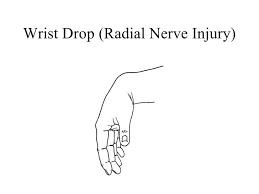
Wrist Drop
What is Wrist Drop?
Wrist drop is a condition caused by radial nerve palsy, resulting in the inability to actively extend the wrist and fingers. When the radial nerve’s function is compromised, the affected individual experiences a flaccid hand that remains flexed when attempting to bring the arm to a horizontal position. This occurs due to the innervation of the extensor muscles by the radial nerve. The flexor muscles of the forearm counteract, leading to a partially flexed wrist.
The hand and wrist are a complex set of joints crucial for various daily activities. Diagnosing and treating hand and wrist conditions require a systematic examination approach. Given the intricacy of these structures, bilateral comparison can aid in accurate diagnosis.
Nerve damage severity can be categorized into three degrees:
- Neurapraxia: The mildest form of injury, categorized as first-degree.
- Axonotmesis: Referring to second, third, or fourth-degree injuries.
- Neurotmesis: The most severe, fifth-degree injury involving complete nerve damage.
Radial nerve injuries are typically confined to the humeral shaft or proximal third of the dorsomedial forearm. High-level radial nerve palsy spares triceps function and elbow extension but results in loss of wrist and thumb extension, thumb abduction, and finger metacarpophalangeal joint extension. Wrist extension is vital for proper flexor tendon tensioning and grip strength. In contrast, distal nerve injuries lead to low radial nerve palsy, preserving wrist extension but causing loss of thumb extension, abduction, and finger metacarpophalangeal joint extension, affecting grip posture.
Observation is common in nerve palsies accompanying closed humeral fractures as normal function usually returns in 3 to 6 months. Surgical exploration for Holstein-Lewis fractures isn’t typically necessary, as recovery tends to occur even without intervention. Open reduction and fixation for acute closed humeral fractures depend on factors other than radial nerve status. Nerve exploration timing varies, and better outcomes are observed with nerve repair performed within six months. Open humeral fractures and lacerations accompanied by nerve deficits may necessitate nerve exploration and repair.
An early tendon transfer may be indicated by Burkhalter in three scenarios:
- To substitute for nerve regrowth, avoid external splints.
- To assist during reinnervation.
- To intervene when nerve repair results are unsatisfactory or irreparable.
Burkhalter proposed the pronator teres transfer to enable early wrist extension and preserve forearm pronation. Low radial nerve palsy, resulting from injuries in the proximal third of the forearm, involves the loss of finger metacarpophalangeal joint extension, thumb extension, and abduction. Procedures for low radial nerve palsy are adapted from those used for high radial nerve palsy.
Forearm anatomy
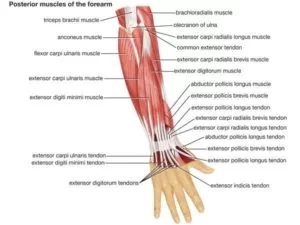
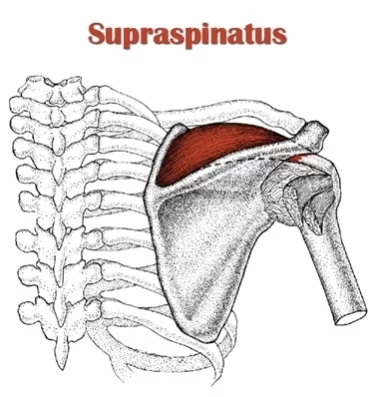
The forearm is the section of the upper limb that extends from the elbow to the wrist, distinct from the arm that stretches from the shoulder to the elbow. The extensor muscles within the forearm encompass the extensor carpi ulnaris, extensor digiti minimi, extensor digitorum, extensor indicis, extensor carpi radialis brevis, and extensor carpi radialis longus. These extensor muscles derive their neural supply from the posterior interosseous nerve, a branch originating from the radial nerve.
