Triangular Fibrocartilage Complex(TFCC) Injury
Introduction
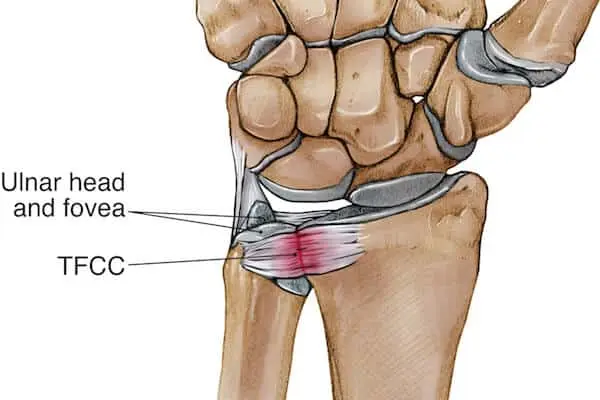
The Triangular Fibrocartilage Complex (TFCC) is a critical structure located in the wrist joint. Comprising a combination of cartilage, ligaments, and tendons, the TFCC plays a pivotal role in stabilizing the wrist and facilitating its smooth movement.
Injuries to the TFCC can result from traumatic events, such as falls or sports-related impacts, as well as from chronic wear and tear over time. These injuries can lead to pain, instability, and limited range of motion in the wrist. Diagnosing and treating TFCC injuries require a comprehensive understanding of the complex anatomy and function of this vital wrist structure.
What is triangular fibrocartilage(TFCC)?
There is a structure that lies between the lunate, triquetrum, and ulnar head which is a load-bearing structure called the triangular fibrocartilage complex (TFCC). The work of the TFCC is to act as a stabilizer for the ulnar side of the wrist.
TFCC carries a risk of acute or chronic degenerative impairments. Both forced ulnar deviation and positive ulnar variation are associated with TFCC injury.
Patients with TFCC injury will present with ulnar-side wrist pain, which may manifest as a click or pain point between the pyramidal head and the ulnar head. TFCC is associated with a distal radius fracture in 39-84% of cases.
Causes of TFCC Injury
Occurs when there is a significant ulnar deviation and compressive stress on the TFCC.
Often linked to radial shortening, measuring an average of 4.5 mm, and positive ulnar variation.
Increased strain is placed on the TFCC by forced ulnar deviation, such as swinging a bat, racket, etc.
Triangular Fibrocartilage Complex (TFCC) injuries can arise from various causes, ranging from acute traumatic incidents to chronic wear and tear. Some common causes of TFCC injuries include:
- Falls: Landing on an outstretched hand during a fall can transmit excessive force to the wrist, leading to TFCC injuries. The impact can cause tearing or damage to the ligaments and cartilage within the TFCC.
- Sports Injuries: Activities that involve repetitive wrist motions or direct impact, such as tennis, golf, or gymnastics, can increase the risk of TFCC injuries. Sudden twisting or loading of the wrist during these activities can strain or tear the TFCC components.
- Workplace or Occupational Factors: Professions that require repetitive wrist movements, heavy lifting, or prolonged weight-bearing on the wrist can contribute to TFCC injuries over time. Mechanics, carpenters, and manual laborers are examples of individuals who may be at higher risk.
- Degenerative Changes: Chronic degeneration of the TFCC can occur naturally over time due to the aging process. This can lead to weakening of the ligaments and cartilage, making the TFCC more prone to injury even from minor trauma.
- Distal Radius Fractures: Fractures of the distal radius (wrist bone) can sometimes involve the TFCC. The impact that causes the fracture can also damage the adjacent TFCC structures.
- Wrist Instability: Pre-existing wrist instability, often due to ligament laxity or prior injuries, can increase the susceptibility of the TFCC to injury. Instability places additional stress on the TFCC during wrist movements.
- Overuse and Repetitive Stress: Activities that involve frequent and forceful wrist movements, such as typing or using handheld tools, can lead to overuse injuries of the TFCC over time.
- Ligament Tears: Tears of other wrist ligaments, such as the ulnar collateral ligament, can alter the biomechanics of the wrist and indirectly contribute to TFCC injuries.
