Trendelenburg Gait
What is Trendelenburg’s Gait?
Trendelenburg gait is a dysfunctional gait brought on by a broken hip abductor mechanism. The gluteal musculature, which includes the gluteus medius and gluteus minimus muscles, is the main group of muscles involved. When walking, the pelvis drops to the opposite side due to the weakening of these muscles. This session examines Trendenlenburg gait examination and management and emphasizes the contribution of interprofessional team members in providing well-coordinated care and improving patient outcomes.
How it occurred?
The pubic symphysis is where the body’s center of gravity lies. The pelvis tends to drop to the unsupported side when one foot lifts off the ground, as it does during the swing phase of the gait cycle. The body remains unsupported on that side. The supported side’s abductor muscles, particularly the gluteus medius, and minimus, contract to prevent the drop, stabilizing the overlaid boot. The pelvis will droop on the side opposite the pathology if there is any injury to the hip and its abductor mechanism as a result of the causes outlined above.
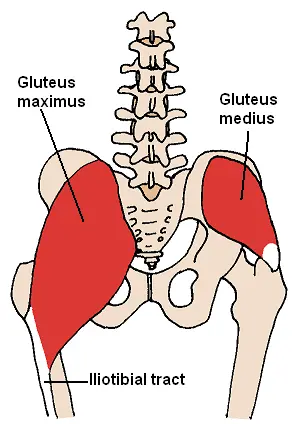
Anatomy
The acetabulum and femoral head make up the hip joint. Twenty-two muscles and soft tissues surround these structures. The femur may move during activity because of the stability and force provided by these muscles.
The two primary hip abductors, gluteus medius and gluteus minimus sustain the pelvis’ opposition and prevent the pelvis from falling. The L4-S1 nerve roots make contributions to the superior gluteal nerve. This nerve travels through the sciatic notch in the pelvis and supplies the tensor fascia lata, gluteus medius, and minimus muscles as well as the hip joint.
Neuromuscular Abnormalities
The following are some instances of neuromuscular disorders that might cause Trendelenburg’s sign:
Injury to the superior gluteal nerve is frequently caused by trauma or iatrogenic after a total hip replacement or hemiarthroplasty.
The superior gluteal nerve, which is generated from the L4, L5, and S1 spinal roots, is frequently accompanied by foot drop in L5 radiculopathy.
Weakness or injury to the gluteus medius and minimus (such as tears or tendinitis)
Hip abductors become paralyzed as a result of poliomyelitis.
Other neuromuscular diseases and muscular dystrophy
Inhibiting pain can cause gluteal weakness (such as hip osteoarthritis).
How Is Trendelenburg Gait Diagnosed?
To correctly identify Trendelenburg’s gait and rule out other gait abnormalities brought on by weak hip muscles, a physical examination and review of your medical history are required. These could consist of the following:
- A painful gait
- High-stepping posture
- Lenk-extension gait
- stomping step
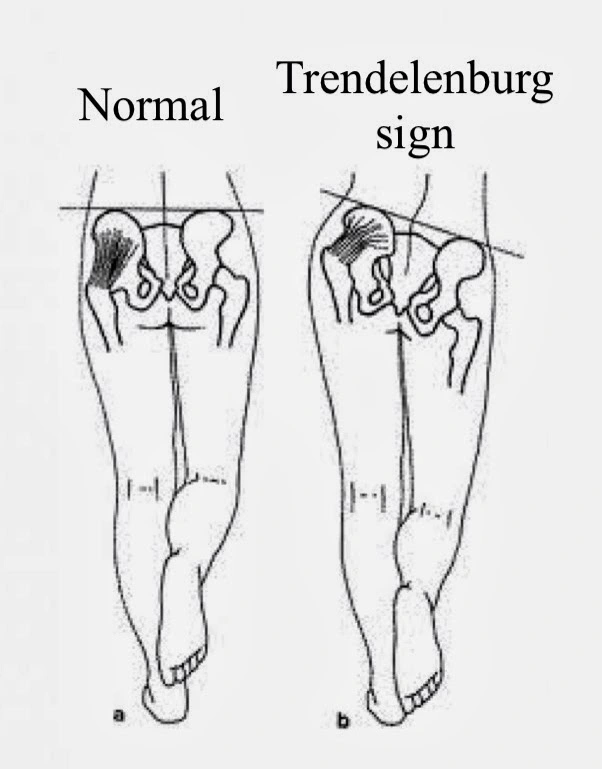
You can find out if you have Trendelenburg gait with a quick test. You will be required to stand on one leg throughout this physical assessment. An unfavorable outcome will occur if the pelvis of the raised leg tilts upward. A positive Trendelenburg sign is present if the raised leg’s pelvis tilts downward or the hip lowers.
To confirm the results of this test, an X-ray may also be used to identify Trendelenburg’s gait.
Examination
To determine whether a patient has a Trendelenburg gait, the modified McKay criteria is helpful. These parameters gauge the hip joint range of motion, gait pattern, Trendelenburg sign status, and discomfort symptoms.
| Grade | Criteria |
| Excellent | No limp, stable, pain-free hip, negative Trendelenburg sign, full range of motion |
| Good | stable, pain-free hip; a small limp; a tiny reduction in range of motion |
| Fair | Positive Trendelenburg sign, limp, stability, painless hip, restricted range of motion, or a mixture of these |
| Poor | unsteadiness or hip pain, or both; a good Trendelenburg sign |
Trendelenburg sign
A physical examination finding known as the Trendelenburg sign is used to detect hip dysfunction. The gluteus medius and gluteus minimus, which make up the hip abductor muscles, are typically weak when the Trendelenburg test is positive.
Technique
