Total Elbow Replacement and physiotherapy
Total Elbow Replacement : Introduction
Total Elbow Replacement : The elbow is a necessary joint for normal functioning in daily life, yet it is susceptible to various degenerative conditions and traumatic lesions or post-traumatic sequelae.
However a total elbow replacement is much less common than knee or hip replacement, it is just as successful in relieving joint pain and returning people to activities they enjoy.
Elbow replacement surgery is a complicated procedure partly because the elbow has several moving parts that balance each other with great precision to control the movements of your forearm.
Your elbow can be damaged by problems ranging from rheumatoid arthritis to traumatic fractures. In some cases, the damage can be surgically repaired. But if the damage is extensive, your doctor might recommend elbow replacement surgery. Pain is the most common reason people choose to have elbow replacement surgery.
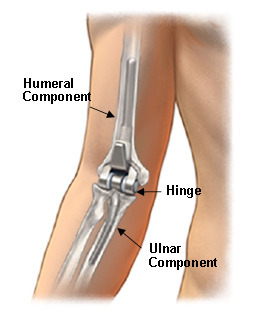
During elbow replacement, a surgeon replaces your elbow with an artificial joint made from two implants that attach to the bones in your arm. A metal and plastic hinge joins the implants together.
The procedure is similar to hip and knee replacements.
- Total elbow arthroplasty (TEA) is increasingly used for the treatment of many debilitating elbow pathologies
- TEA for trauma is one of the fastest-growing indications
- Forms of elbow arthroplasty
- total elbow arthroplasty
- hemi elbow arthroplasty
- radiocapitellar
- distal humeral
- ulnohumeral distraction & interpositional arthroplasty
- olecranon fossa debridement
- radial head arthroplasty
Elbow replacements were originally developed for those with RA
Elbow replacement was originally developed for people with rheumatoid arthritis. With this autoimmune disease, the body’s immune system attacks healthy tissue — primarily the tissue lining the joints. It usually affects multiple joints, which may include the elbows, causing pain, swelling and stiffness. If symptoms become severe and cannot be relieved with nonsurgical measures, elbow replacement becomes an option.
The more common type of arthritis — osteoarthritis — results from the deterioration of cartilage (which cushions the ends of bones in joints and creates a smooth gliding surface for movement), causing pain, swelling and stiffness. Weight-bearing joints, such as the hips and knees, are most susceptible.
Osteoarthritis can develop in the elbow, but it’s most likely to affect people who have had a traumatic injury to the elbow or who put excess pressure on their elbows. They may include heavy machine operators, weightlifters and some athletes.
Nonsurgical measures are used to treat osteoarthritis, regardless of the affected joint. If pain and diminished mobility in the elbow become severe, a last resort is an elbow replacement.
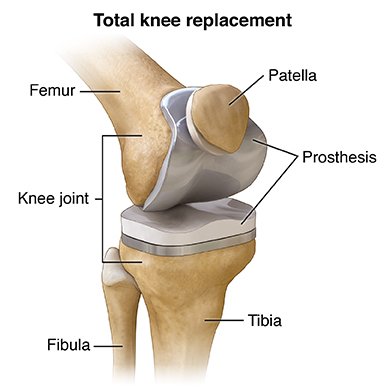
Anatomy
The elbow is a hinge joint which is made up of three bones:
- The humerus (upper arm bone)
- The ulna (forearm bone on the pinky finger side)
- The radius (forearm bone on the thumb side)
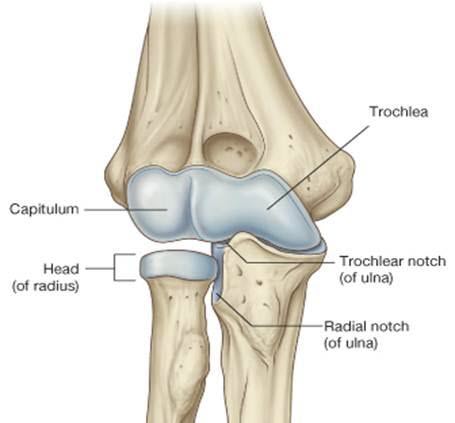
The surfaces of the bones where they meet to form the elbow joint are covered with articular cartilage, a smooth substance that protects the bones and enables them to move easily. A thin, smooth tissue called synovial membrane covers all remaining surfaces inside the elbow joint. In a healthy elbow, this membrane makes a small amount of fluid that lubricates the cartilage and eliminates almost any friction as you bend and rotate your arm. Muscles, ligaments, and tendons hold the elbow joint together.