Associated with this nerve, several other muscles in the forearm receive innervation, including the supinator, extensor pollicis brevis, extensor pollicis longus, and abductor pollicis longus. These muscles are predominantly situated in the posterior segment of the forearm when it’s in its standard anatomical alignment.
Furthermore, in the arm, specific muscles are innervated by the muscular branches stemming from the radial nerve. These muscles encompass the brachioradialis, anconeus, triceps brachii, and extensor carpi radialis longus. This intricate innervation network orchestrates the various movements and functions of the forearm and arm muscles, ensuring their coordinated activity for daily activities.
Pathophysiology
The radial nerve undergoes a bifurcation into both deep and superficial branches, occurring along the lateral border of the cubital fossa, just distal to the elbow joint. The deep branch, also known as the posterior interosseous nerve, traverses through the supinator muscle, providing innervation to this muscle and the extensor muscles controlling wrist and digital movements. Consequently, injuries occurring proximal to this bifurcation point may not only lead to radial nerve palsy but can also result in sensory disturbances along the radial nerve pathway.
The radial nerve is susceptible to entrapment at the level of the supinator muscle. Entrapment scenarios might include the radial head becoming entrapped proximal to the elbow, often involving the head of the triceps muscle. In such cases, deficits in elbow extension can coincide with the occurrence of wrist drop. Notably, when wrist drop serves as the initial indication of mono neuritis multiplex, its underlying pathophysiology is likely influenced by immunological, infectious, paraneoplastic, or other processes that contribute to axonal damage and subsequent disruption of nerve conduction.
This complex interplay of anatomical branching and potential entrapment underscores the intricacies of radial nerve function and the diverse mechanisms that can contribute to its dysfunction.
Which are the Causes of Wrist Drop?
Wrist extension relies on the coordinated contraction of forearm muscles, causing tension on tendons that attach beyond the wrist. If any components in this chain—the tendons, muscles, or nerves innervating these muscles—suffer damage or dysfunction, it can lead to a condition known as wrist drop.
Several scenarios can lead to the manifestation of wrist drop:
- Stab wounds below the clavicle: Stab wounds at or below the clavicle can damage the radial nerve, a terminal branch of the brachial plexus’s posterior cord. This damage can result in neurological deficits, including limited shoulder abduction beyond 15 degrees, impaired forearm extension, reduced hand supination ability, weakened thumb abduction, and sensory loss along the arm and hand’s posterior surface.
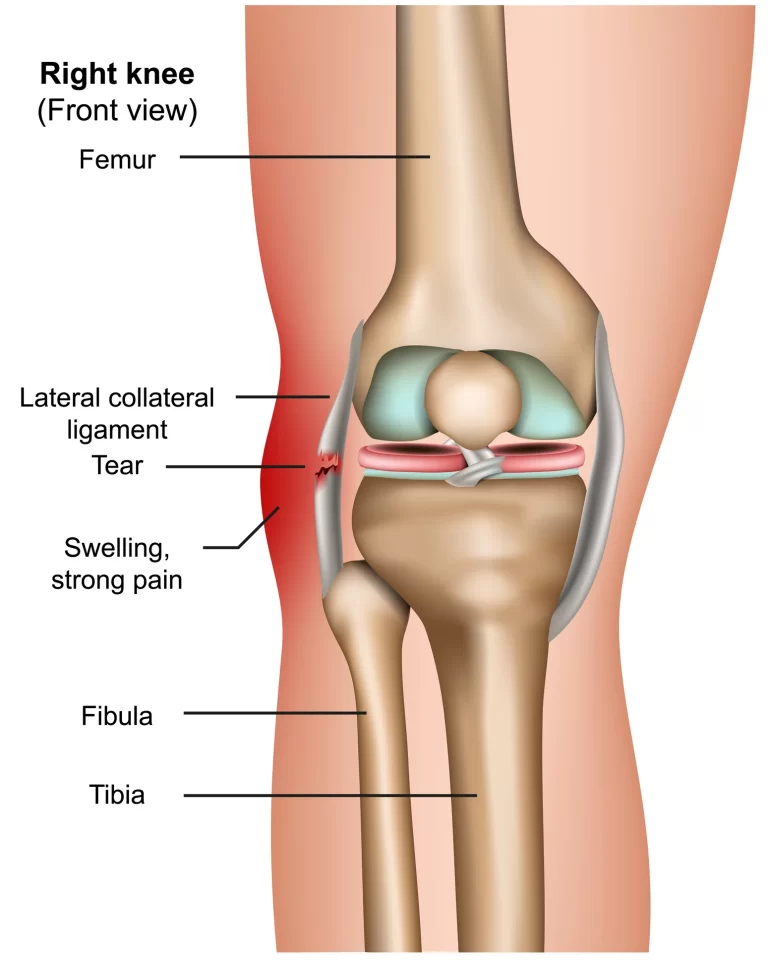
- Humerus fractures: A broken humerus bone can lead to radial nerve damage, especially if the fracture occurs in proximity to the radial groove along the bone’s lateral border, where the radial nerve runs alongside the deep brachial artery.