- Arthritis: Conditions like rheumatoid arthritis or osteoarthritis can cause inflammation and degeneration of the wrist joint, affecting the health and integrity of the TFCC.
It’s important to note that the severity and type of TFCC injury can vary based on the cause and the specific structures affected.
Pathophysiology
The ligamentous and cartilaginous structures that divide the distal radioulnar joint from the radiocarpal joint are known as the triangular fibrocartilage complex. The extensor carpi ulnaris sheath, dorsal & volar radioulnar ligament, ulnocarpal ligament, meniscus homolog, and articular disc make up the TFCC.
The ulnocarpal collateral ligament, meniscal homolog, lunotriquetral and ulnolunate ligaments, dorsal and volar distal radioulnar ligaments, and triangular fibrocartilage disc are all anatomical components of the TFCC. In contrast to the bone attachment on the ulnar side, the triangular fibrocartilage disc attachment on the radial side is attached to hyaline cartilage, making it weaker.
When there is positive ulnar variation, the TFCC is more susceptible to harm. Supination causes a decrease in ulnar variation, whereas pronation causes a rise. The amount of load on the ulna has been demonstrated to be significantly affected by small variations in ulnar length.
Because the extensor carpi ulnaris depends on the TFCC for movement, a change in that muscle’s action might cause the TFCC to be subjected to unusual force and put it at risk for damage.
Mechanism of the TFCC injury
When a load is forced into the TFCC with the wrist in ulnar deviation, TFCC injury frequently results. Swinging a bat or a racket is one of the most common causes of forced ulnar deviation. A positive ulnar variance, which occurs when the articular surface of the ulna is further distal than the articular surface of the radius, is also linked to TFCC damage. Surgical or other earlier procedures frequently cause positive ulnar variance.
The ulnocarpal collateral ligament, meniscal homolog, lunotriquetral and ulnolunate ligaments, dorsal and volar distal radioulnar ligaments, and triangular fibrocartilage disc are all anatomical components of the TFCC. The radial side’s triangular fibrocartilage disc connection is to hyaline cartilage, making it weaker than the bony attachment on the ulnar side.
When there is positive ulnar variation, the TFCC is particularly prone to harm. Supination causes a decrease in ulnar variation, whereas pronation causes a rise. The amount of load on the ulna has been demonstrated to be significantly affected by small variations in ulnar length.
Because the extensor carpi ulnaris depends on the TFCC for movement, a change in that muscle’s action might cause the TFCC to be subjected to unusual force and put it at risk for damage.
- Origin: Distal radius’ medial boundary
- Based on the ulnar styloid insertion
- Vascular Supply: The TFCC edges are perforated by peripheral blood arteries, while the core disc is avascular.
- The TFCC serves as the primary stabilizer of the distal radioulnar joint; its volar portion inhibits ulna displacement to the dorsal and is tight in pronation, while its dorsal component prevents ulna displacement to the volar and is tight in supination. stabilizes the ulnocarpal joint.
Epidemiology
According to one study, the frequency of TFCC injuries rises with age. In patients aged 70 or older, the frequency was 49%, whereas, in patients aged 30 or younger, it was 27%.
The frequency of TFCC damage was also shown to be similar in patients with ulnar-sided pain compared to individuals who underwent wrist imaging for reasons other than ulnar-sided pain in a different research that revealed a similar prevalence in participants younger than 30. According to this study, not all TFCC problems result in ulnar-sided discomfort or fractures.
Histopathology
The following is a breakdown of the histology of the TFCC’s constituent parts:
Triangular fibrocartilage disc: fibrocartilage that is avascular and only has blood vessels on the ulnar side.
Extensor carpi ulnaris tendon sub-sheath: parallel collagen that is both flexible and rigid.
The ulnolunate and lunotriquetral ligaments are made up of parallel collagen fibers that are both loose and tight. Less elastic fibers make up the ulna-lunate than the lunotriquetral. Parallel collagen bundles make up the dorsal and volar distal radioulnar ligaments.
The majority of the meniscal homolog is made up of loose connective tissue.
Symptoms of TFCC Injury
Patients will express discomfort in their ulnar wrist, which frequently worsens with activity.