The patient is instructed to stand on one leg for 30 seconds without tilting to one side; if balance is a concern, the patient may grab onto an object. When the patient is in the single-leg posture, the therapist watches to determine if the pelvis remains level. If the pelvis lowers towards the unsupported side while carrying unilateral weight, it is a positive Trendelenburg test.
Positive Trendelenburg sign
The gluteus medius and gluteus minimus are the two hip abductor muscles that are often weak when the Trendelenburg sign is positive. These results are related to a number of hip disorders, including congenital hip dislocation, rheumatoid arthritis, and osteoarthritis.
A test is considered positive if, when standing on one leg, the pelvis on the non-affected side lowers. This can also be seen during gait: while compensating for an affected extremity, the trunk is flexed in the direction of the implicated side during the stance phase.
The test’s limitations
Early osteonecrosis may mask a positive Trendelenburg’s sign, and healthy people with a normal hip abductor mechanism but insufficient function can develop pelvic drop.8
Lack of comprehension or compliance, severe hip pain, and scoliosis (where the costal margin may impinge on the iliac crest) can all result in false positives.
Be alert for upper body movements since patients who compensate by moving their torso (and center of gravity) over the weight-bearing hip may experience false negatives.
Complications of Trendelenburg Gait
Over time, a persistent, untreated Trendelenburg gait disorder may result in secondary disease in the knees or ankles. It is also known to hasten the deterioration of the hip joint. The areas of the hip that are often not used during regular stride experience wear and tear, especially in athletes. Trendelenburg gait left untreated might result in dynamic lower extremity valgus. The boot will lean towards the affected side as a result of the unaffected side’s pelvis being lifted, which is the mechanism behind this. The resulting force from the ground will then be directed towards the lateral knee joint, resulting in a valgus knee on the side that is afflicted. This may eventually result in knee pain.
If Trendelenburg gait is your only symptom, there isn’t much reason for concern as there isn’t likely to be any short-term harm done (apart from that caused by poor balance).
The majority of the time, Trendelenburg gait can be self-corrected in the convenience of one’s own home; it infrequently necessitates in-patient physical rehabilitation.
What Are the Long-Term Consequences of Trendelenburg Gait Untreated?
Your knees and ankles may develop long-term issues if you have a chronic Trendelenburg gait that is not corrected. Additionally, it hastens the progression of degenerative arthritis. The hip joint experiences “wear and tear” in places that aren’t often impacted by a typical stride.
Trendelenburg gait, if left untreated, can result in a severe elevation of the pelvis on the unaffected side. Over time, this ultimately results in the knee joint bending outward, which causes knee discomfort. Pinched nerves, hip grinding, the requirement for a walker or wheelchair, and bone tissue loss are among the more potential side effects of an untreated chronic Trendelenburg gait.
Physiotherapy Treatment of Trendelenburg Gait
You might be able to control your gait and lessen the side-to-side motion with the help of physical treatment. Osteopathic manipulative therapy is frequently used in physical therapy for this gait (OMT).
Your doctor will move your legs in different directions during OMT using your hands. This can improve your muscular strength and resistance and help your joints get used to moving in particular directions.
The following additional exercises can help your hip abductor muscles:
Extending your leg straight out while lying on your side. Moving one leg up, over the other, and back the other way while squatting. Stepping sideways up onto an elevated surface, then stepping back down.
Bending your lower leg, raising your knee, extending it, and swinging the extended leg backward cause you to lean forward.
These are some Trendelenburg gait exercises to strengthen your hip abductors. For all of these workouts, a resistance band is required. One can be found anywhere that sells exercise equipment, including sports goods stores.
Side plank