- Lead poisoning: Wrist drop is associated with lead poisoning due to lead’s adverse impact on the radial nerve.
- Persistent nerve injury: Repetitive movements or prolonged external pressure on the path of the radial nerve, such as extended use of crutches, prolonged leaning on elbows, or regular upper body rope suspension, can cause ongoing nerve injury. The colloquial terms for radial nerve palsy stem from these described causes.
- Correcting dislocated shoulders: Radial nerve palsy can impact from the outdated training of trying to relocate a dislocated shoulder by putting a foot in the armpit & dragging the limb to glide the humerus back into the glenoid cavity of the scapula.
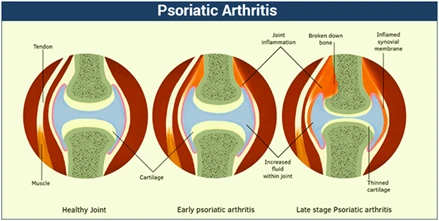
- Neuropathy in rheumatoid arthritis: In rare instances, patients with rheumatoid arthritis may experience wrist drop due to neuropathy. Swollen joints can potentially compress nearby nerves, leading to sensations of pain, numbness, or tingling—known as nerve entrapment. This is often observed at the wrist (carpal tunnel syndrome) or elbow (ulnar nerve entrapment). Neuropathy, a form of nerve damage, can emerge in rheumatoid arthritis patients, often stemming from inflammation of blood vessels (vasculitis).
What are the Symptoms of Wrist Drop?
- The wrist hangs limply, lacking its usual support.
- The ability to raise the wrist is compromised.
- Challenges arise in extending and straightening the wrist as well as the fingers.
- Forming a fist becomes problematic.
- In addition to wrist drop, radial nerve palsy introduces various symptoms that impact the arm, wrist, hand, and fingers, potentially encompassing:
- Sensations of pain surrounding the wrist joint.
- Muscular weakness.
- Numbness spanning from the triceps muscle down to the fingers.
- Difficulty in muscle control.
- Loss of functional capabilities.
- Issues with pinching and grasping objects.
- Diminished strength or an inability to regulate muscles extending from the triceps downward to the fingers.
What is the diagnosis of the Wrist drop?
Evaluation of wrist drop typically encompasses a comprehensive approach, which frequently involves nerve conduction velocity studies as a primary measure to identify and confirm the involvement of the radial nerve. The inability to extend the thumb into a “hitchhiker’s sign” is often utilized as a screening test. Radiographs might reveal bone spurs or fractures contributing to nerve damage, while MRI imaging can be necessary for detecting subtle underlying causes. The assessment of foot drop entails a physical examination to scrutinize weakness, numbness, and related symptoms in the arm and hand.
Sophisticated diagnostic techniques and technologies play a pivotal role in accurately diagnosing, guiding treatment, and closely monitoring wrist drop.