What is Total Elbow Replacement?
In case of severe arthritis or multiple fractures of the elbow joint an elbow replacement surgery is recommended. In this surgery the elbow joint is replaced by an artificial joint which consist of two metal stems and a hinge made up of metal or plastic. During the surgery the stems are inserted inside the hollow part of the bone called canal.
Total Elbow Replacement Types :
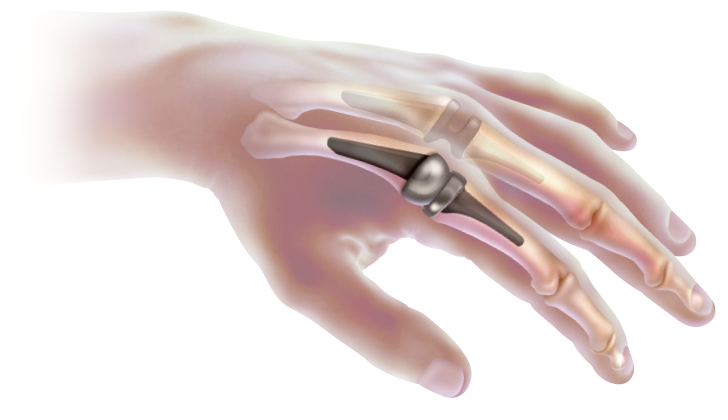
In some cases, you may need a replacement of just one portion of the joint. For example, if only the head of one of your forearm bones (radius) is damaged, it can be replaced with an artificial head.
If the entire joint needs to be replaced, the ends of the bones that come together in the elbow will be removed. Bones are hard tubes that contain a soft center. The long, slender ends of the artificial joint are inserted into the softer central part of the bones.
There are two main types of prosthetic devices available:
- Artificial elbow joints can either be of linked (semi-constrained) or unlinked (constrained) type.
- Linked. This type of prosthesis acts somewhat like a loose hinge because all the parts of the replacement joint are physically connected to each other. This provides good joint stability, but the stresses of movement can sometimes result in the prosthesis working itself loose from where it’s inserted into the arm bones.
- Unlinked. This type of device comes in two separate pieces that aren’t connected to each other. This design depends on the surrounding ligaments to help hold the joint together, which can make it more prone to dislocation.
There are two main categories of elbow arthroplasty:
- Hemiarthroplasty
- Total Elbow Replacement
There are different types of elbow replacements, and components come in different sizes.
Total Elbow Replacement : Causes/Indications
Several conditions can cause elbow pain and disability, and lead patients and their doctors to consider elbow joint replacement surgery.
Rheumatoid Arthritis
This is a disease in which the synovial membrane that surrounds the joint becomes inflamed and thickened. This chronic inflammation can damage the cartilage and eventually cause cartilage loss, pain, and stiffness.
Rheumatoid arthritis is the most common form of a group of disorders termed “inflammatory arthritis.”
Osteoarthritis (Degenerative Joint Disease)
Osteoarthritis is an age-related, “wear and tear” type of arthritis. It usually occurs in people 50 years of age and older, but may occur in younger people, too. The cartilage that cushions the bones of the elbow softens and wears away. The bones then rub against one another. Over time, the elbow joint becomes stiff and painful.
Rheumatoid arthritis and osteoarthritis cause cartilage damage that can result in severe pain and disability.