Additionally, there can be clicking, instability, or grip brittleness.
Acute injuries particularly to baseball can result from forceful wrist extension when sliding head-first or when a batter attempts to hit an inside pitch and gets “jammed.” These are just a few examples of how certain aspects of history might arise in connection with specific sports.
Baseball players are susceptible to chronic injuries because of the strain the swing puts on the wrist. Even if these athletes do not exhibit positive ulnar variance, they are nevertheless susceptible to TFCC problems.
In gymnastics, both support skills and hanging aspects can cause overuse injuries to the TFCC. This region can become inflamed with repeated weight bearing (both compressive and tensile), and tendonitis/tendinosis can form in the anchoring wrist ligaments (commonly misinterpreted as a wrist injury).
Diagnostic Procedures
Physical Examination TFCC Stress Test
- When performing an exam, pronating the wrist is best for palpating the TFCC. Between the ulnar styloid, flexor carpi ulnaris, and the os pisiform, it is located. The diagnosis of TFCC injury may be suggested by a number of physical exam tests. These consist of:
- The forearm in a neutral position with ulnar deviation reproduces symptoms in the TFCC compression test.
- TFCC stress test: reproducing symptoms by exerting strain across the ulna with the wrist deviated.
- Press test: The patient extends their wrists to pull himself out of a chair. Pain is a sign of a successful exam.
- Supination test: Holding a table’s underside with the forearms in a supinated posture, the patient applies pressure on the TFCC, resulting in painful dorsal impingement, if there is a peripheral, dorsal tear.
- Piano test: Put both hands on a table and put your palms down to practice your piano abilities. If the distal ulna is prominent on the side that is damaged, this may be a sign of TFCC injury-related distal radioulnar joint instability. This is a successful test if the palms are relaxed and the ulnar head returns to its original position.
- Grind test: Rotate the patient’s forearm while compressing the radius and ulna. Pain could indicate a degenerative process.
Diagnostic Imaging
Avulsion injury of the ulnar styloid, scaphoid fracture, distal radial fracture, volar tilt of the lunate or triquetrum bone, and ulnar variance may all be observed on X-Ray.
- Triple injections Arthrography: low specificity tear identification.
- MRI: excellent sensitivity and specificity for identifying tears.
Surgical Intervention
If non-surgical measures are unsuccessful or there is DRUJ instability, surgical options should be taken into account. Surgical intervention will rely on the injury’s Palmer categorization.
The Palmer classification is the most widely used classification system for TFCC lesions. It separates them into two groups (with additional subgroups that are outside the scope of this article: Degenerative and Traumatic. This classification offers a precise anatomic description of tears; it does not, however, suggest a course of action or offer a prognosis.
The Palmer classification of the injury, covered in the staging section, will determine the surgical course of action.
Palmer classification
- 1A: If this injury is left untreated, it will not heal because it is in an avascular area. Debridement is the preferred strategy because it does not respond to direct surgical care due to its lack of vascularity.
- 1B: A direct surgical repair is an option because the area contains vascularization. The radioulnar ligaments are injured and there will be instability if the triangular fibrocartilage disc entirely separates from the ulnar insertion.
In this situation, the tendon’s degree of retraction should be assessed, and a tendon transplant can be required as part of the surgical repair. Partial tears would not result in radioulnar ligament damage, making them stable and amenable to arthroscopic suturing. Tears at the foveal insertion need to be surgically repaired, making them more serious than tears at the styloid insertion.
- 1C: Two options are arthroscopy and debridement. If the ligaments cannot be repaired, a debridement is an alternative.
- 1D: Surgical reattachment is the preferred course of treatment when the injury involves damage to the radioulnar ligament. Partial resection with arthroscopy is a possibility if the radioulnar ligaments are unharmed by the lesion.
Whether the lunotriquetral ligament is damaged or intact determines how a type 2 lesion should be treated. Although CT arthrography also works well for this purpose, MR arthrography is the preferred method. Lesions of types 2A, 2B, and 2C may benefit from cautious treatment. If conservative care is unsuccessful, the Wafer surgery, which involves resecting the distal portion of the ulnar head, is a viable next option. Resection of the ulnar head is another treatment option for type 2E lesions. Treatment for type 2D lesions involves osteotomy and ulnar shaft shortening.