Diagnostic methodologies may include:
- Electromyogram (EMG): This examination gauges the muscle’s electrical activity in response to stimulation, assessing the nature and speed of electrical impulses’ conduction through the nerve. This aids in confirming nerve damage presence and assessing its severity.
- Nerve conduction studies: These tests appraise how effectively specific nerves transmit electrical signals from the spinal cord to muscles. By positioning an electrode emitting electrical pulses over a nerve of interest and recording electrodes over the muscles it supplies, this test determines the time taken for a muscle to contract in response to electrical stimulation.
Imaging Techniques:
- X-rays: These employ minimal radiation to visualize bone lesions or soft tissue masses contributing to symptoms.
- Ultrasound: Using sound waves, this method creates images of internal structures, potentially detecting cysts or tumors on nerves or displaying nerve swelling due to compression.
- CT scan: Employing X-rays from multiple angles, this technique generates cross-sectional views of bodily structures.
- Magnetic resonance imaging (MRI): Employing radio waves and powerful magnetic fields, MRI produces detailed images, especially useful for visualizing soft tissue lesions compressing nerves.
Special Tests:

- Hitchhike Sign: Employed to distinguish between radial nerve or posterior interosseous nerve palsy and dystrophic dwarfism. The assessment involves examining a patient before and after surgery to fix a fracture. A hitchhike sign indicates intact radial and posterior interosseous nerve function. The inability to perform this sign might suggest posterior interosseous nerve involvement.
- Upper Limb Tension Test (ULTT, Radial nerve): This test, conducted initially on the asymptomatic side, assesses pain or tingling sensations during specific joint positioning. Pain provocation during movement or additional maneuvers indicates mechanical interference with neural structures.
Treatment of Wrist drop
The treatment approach for wrist drop depends on its underlying cause. When the cause is effectively addressed, the wrist drop may resolve. However, if the cause cannot be treated, the wrist drop could become a permanent condition.
Medical Interventions for Wrist Drop
In cases where painful paresthesias develop, certain conditions can be managed through methods like sympathetic blocks or laparoscopic synovectomy. Additionally, wrist drop can be addressed with medications like amitriptyline, nortriptyline, duloxetine, pregabalin, and gabapentin, which can alleviate symptoms.
Local Treatments such as transdermal capsaicin or diclofenac may be employed to reduce symptoms. Even when pain is significant, the use of narcotic medications should be minimized. Interestingly, erythropoietin, a hormone primarily approved for treating anemia, has demonstrated potential neuroprotective and neurotrophic properties. It appears to function by promoting cell survival through anti-apoptotic and anti-inflammatory mechanisms.
Splinting as a Management Strategy for Wrist Drop

One effective method involves the utilization of a radial nerve palsy splint designed to address wrist and finger extension issues. This type of splint is scarce in the market, particularly ones that offer affordability, functionality, practicality, comfort, and proper fit. Notably, wrist issues caused by radial nerve injuries, leading to wrist drop, are more prevalent than commonly perceived. As a reference, statistics indicate that around 2% to 17% of individuals with a humeral shaft fracture eventually experience radial nerve palsy.
With this in mind, our team of therapists is dedicated to creating an innovative and supportive radial nerve brace that caters to both men and women with radial nerve palsy, peripheral nerve injury, wrist drop, and related conditions. Our “BraceAbility Radial Nerve Palsy Splint” has been engineered to position the wrist and fingers into dorsiflexion, enabling movement while providing crucial support following radial nerve injuries. As recovery progresses, the splint aids in strengthening the wrist extensors, thereby accelerating the healing process.
Physical therapy treatment for Wrist drop
It serves as a pivotal component for fortifying the arm’s musculature, effectively mitigating the vulnerability to radial nerve injuries. The adept therapist imparts invaluable knowledge encompassing proper balance exercises, a preventive measure against potential falls.
The significance of maintaining an ergonomic posture both in the workplace and during sleep is also instilled in the patient. Leveraging the expertise of a physiotherapist, patients are empowered to manage medical conditions such as diabetes and kidney stones, thus effectively diminishing the likelihood of radial nerve injury.
