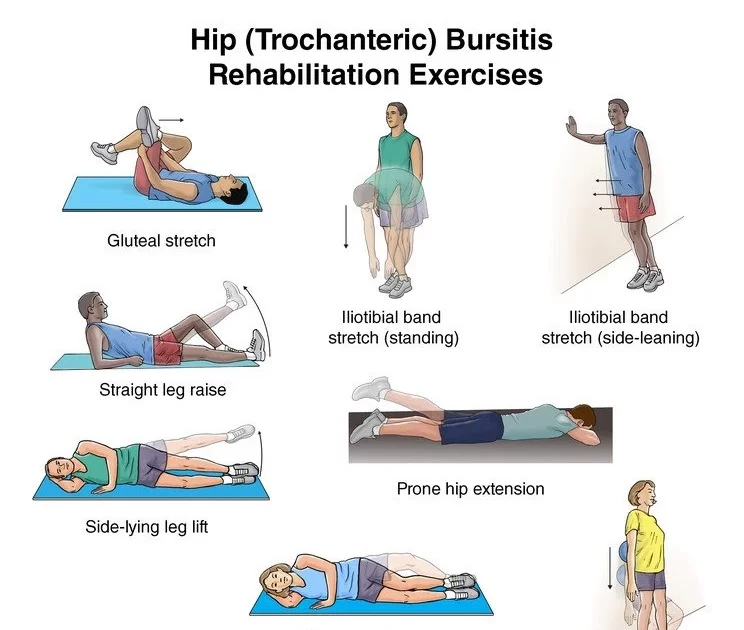
Stretching exercises
Gluteal stretch: Lie on your back with both knees bent. Rest the ankle on your injured side over the knee of your other leg. Grasp the thigh of the leg on the uninjured side and pull toward your chest. You will feel a stretch along the buttocks on the injured side and possibly along the outside of your hip. Hold the stretch for 15 to 30 seconds. Repeat 3 times.
Iliotibial band stretch, standing: Cross your uninjured leg in front of the other leg and bend down and reach toward the inside of your back foot. Do not bend your knees. Hold this position for 15 to 30 seconds. Return to the starting position. Repeat 3 times.
Iliotibial band stretch, side-leaning: Stand sideways near a wall with your injured side closest to the wall. Place a hand on the wall for support. Cross the leg farther from the wall over the other leg. Keep the foot closest to the wall flat on the floor. Lean your hips into the wall. Hold the stretch for 15 to 30 seconds. Repeat 3 times.
Hamstring wall stretch: Place one foot (and leg) on the wall and try to push your knee straight. Hold for 30 to 45 seconds. Gently release the stretch. Repeat with your other leg against the wall.
Strengthening exercises
Straight leg raise: Lie on your back with your legs straight out in front of you. Bend the knee on your uninjured side and place the foot flat on the floor. Tighten the thigh muscle on your injured side and lift your leg about 8 inches off the floor. Keep your leg straight and your thigh muscle tight. Slowly lower your leg back down to the floor. Do 2 sets of 15.
Prone hip extension: Lie on your stomach with your legs straight out behind you. Fold your arms under your head and rest your head on your arms. Draw your belly button in towards your spine and tighten your abdominal muscles. Tighten the buttocks and thigh muscles of the leg on your injured side and lift the leg off the floor about 8 inches. Keep your leg straight. Hold for 5 seconds. Then lower your leg and relax. Do 2 sets of 15.
Side-lying leg lift: Lie on your uninjured side. Tighten the front thigh muscles on your injured leg and lift that leg 8 to 10 inches (20 to 25 centimeters) away from the other leg. Keep the leg straight and lower it slowly. Do 2 sets of 15.

Wall squat with a ball: Stand with your back, shoulders, and head against a wall. Look straight ahead. Keep your shoulders relaxed and your feet 3 feet (90 centimeters) from the wall and shoulder’s width apart. Place a soccer or basketball-sized ball behind your back. Keeping your back against the wall, slowly squat down to a 45-degree angle. Your thighs will not yet be parallel to the floor. Hold this position for 10 seconds and then slowly slide back up the wall. Repeat 10 times. Build up to 2 sets of 15.
Clam exercise: Lie on your uninjured side with your hips and knees bent and feet together. Slowly raise your top leg toward the ceiling while keeping your heels touching each other. Hold for 2 seconds and lower slowly. Do 2 sets of 15 repetitions.
Side plank: Lie on your side with your legs, hips, and shoulders in a straight line. Prop yourself up onto your forearm with your elbow directly under your shoulder. Lift your hips off the floor and balance on your forearm and the outside of your foot. Try to hold this position for 15 seconds and then slowly lower your hip to the ground. Switch sides and repeat. Work up to holding for 1 minute. This exercise can be made easier by starting with your knees and hips flexed toward your chest.
The plank: Lie on your stomach resting on our forearms. With your legs straight, lift your hips off the floor until they are in line with your shoulders. Support yourself on your forearms and toes. Hold this position for 15 seconds. (If this is too difficult, you can modify it by placing your knees on the floor.) Repeat 3 times. Work up to increasing your hold time to 30 to 60 seconds.
other related posts :








3 Comments