Studies and procedures for better rehabilitation
- One research of 57 patients who had chronic tears and had discomfort for, on average, nine months before surgery discovered a 98% satisfaction rate and a nine-week return to work for these patients.
- The Wafer procedure, ulnar shortening, arthroscopic repair, and arthroscopic debridement are common surgical alternatives.
- A surgical procedure called debridement causes bleeding to promote healing. Debridement has beneficial outcomes for central.
- TFCC tears, but it has been demonstrated that patients with degenerative tears or higher positive ulnar variation have worse outcomes.
- A radiocarpal joint that is rheumatic or a lunate and scaphoid ligament that is insufficient are contraindications to arthroscopy.
Treatment for non-athletes may be different from treatment for athletes. An athlete in high school who won’t continue competing until graduation should start with four weeks of rest, ice, and anti-inflammatories. For elite athletes, one week of rest with splinting and re-examination after one week is suitable if there is no distal radioulnar joint instability. It could be detrimental to one’s career if the TFCC is torn together with instability in the distal radioulnar joint.
If non-surgical treatment is chosen, this could involve immobilizing the long arm for three weeks, the short arm for three weeks, and then gradually returning to play. If there is a persistent tear, the athlete can be advised that there is little chance of more harm. Therefore, the athlete has two options: have surgery right away or try to play through the injury until the end of the season. Additionally available are corticosteroid injections, particularly for professional athletes who choose to postpone surgery in an effort to finish the season.
Staging
The Palmer classification is used to classify TFCC injuries. Grade 1 is trauma and Grade 2 is degenerative. All type 2 lesions are likely to be associated with positive axial variance. Each class is further subclassed:
- 1A: The central surface of the triangular fibrocartilage disc is perforated. Since the ulnar ligaments are intact, these are stable injuries.
- 1B: Injury to the attachment part of the triangular fibrocartilage disc. This lesion is not communicated on arthrography.
- 1C: Distant TFCC disturbance. In this case, there was the separation of the lunotriquetral and palmar ulnolunate ligaments of the carpal tunnel attachment.
- 1D: damage to the triangular fibrocartilage disc’s radial connection. These lesions are conveyed on MRI arthroscopy.
- 2A: Triangular fibrocartilage discs undergoing degenerative alterations without showing signs of perforation.
- 2B: Grade 2A with additional presence of cartilaginous malacia of transparent cartilage on the joint surface.
- 2C: The triangular cartilage disc was perforated in its full thickness.
- 2D: One of the features of 2A to 2C plus a tear in the lunotriquetral ligament.
- 2E: Grade 2D with ulnocarpal arthritis also present.
Outcome Measures
- DASH Outcome Measure
- Modified Mayo Wrist Score
- Activities of Daily Living Score
- Management / Interventions
- Conservative Treatment
The rehabilitation program should include rest, activity modification to remove trauma stimulus, ice application, and splint immobilization for 3 to 6 weeks. After immobilization, the patient should receive physical therapy.
Physiotherapy
Rest, physical therapy, and corticosteroid injections are all part of the starting treatment.
Time to try conservative treatment before moving on to different surgical options.
If the distal radial joint is not unstable, six months of conservative therapy are attainable.
Post-Operative Rehabilitation
Recovery from surgery varies, but usually takes four to six weeks for arthroscopy and about three months for open methods. The patient will undergo physical therapy after the procedure. The type of surgery being performed and the surgeon’s preferences determine the precise start date and duration of physical therapy.
For type 1 injury
The wrist will be immobilized for 1 week after arthroscopy.
After a week, range of motion exercises can be started.
Golf, boxing, tennis, water skiing, gymnastics, pole vaulting, and hockey are all sports that frequently result in TFCC tears. Golf and tennis players with a stable TFCC tear can begin mild ball-contact activity 3 weeks after arthroscopy. They can resume normal sports activities after 4 to 6 weeks.
When symptoms persist, ulnocarpal corticosteroid injections may be an option.