Electrotherapy:
2. Application of Hot Packs: This modality stands as a potent ally in the pursuit of pain relief, offering a therapeutic dimension to the treatment approach.
1. Electrical Stimulation (TENS): This innovative approach capitalizes on a mild electrical current to alleviate the discomfort associated with radial nerve pain. The compact TENS device, harnessing battery power, interfaces with adhesive electrodes strategically positioned to stimulate nerve activity in regions prone to wrist drop.
3. Electrical Stimulation (ES): The application of mild electrical pulses through the skin effectively stimulates targeted muscles or nerves, translating to reduced pain. Although not universally applicable, ES showcases promise in accelerating recovery and mitigating distressing symptoms among those who can undergo painless procedures.
Integral to physical therapy, massage therapy assumes a pivotal role in counteracting swelling that could potentially impede radial nerve function. This beneficial effect can be attributed to the lymphatic fluid-draining properties inherent to massage techniques. Of paramount significance, physical therapy is a driving force behind the rehabilitation of an injured radial nerve, bolstering blood circulation and consequentially restoring mobility to the wrist and fingers. This restorative journey is further supported by purposeful gripping exercises, offering potential relief for conditions such as wrist drops.
The practice of electrotherapy, coupled with an array of strategic physical therapy interventions, converges into a comprehensive healing strategy, fostering pain management and functional recovery.”
Exercise for Wrist Drop:
Stretching Exercises:

- Praying Position Stretching: Initiate the exercise in either a standing or sitting position. Palms are joined in a praying stance with elbows touching, positioned in front of the face. Gradually spread the elbows apart, lowering the hands to waist height. Hold the stretch for 30 seconds, repeating three times in one session. Perform three sessions daily.
- Wrist Flexors Stretch: Straighten the arm and bend the wrist back, applying gentle pressure across the palm with the opposite hand. Hold the stretch for 30 seconds, repeating three times per session. Engage in three sessions daily.
- Clenched Fists: Start seated, palms open on thighs. Close hands into fists, raising them off the thighs and bending at the wrists. Hold for 30 seconds, repeating three times in one session. Perform three sessions daily.
- Hooked Stretching Exercise: Interlock elbows and pull arms toward the centre of the torso, feeling the stretch in the shoulders. Wrap one arm around the other, palms touching. Hold for 30 seconds, repeat three times per session, and engage in three daily sessions.
- Finger Stretching Exercise: Touch the pinky and ring fingers together, separating the middle and index fingers. Hold for 30 seconds per repetition, perform three repetitions in one session, and repeat three sessions daily.
- Fist-Opener: Make a fist and hold it for 30 seconds. Open your fingers wide, repeating the motion five times in one session. Engage in three sessions daily.
- Thumb Pull: Grip and gently pull the thumb backward. Hold for 30 seconds per repetition, perform three repetitions in one session, and repeat three sessions daily for each thumb.
- Alternate Finger Stretch: Bring middle and ring fingers together, separating pinky and index fingers. Perform three repetitions per session and engage in three daily sessions.
- Side to Side Stretching: Adopt the tabletop position, moving fingers outward, then side to side. Hold for 30 seconds, repeat three times per session, and perform three sessions daily.
- Wrist Circle Stretching Exercise: Sit with hands hanging off a table edge, and make wrist circles clockwise and counterclockwise. Hold each position for 30 seconds, repeat three times per session, and engage in three daily sessions.
- Thumb and Upper Wrist Stretching Exercise: Extend the arm and make a fist around the thumb. Bend the fist downward to stretch the wrist’s top and the thumb. Hold for 30 seconds, repeating three times per session for each hand, and engage in three daily sessions.
- Palm to Ceiling Wrist Stretching Exercise: Extend arm with palm facing the ceiling, bend wrist to point fingertips downward. Gently pull fingers toward the body with the opposite hand, feeling the stretch. Hold for 30 seconds, repeat three times per session for each hand, and perform three daily sessions.