Post-traumatic Arthritis
This type of arthritis can follow a serious elbow injury. Fractures of the bones that make up the elbow, or tears of the surrounding tendons and ligaments may cause damage to the articular cartilage over time. This causes pain and limits elbow function.
Severe Fractures
A severe fracture of one or more bones that make up the elbow is another common reason people have elbow replacements. If the elbow is shattered, it may be very difficult for a doctor to put the pieces of bone back in place. In addition, the blood supply to the bone pieces can be interrupted. In this type of case, a surgeon may recommend an elbow replacement. Older patients with osteoporosis (fragile bone) are most at risk for severe elbow fractures.
In addition, some fractures do not heal well and may require an elbow replacement to address continuing problems.
Instability
Instability occurs when the ligaments that hold the elbow joint together are damaged and do not work well. The elbow is prone to dislocation. Chronic instability is most often caused by an injury.
Contraindications
- absolute
- active infection (arthrodesis favored)
- Charcot joint
- relative
- poor neurologic control of affected extremity
- active patient younger than <65 years old
- olecranon osteotomy
What Are the Risks?
The most common complications are:
- Infection
- Injury to nerves and blood vessels
- Allergic reaction to the artificial joint
- Broken bone
- Stiffness or instability of the joint
- Loosening or wearing of the artificial parts
- Weakness or failure in the tendons of your arm
- Pain
There are risks because of the anesthesia, such as an allergic reaction to those medicines and breathing problems. As with any surgery, bleeding and blood clots are possible, too.
Understanding limitations after elbow replacement
That said, elbow replacement isn’t for everyone. “The main limitation of elbow replacement surgery is the permanent lifting restriction of not more than seven pounds,” says Dr. Maschke. In addition, the implants aren’t likely to hold up for the several decades that would be necessary if used in a younger adult. For these reasons, elbow replacement surgery generally is reserved for older adults who don’t need to lift heavy items.
Diagnostic and surgical innovation
Surgical techniques to help make elbow replacement a highly effective treatment option.
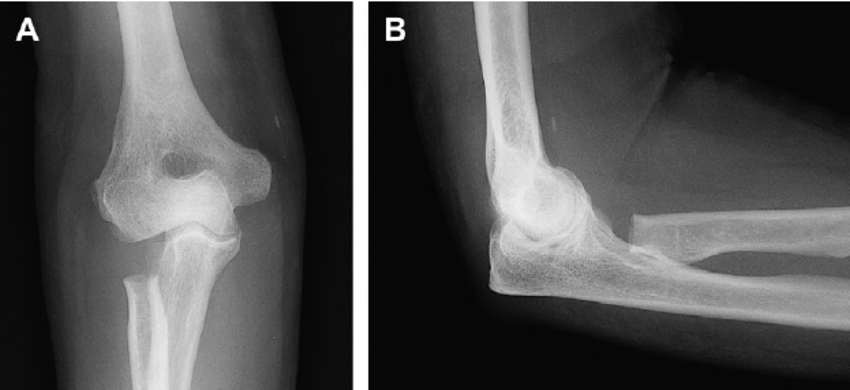
1.Affected joint(s) : Radial head
- Options : Radial head replacement
Plain radiographs : Radial head replacement
2. Affected joint(s) : Ulna
- Options : total elbow replacement
Plain radiograph : total elbow replacement

3. Affected joint(s) : Humeroradial
- Options : Radial head replacement
- Uncompartmental replacement
Plain radiograph : uncompartmental replacement

4. Affected joint(s) : Humeroulnar
- Options : Total elbow arthroplasty
- humerus hemiarthroplasty
Plain radiograph : Humerus hemiarthroplasty

5. Affected joint(s) : Radioulnar
- Options : Radial head replacement
- Radial head resection
Plain radiograph : Radial head resection
Surgical Procedure
To reach the elbow joint, your surgeon will make an incision (cut), usually at the back of the elbow. After making the incision, your surgeon will gently move muscles aside to get access to the bone. After removing scar tissue and spurs around the joint, your surgeon will prepare the humerus to fit the metallic piece that will replace that side of the joint. The same preparation is done for the ulna.