Side planks are a unilateral isometric exercise that is very successful for treating Trendelenburg gait brought on by a hip flexor muscular imbalance, especially when dynamic movement throughout the muscle group’s range of motion is restricted because of injury or aging.
Technique:
The exerciser should be on their side on a yoga mat with the opposite leg resting on the lower leg that is on the ground, and the torso should be supported by the forearm and elbow on the same side.
The exerciser will start by aligning their body in a straight line, flexing their abdominal muscles, and balancing for a set period of time on their feet and elbows.
The exerciser will switch to the opposite side to finish the repeat whenever enough time has passed on the first side.
Resisted side steps

Resisted side steps may be performed in Trendelenburg gait cases where the patient is mobile and strong enough to carry out resisted exercise in order to rehabilitate the hip abductors.
The exercise is performed standing up, and it will take some stability in the lower body to keep your balance even when you add resistance close to your ankles or knees.
They may be conducted with a resistance band or machine, but they should still be done at very low resistance to prevent any unwanted repercussions for the patient.
Technique:
While standing straight up with a resistance band around the knees or ankles, the exerciser will lower themselves into a half-squat position by tightening their abdominal muscles and bending at the hips and knees, which will cause their torso to sag slightly forward.
The legs must be kept apart enough to maintain tension in the band, and the steps must be brief enough that the unaffected leg does not need to make bigger movements to make up for the affected limb. The hip abductor muscles must be effectively rehabilitated while the trunk is vertically parallel to the floor and upright.
The exerciser will carefully walk to the side with the injured leg while in this half-squat position, making sure that the hip abductors are correctly tensed. The repetition ends after the opposing leg does the same.
Bridging

Generally requiring little to no equipment, glute bridges are a popular exercise for their combination of isometric and dynamic muscular contraction of the various muscles responsible for Trendelenburg gait. They are also thought to be quite effective at treating posterior chain or hip flexor weakness in otherwise healthy individuals.
Hip abduction

The laying side hip abduction exercise is a rehabilitation exercise designed to focus on the hip abductor muscles of the affected side, whether it is carried out with a resistance band loaded or without any tools.
Technique
Lying on one side, you will fully extend your knee until it is parallel to the floor, then raise it at the hip in an upward motion. They will stop when they have reached the limit of their hip abductor’s range of motion.
The difficulty of the movement can be substantially reduced for exercisers who are unable to perform this, allowing them to go to the fully-extended variation of the exercise. This can be done by keeping the feet together and raising the leg at the knee instead of fully extending it.
FAQ
How is the Trendelenburg gait reversed?
Your knees should be straight and your feet should be stacked and supported on the ground. Start the exercise by pushing your hips as far up and forward as you can while maintaining the position. Then, while keeping your upper leg straight and in line with your torso, raise it towards the ceiling, drop it, and repeat.
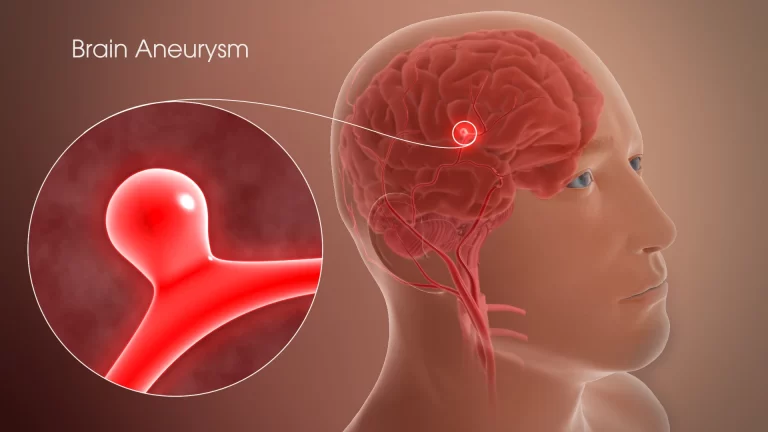
How dangerous is the Trendelenburg position?
Alterations in pulmonary function, airway edema, elevated intracranial and intraocular pressure, and nerve injury are among the risks connected to a steep Trendelenburg posture.
When to Refrain from Working Out with a Trendelenburg Gait?
Exercise is one of the best ways to treat a Trendelenburg gait brought on by muscular weakness, but certain other causes can actually have quite the opposite impact when activity is involved, perhaps making the movement problem worse or causing even more symptoms to appear.




One Comment