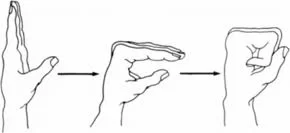
- Finger Tendon Glide Stretch: Perform a hook fist, then a straight hand, ten times per set. Engage in three sets per session and repeat three daily sessions.
- Loosen-Up Stretching Exercise: A simple exercise to prepare the fingers and hands for subsequent exercises. While seated, extend the arm at a right angle and make a fist, then gradually open the fingers. Hold for 30 seconds, repeat three times per session, and engage in three daily sessions.
- Wrist Supinators Stretching: Sit or lie down comfortably, the therapist grasps the hand and turns the palm upward. Hold for 30 seconds, repeat three times per session, and perform three daily sessions.
- Wrist Pronators Stretching: Assume a comfortable position, therapist grasps the hand and turns the palm downward. Hold for 30 seconds, repeat three times per session, and engage in three daily sessions.
- Table Stretch: Stand beside a table, place the back of the hand on the table, and rotate the body away. Perform three times per session and engage in three daily sessions.
Range of Motion Exercise for Wrist Drop:
Passive Range of Motion Exercise:
Passive Wrist Extension: Initiate the exercise from a seated position, allowing the affected hand to hang off the table’s edge with full pronation. Place a rolled towel underneath. Position the physical therapist opposite the patient. The therapist instructs the patient to attempt a wrist upward movement. When the patient’s reach is limited, the therapist aids in achieving a complete range. Repeat ten times per session. Engage in three sessions daily.
Passive Wrist Ulnar Deviation: Sit comfortably with the affected hand in mid-pronation. Employ the rolled towel for support. The therapist stands opposite the patient. The patient attempts wrist-down movement while the therapist assists in attaining the full range of ulnar deviation. Perform ten times per session. Engage in three sessions daily.
Passive Wrist Radial Deviation: Adopt a seated position with the affected hand in mid-supination. Place the rolled towel underneath. The therapist faces the patient. Instruct the patient to try moving the wrist upward, while the therapist aids the radial deviation to achieve the complete stretch. Perform ten times in one session. Engage in three sessions daily.
Passive Supination: Sit comfortably, with the injured hand in full pronation and the rolled towel in place. The therapist faces the patient. Instruct the patient to attempt wrist rotation while the therapist passively facilitates supination until the stretch is felt. Perform ten times in one session. Engage in three sessions daily.

Passive Pronation: Seated on a chair, the affected hand rests in full supination with the rolled towel underneath. The therapist stands opposite. The patient tries wrist rotation while the therapist assists in pronation until the stretch is felt. Repeat ten times per session. Perform three sessions daily.
Passive Finger Flexion and Extension: Place the affected hand flat on the table, palm up, fingers extended. The therapist places their free hand on the back of the fingers and guides them inward for flexion and outward for extension. Perform ten times per session. Engage in three sessions daily for each movement.
Passive Thumb Flexion and Extension: Position the forearm on a table with the affected hand in mid-pronation, employing the rolled towel. The therapist gently bends the thumb down for flexion and stretches it outward for extension. Perform ten times per session. Engage in three sessions daily.
Active-Assisted Range of Motion Exercise:

Active-Assisted Wrist Extension: Seated, allow the affected hand to relax on the table’s edge in full pronation. Use the rolled towel for support. The therapist stands opposite. The patient tries wrist upward movement, with the therapist providing assistance as needed. Perform ten times per session. Engage in three sessions daily.
Active-Assisted Wrist Ulnar Deviation: Sit on a chair, ensuring the affected hand is in mid-supination and supported by the rolled towel. The therapist stands opposite. As the patient attempts wrist-down movement, the therapist provides aid to achieve the full ulnar deviation range. Perform ten times per session. Engage in three sessions daily.
Active-Assisted Wrist Radial Deviation: From a seated position, with the affected hand in mid-supination, use the rolled towel for support. The therapist stands opposite. As the patient aims for wrist-up movement, the therapist assists in radial deviation to attain the full stretch. Perform ten times in one session. Engage in three sessions daily.