The replacement stems are placed into the humerus and ulna bones, and kept in place with a bone cement. The two stems are connected by a hinge pin. After the wound is closed, a padded dressing is then placed to protect the incision while it heals.
Some surgeons will place a temporary tube in the joint to drain the surgical fluid. This tube can be easily removed in your hospital room within the first few days after surgery.
Implants
The metal replacement parts are made of chrome-cobalt alloy or titanium and there is a liner made of polyethylene (plastic). The bone cement is made of polymethylmethacrylate (acrylic, a type of plastic).
Recovery
Your medical team will give you several doses of antibiotics to prevent infection. Most patients are able to eat solid food and get out of bed the day after surgery. You will most likely stay at the hospital 2 to 4 days after your surgery.
Pain Management
Although the operation is to relieve pain, it may be several weeksuntil you begin to feel the benefit. You will be given pain-killers(either as tablets or injections) to help reduce the discomfort whilstyou are in hospital. A prescription for continued pain medication willbe given to you for your discharge home. Please visit your GeneralPractitioner (GP) if you require further medication after that.You will probably have some bruising around the elbow and thearm may be swollen. These will gradually disappear over a periodof a few weeks.You may find ice packs over the area helpful. Use a packet of frozenpeas, placing a piece of wet paper towel between your skin and theice pack. Until the wound is healed, also use a plastic bag toprotect the wound from getting wet. Leave on for 10–15 minutesand you can repeat this several times a day.
Do I need to wear a sling?
The sling is to protect the elbow replacement. You will keep it on most of the time for the first 3 weeks. You do not need to have your arm strapped to your body. You will take the sling off for most of the exercises. If you are sitting and resting you may take the sling off if you wish. The therapists and nurses will show you how to use the sling.You will gradually wear the sling less after 3 weeks, but you may find it takes 6 weeks or more, before you are without it all the time.You may find it helpful to wear the sling at night (with or without the body strap), particularly if you tend to lie on your side.Alternatively you can use pillows in front of you to rest your arm on. In addition if you are lying on your back to sleep you may find placing a thin pillow or folded towel under your arm will be comfortable.
Physiotherapy rehabilitation
You will be shown exercises by the physiotherapist. You will start exercises to move the elbow, as well as your shoulder, wrist and hand on the first day after the operation. You will then need to continue with exercises when you go home. Outpatient physiotherapy is not routine, but will be organised if it is felt to be necessary in your case.You will need to get into the habit of doing regular daily exercises at home for several months. They will enable you to gain maximum benefit from your operation.The exercises aim to stop your elbow getting stiff and strengthen muscles.
Wound healing
Keep the wound dry until it is healed. This is normally for 10–14days. You can shower or wash and use ice packs but protect the wound with cling-film or a plastic bag. Avoid using talcum powder or perfumes near or on the scar.Normally your clips (or stitches) will be removed by the nurse after 10 days of your surgery.
Things should be avoided after surgery
For 6 weeks. Do not try and push or force your elbow straight.For example, pushing through your arm to get from sitting to standing, pushing a door open, polishing surfaces. This is because the muscle (triceps)has been cut and re-stitched in the operation. It takes time to heal before you can put force through it. Even after 6 weeks, take care of this action. However, it is important you do practice trying to straighten your arm as the therapist shows you, just don’t use your muscle power to do it!Try to avoid twisting the elbow with your arm out to the side.For example, reaching back to get your seat belt in a car and in the‘throwing’ (e.g. a ball) action.
For the rest of your life. It is not known exactly what may cause the elbow replacement to dislocate or become loose, but it is advised that you try to avoid:
- heavy manual work
- lifting objects with any weight(e.g. over 10 lbs)
- forceful pushing and pulling activities.