For more serious injuries, postoperative 4 week Muenster cast immobilisation may be recommended.
After 4 weeks:
The wrist is placed in a short arm brace or a Versa wrist brace, allowing gradual movement toward the wrist.
Immobilization will reduce wrist pain and worsening of the condition, which can improve healing.
Some types of splints will help immobilize the wrist, helping to improve hand function. The patient can then begin with motion and grip-strengthening exercises.
The co-activation of the wrist flexor pattern, which stabilizes the wrist, can be affected by eccentric grip strengthening activities, which therapists are more likely to suggest. Other co-activation exercises may also be included to improve overall wrist stability.
After 8 weeks postoperatively:
Active muscle training has to be initiated.
A grade-vise, pain-free exercise program is recommended.
Physical therapy management should include patient education and activity modification. Isometric exercises should be included to help strengthen the region and reduce the risk of instability. In particular, unilateral isometric exercises are beneficial because they increase bilateral voluntary muscle activation. This may be because the motor cortex is stimulated, leading to better neuromuscular control. In addition, controlled isometric activation of the pronator quadratus in the supine and neutral wrist position helps stabilize the distal radial joint (DRUJ). This can be used before and after surgery in patients with TFCC lesions.
At 3 months:
After surgery, the patient is able to resume normal activities. It takes another 3 to 4 months to resume normal sports activities.
Passive Mobilisation
Initially, traction of the wrist and mid-carpal joints may be used to determine if this is causing pain.
To promote flexion of the wrist, the back glide technique can be used.
The palmar sliding method can be applied to encourage wrist extension.
Using the ulnar sliding approach can encourage radial deviation.
To promote ulnar deviation, the radial sliding technique can be used.
General Mobility Exercises
Patients should perform joint mobility exercises:
- Wrist rotations.
- Ulnar and radial transverse deviation.
- Active pronation and supination of the forearm.
- Flex the wrist and straighten the wrist(flexion-extension)
- Strengthening exercises
- At the end of therapy, then move on to strengthening exercises. All of the following exercises are performed with dumbbells in your hands or with a terra tire.
- Pronation and supination.
Differential Diagnosis
- Hypothenar hammer syndrome: It’s necessary to distinguish between the two since the fourth or fifth finger may exhibit discolouration, ulceration, or bleeding from splinters. Angiography can diagnose this condition.
- Carpal Ulnar Impingement: It should be differentiated because this is often the result of shortening of the ulna due to surgical resection of a previous injury.
- Tendonitis of the extensor or flexor muscle: Movements that cause muscles to work will cause pain. The pain may radiate along the abdominal muscles depending on the degree of inflammation.
- DRUJ chondral lesions or osteoarthritis: Distinguish by radiographic evidence suggesting cartilage injury or osteoarthritis.
- Ulnar Styloid Impingement Syndrome: Although there were signs that were typical of TFCC damage, the TFCC is unharmed.
Complications
Complications are mainly related to surgical management. Postoperative complications include but are not limited to, infection, hypertrophic scarring, tendon damage, nerve damage, reflex sympathetic dystrophy, and stiffness with limited range of motion.
Postoperative and rehabilitation care
Recovery from surgery varies, but usually takes four to six weeks for arthroscopy and about three months for open methods. The patient will undergo physical therapy after the procedure. The type of surgery being performed and the surgeon’s preferences determine the precise start date and duration of physical therapy. If osteotomy is performed to shorten the ulna, the patient will be immobilized for about 4 weeks before starting a series of mobility exercises.
Grip strength is one way to determine when to start strength exercises. Grip strength is estimated to be 10% higher in the dominant hand. Once grip strength reaches 80% of the expected normal range, the athlete can begin strengthening exercises and gradually return to competition. If surgery on the throwing arm is performed, elite athletes can resume competition after 8 to 12 weeks. If surgery on the arm doesn’t throw, you can return to play in 6 to 8 weeks.
Prevention and patient education
Patients should be educated to avoid activities that cause pain as soon as they first notice pain. If rest and strengthening exercises are started promptly, this increases the chances of preventing disease progression.