This will result in you being unable to do heavy gardening (e.g.digging). If your dominant arm has been operated on you are advised not to do sports such as bowls (or else learn to use your non dominant arm). The therapists will be able to advise you on ways to avoid unnecessary stress and strain on your elbow.
Rehabilitation Considerations:
Hematoma formation follow elbow arthroplasty can lead to pain and loss of motion in the early phases after surgery. Attempts to reduce and mobilize edema are critical in the early phases. Hematoma also increases the risk of infection which occurs in 2-3 percent of elective cases and up to 7% of cases performed for trauma.
Full flexion and extension can usually be obtained on the table but stiffness may ensue rapidly. Continuous passive motion is almost always employed when possible but patients must be encouraged to perform daily stretching exercises to preserve motion. Because the extensor mechanism must heal back to the ulna, active elbow extension, such as using the arm to assist in rising from a chair, is not permitted for 8 weeks. Adjacent joint therapy may be particularly important for patients with rheumatoid arthritis who may have concomitant disease of the shoulder and wrist.
Pre-rehabilitation:
- Instruct in application of ice and encourage use as much as tolerated within a 24 hour period for first week. If using ice packs, encourage to ice 20-30 minutes every 3-4 hours while awake.
- Instruct in home program of elbow flexion, extension, pronation and supination.
- Instruct in basic progression of rehabilitation program and expectations for time course to recovery
- Arrange follow-up physical therapy appointment on 7th-10th day post-operative to correspond with physician’s post-operative evaluation
Inpatient: (0-4 days)
- Arm is generally splinted in extension with hemo-vac drain in place for 1st 36 hours to prevent swelling and reduce chance of a hematoma. Arm is generally elevated in a sling on a pole.
- Evening of the first postoperative day, the splint is removed and patients are started on CPM set to provide full flexion and extension.
- Arm should be removed every 1-2 hours to prevent compressive neuropathy
- Cryotherapy in between sessions
ROM
- Instruct in home program, and begin, active assisted elbow and wrist flexion, extension, pronation and supination.
- Instruct in home program, and begin, self-assisted forward elevation and external rotation of the shoulder to prevent adjacent joint stiffness
- Finger ROM but no aggressive grip strengthening so that muscular attachments heal
Other:
- Instruct to don and doff sling
- Methods of edema control
- Instruct in precautions of no active elbow extension and avoid direct pressure on posterior aspect of elbow
- Instruct on proper use of ice or cryocuff 20-30 minutes at a time, several times per day, especially after exercises Arrange for outpatient physical therapy follow-up to begin on day of office follow-up
Outpatient Phase 1: (Hospital Discharge to Week 4)
ROM
Continue program active elbow and wrist flexion, pronation and supination and active assisted elbow flexion.
Continue shoulder flexibility exercises
Strength
Can start gentle grip strengthening but no active elbow or wrist strengthening exercises until Phase II Sling
Sling
should only be used when patients are out in busy or crowded
locations but not around the house and not to bed
Other
Incision mobilization and desensitization
Modalities for pain, inflammation and edema control (no e-stim)
Cryotherapy as needed
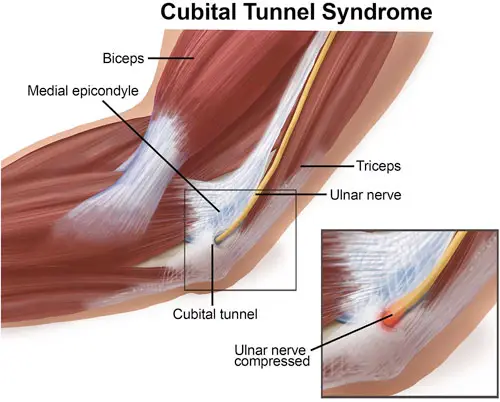
Ulnar nerve desensitization
Outpatient Phase 2: (Weeks 5-8)
ROM
Continue shoulder elbow and wrist ROM
At 6 weeks can add active extension (anti-gravity only but no resistance)
Night time extension splinting if flexion contracture developing
Strength
May begin gentle isometric and isotonic wrist flexion/extension and elbow flexion strengthening
Biceps strengthening should be done with elbow supported
No elbow extension strengthening
Sling
Sling should be fully discontinued at this point Other
Continue scar massage
Outpatient Phase 3: (Weeks 9 -12)
ROM
Active range of motion in all planes
Continue night time extension splinting if necessary
Dynasplint if flexion contracture >30o
Strength
Continue isotonic strengthening
May add anti-gravity active extension but no resistance
May add UBE at very low resistance for conditioning
May add exercises for shoulder to promote generally upper extremity conditioning
Outpatient Phase 4: Weeks 12 – 16)
ROM
Continue maintenance flexibility program
Strength
Progressive isotonic resistance including elbow extension
Progress to functional use
When can a patient return to work?