Other Issues
The pitfalls in diagnosing TFCC injuries are largely related to MRI misreading. Here are some examples of common errors when reading an MRI:
Anterior styloid is a normal wrist structure near the ulnar styloid that is filled with fluid and can often be mistaken for a sign of trauma or tumor. Cartilaginous tissue at the level of the ulnar styloid may have a signal intensity that may be misinterpreted as a partial tear. The subquantum ligament is a normal structure at the ulnar insertion of a triangular fibrocartilaginous disc that is typically highly signal-intensity.
Similarly, the triangular fibrocartilage disc’s radial connection is a healthy structure that shows up on an MRI with a high signal intensity. None of these should be confused with an injury.
Another complication associated with an MRI reading includes if the wrist is rotated during the imaging time. If so, the central disc may appear thin on the coronal plane. As long as there are no significant signs other than a thin-looking disc, it is not pathological.
An intermediate signal in the central disc may indicate intrinsic degeneration rather than tear. Chondrocalcinosis can also resemble class 2 Palmer’s lesions. If this is suspected, a CT scan before diagnosing a TFCC tear is appropriate.
Enhancing healthcare team outcomes
The best outcome with TFCC injury will occur when other causes of wrist pain on the ulnar side are ruled out by prompt initiation of conservative treatment. If the patient does not improve with conservative treatment, the next step is timely surgical consultation. If an MRI is done, it is essential to have the MRI results read by a radiologist experienced in TFCC injuries. An inter-specialist team consisting of a nurse, physiotherapist or occupational therapist, and a doctor will ensure the best follow-up.
Summary
When conservative treatment is started for TFCC injury, the best results come when other ulnar-side wrist pain sources are eliminated. MRI imaging is useful as a preliminary diagnostic tool; Arthroscopy is the gold standard for diagnosis.
Conservative methods like rest, NSAIDs, and corticosteroid injections are among the available treatments, in addition to surgical management. The prognosis for TFCC injuries is generally favorable.
If the patient does not improve with conservative treatment, the next step is timely surgical consultation. If an MRI is done (read by a radiologist experienced in TFCC injuries).
An inter-specialist team consisting of a nurse, physiotherapist or occupational therapist, and a doctor will ensure the best follow-up.
FAQs
What is an injury to the triangular fibrocartilage complex?
When the triangular fibrocartilage complex (TFCC), a cartilage structure that connects the end of the forearm to the tiny wrist bones on the pinkie side, is stressed as a result of an accident or a golf swing, it can rupture or sprain.
Can TFCC tear heal itself?
Yes, a TFCC rupture is treatable without surgery, is the simple response to this issue. It’s critical to recognise that your discomfort may not go away immediately and that the region on the outside of your wrist will recover better without surgery.
What are the symptoms of TFCC injury?
Although you may have discomfort throughout your entire wrist, soreness around the outside of your wrist is the primary sign of a TFCC rupture. You could have discomfort all the time or only when you move or press on your wrist. When you move your wrist, you could hear a clicking or popping sound as one of the signs of a TFCC tear.
How do you repair a TFCC tear?
It is possible to use open or arthroscopic techniques to treat TFCC injuries. A telescope (arthroscope) and other surgical equipment are introduced via 2 to 3 incisions of around 5 mm each created in the wrist during an arthroscopic TFCC repair. This treatment is less invasive.
Can i lift weights with a TFCC injury?
It’s essential to keep an eye on the symptoms and prevent from putting any weight on the wrist for 10 to 12 weeks. It could take more time to fully restore before returning to higher-level activities like heavy lifting, gymnastics, or work as a heavy machine operator. Finally, it’s crucial to have a lot of patience while healing from a TFCC tear.
Is TFCC tear permanent?
With rest and therapy, the majority of mild TFCC tears can mend on their own. More serious tears can be repaired surgically. Within 12 weeks of surgery, the majority of patients with TFCC rips regain full function.
What percentage of TFCC tears require surgery?
The frequency of surgically necessary triangular fibrocartilage injuries. 43% of patients who were initially immobilised for 4 weeks in a short-arm cast or volar orthosis subsequently required surgery. Debridement alone, open repair, or arthroscopic repair are all possible surgical treatment options.





2 Comments