You will probably be off work approximately 6–8 weeks, depending on the type of job you have. If you are involved in overhead activities you are advised not to do these for 3–6 months. You maybe advised to change your employment if you have to do lifting or heavy manual work. Please discuss any queries with the therapists or hospital doctor
When can a patient drive?
It is normally about 6–8 weeks before you can do this safely. You may find it is more difficult if your left arm has been operated on because of using the gear stick/handbrake. Check you can manage all the controls and it is advisable to start with short journeys.
When can a patient participate in leisure activities?
Your ability to start these activities will be dependent on pain,range of movement and strength that you have in your elbowfollowing the operation. Please discuss activities that you may beinterested in with the therapists or hospital doctor. Start with shortsessions, involving little effort and gradually increase. General examples:•Swimming – after 6 weeks•Gardening (light tasks e.g. weeding) – after 6–8 weeks
Guide to daily activities in the first 6 weeks
Some difficulties are quite common, particularly in the early stages.The occupational therapist (O.T.) will help you to be as independent as possible during your rehabilitation. Special equipment can be borrowed from the O.T. department. Often other joints may be causing problems with pain and stiffness.Everyone is different so your individual needs will be assessed. We appreciate that you may have been having many of these problems before your operation. Please discuss your difficulties with the occupational therapist.
- Getting on and off seats.Raising the height can help. e.g.extra cushion, raised toilet seat, chair or bed blocks. Remember we would like you to avoid pushing up from a chair using your operated elbow.
- Getting in and out of the bath.Using a bath board may help although initially you may prefer to strip wash.
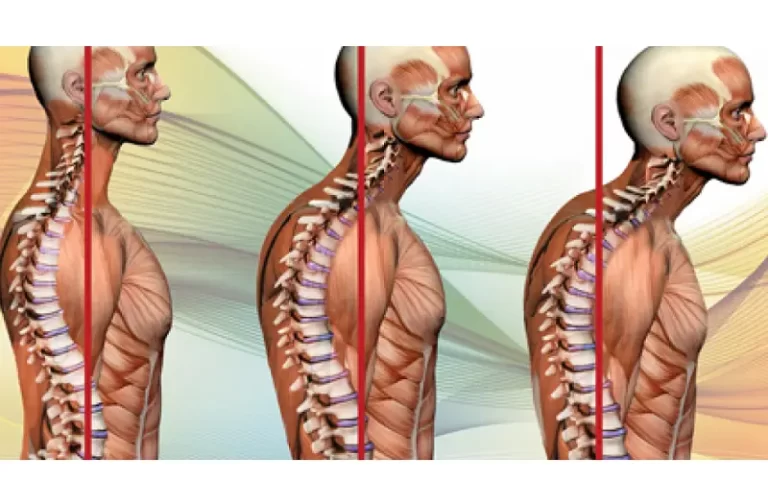
- Hair care and washing yourself.Long handled combs, brushes and sponges can help to stop you using your arm overhead. You may need some help to wash your hair. Have your head down if possible.
- Dressing.Wear loose clothing, either with front fastening or that you can slip over your head. For ease also remember to dress your operated arm first and undress your operated arm last. In addition dressing sticks, long handled shoe horns, elastics hoe laces and a ‘helping hand’ can help.
- Eating.Use your operated arm as soon as you feel able for cutting up food and holding a cup. A non slip mat and other simple aids can help.
- Household tasks/cooking.Do light tasks at waist level as soon as you feel able e.g. lift kettle with small amount of water, light dusting, ironing. Remember not to push your arm straight for the first 6 weeks. There are various gadgets that can help you
Exercises
Use pain-killers and/or ice packs to reduce the pain before you exercise.
It is normal for you to feel aching, discomfort or stretching sensations when doing these exercises.
However, if you experience intense and lasting pain (e.g. more than 30 minutes), i tis an indication to change the exercise by doing it less forcefully, or less often. If this does not help, discuss the problem with the physiotherapist.
Certain exercises may be changed or added for your particular elbow.Do short, frequent sessions(e.g. 5–10 minutes, 4 times a day)rather than one long session.
Gradually increase the number of repetitions you do.
Aim for the repetitions your therapist advises,the numbers stated here are rough guidelines.
After 3–4 weeks you can increase the length of time exercising.Get into a habit of doing them.
NB. Exercises shown for right arm, unless specified.
Phases 1 & 2From operation day for 6 weeks
Neck exercises

- Standing or sitting.
- Tilt your head towards one shoulder. Repeat 5 times.
- Then turn your head to the other side and repeat 5times.
- Then tilt your head to the other side and repeat 5times.
- Turn your head to one side.Repeat 5 times.
Shoulder blade exercises
Sitting or standing.
- Keep your arms relaxed.
- Shrug your shoulders up towards your ears. Then let them relax.
- Repeat 5 times.
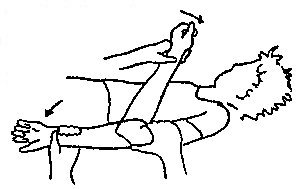
Shoulder exercises Stand leaning forwards. (Keep sling on initially.)
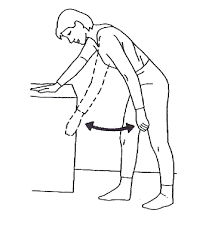
- Let your arm hang down.
- Swing your arm forward and back, side to side and round in a circle.
- Progress to doing exercise without sling.
- Repeat 5 times.(Shown for without sling.)
Lying on your back on the bed. (Keep sling on initially.)
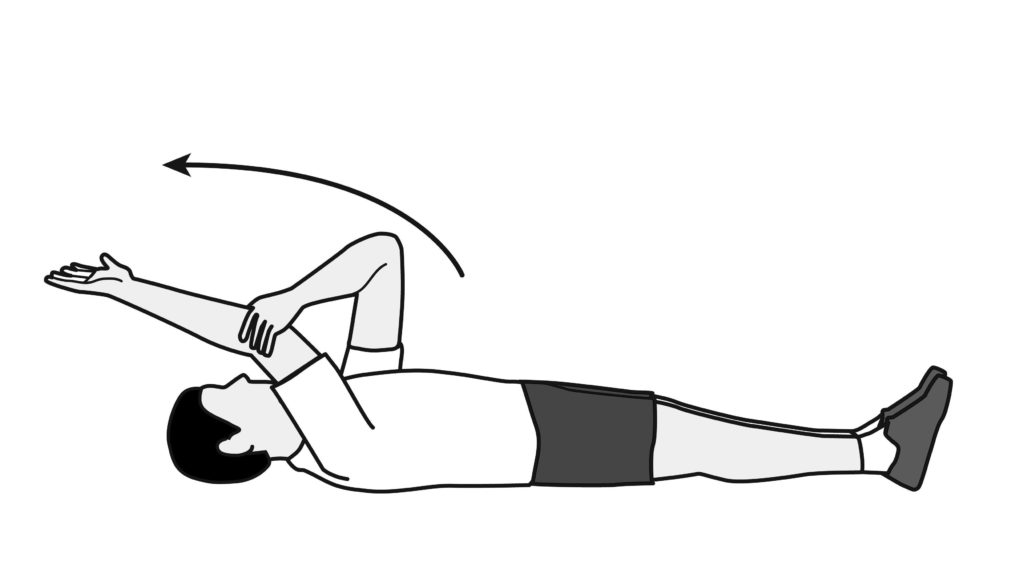
- Lift your operated arm up with your other arm,aiming to get it over your head.
- keep your elbow straight.
- Repeat 5 times.
Standing with arm by side
- Keep the arm by your side but twist it outwards trying to make the palm face forwards.
- Repeat 5 times.
Wrist exercises
- Keep your arm in the sling or rest your forearm on a flat surface.
- Keeping your forearm still, move your hand up and down,bending at the wrist.
- Do this with your fingers straight and bent (i.e. with a fist and without).
- Repeat each 5 times.
Elbow exercises
Rotating
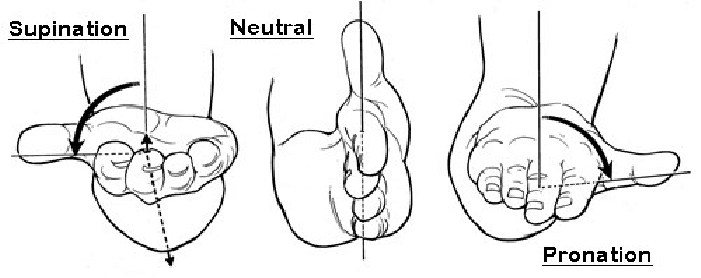
- Rest your forearm on a flat surface.
- Try and turn your palm up towards the ceiling.
- Then turn palm down.
- Repeat each movement 5 times
Bending and straightening.
- These exercises are important, especially the bending part.
- It can be done in different positions.
- The therapist will help you to find the most useful for you.
- Lying on your back, arm supported.
- Let your arm go straight.DO NOT PUSH it straight.Just ‘let it go’.
- Repeat 5 times.
- Lying on your back.
- Rest upper arm on bed on small pillow.
- Use your other arm to help your hand towards your mouth.
- Gradually do this without using the other arm for help.
- Repeat 5–8 times.
Standing

- Let your arm relax down straight. Do not push it.
- Repeat 5 times
- Bend your elbow, trying to take your hand towards your mouth,with the palm facing you.
- Repeat 5 times.
Standing (arm behind your back)

- Try and take your hand behind your back with the help of your other hand.
- Repeat 5 times.
Phases 3 & 4 (6 weeks after your operation)
You can now start using the triceps muscle.
Lying down
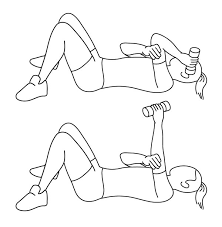
- Rest your hand on your forehead.
- Then try and straighten your arm up in the air.
- Repeat 5 time.
- do it with weight for strengthening.
Weight bearing on Affected arm

- Standing or Sitting
- Arms by your side.
- Try and straighten your arm and then put a little weight through it.
- Do not let the arm buckle.
- Do not push hard.
- Repeat 5 times.
Elbow behind your neck
- Lift your shoulder and bend your elbow. Try and place you hand behind your head. (shown in picture)
- Standing or Sitting

NOTE : Do exercises that you feel will help you to do the things that you wish to do in your life. Not all of these exercises may be required. Do not do weight lifting type exercises unless directed by a therapist. If the movement does not change within 12 weeks, it may not change further. This will be the movement that you will have for daily activities.





4 Comments