Active-Assisted Supination: Sit on a chair, ensuring the injured hand is in full pronation, supported by the rolled towel. The therapist faces the patient. Instruct the patient to rotate the wrist while the therapist provides outside force to achieve the full supination range. Perform ten times per session. Engage in three sessions daily.
Active-Assisted Pronation: In a seated position, keep the affected hand in full supination and support it with the rolled towel. The therapist stands opposite. The patient is guided to rotate the wrist, with the therapist offering assistance to reach the full range of pronation. Perform ten times per session. Engage in three sessions daily.
Active-Assisted Thumb Flexion and Extension: Sit on a chair, ensuring the hand is in mid-pronation, using the rolled towel for support. The therapist gives a command to bend the thumb down for flexion, assisting as needed. Perform ten times per session. Engage in three sessions daily.
Active Range of Motion Exercise:
Wrist Supination: Stand or sit with the arm at the side, the elbow bent to 90 degrees, and the hand mid-range over a table’s edge. Turn the forearm’s palm facing upward without reaching the endpoint. Perform ten times per set per session. Engage in three sessions daily.
Wrist Pronation: Stand or sit, the arm at the side, elbow flexed to 90 degrees, hand mid-pronation over a table’s edge or knee. Rotate the wrist downward, with the palm facing the ground, without reaching the endpoint. Perform ten times per session. Engage in three sessions daily.
Wrist Extension Range of Motion Exercise: With the forearm resting on a table and the hand hanging off, palm down, move the hand upward until a gentle stretch is felt. Return to the starting position. Perform ten times in one session. Engage in three sessions daily.
Wrist Extension in Supination Position: With the forearm supported by a table and the hand in full supination, use the rolled towel. Stretch the hand backward slightly without abduction motion. Perform ten repetitions per session. Engage in three sessions daily.
Wrist Ulnar Deviation: Support the forearm on a table or knee, with the thumb upward. Move the wrist down through the full ulnar deviation range. Perform ten times per session. Engage in three sessions daily.
Wrist Radial Deviation: Support the forearm on a table or knee, with the thumb upward. Move the wrist upward through the full radial deviation range. Perform ten times in one session. Engage in three sessions daily.
Thumb Flexion and Extension: Support the forearm on a table or knee. Position the thumb outward and move it across the palm and back to the starting position. Perform ten times in one session. Engage in three sessions daily.
Additional Range of Motion Exercises:
Wrist Supination: Extend the arms parallel to the floor, bend the elbow, and face the palm upward. Hold the wrist to gently turn the forearm into the palm-up position until a stretch is felt. Hold for 30 seconds. Repeat three times in one session. Engage in three sessions daily.
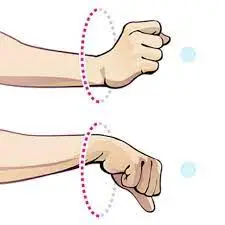
Wrist Circles: Sit comfortably and bring the hands up with the elbows close to the body, making fists. Rotate the wrists in a circular motion while keeping the palms facing down to maximize the range of motion. Perform ten circles in each direction per session. Perform three sessions daily.
Wrist Shakes: Hold the hands in a “namaste” position and shake the wrists for one minute per set per session. Engage in three sessions daily.
Shake It Out: Hold the hands out in front with palms facing down. Gently shake the hands by letting the wrists go limp. Continue for 30 seconds. Do repeat up to 3 times/set. One set per session is sufficient. Engage in three sessions daily.
Fist to Fan: Position the hands in front with palms facing downwards. Make a fist and then open it halfway, bending the fingers at the knuckles. Open the hands fully with all five fingers straight and spread apart. Hold for ten seconds per repetition. Perform five times per session. Engage in three sessions daily. After opening the hand fully, return to a fist and repeat the sequence.
Thumb Touches: Extend the arms outward with palms facing the ceiling. Use the injured hand to touch the tip of each finger. Gradually touch further down on each finger until the base of each finger is touched. Repeat ten times per session. Engage in three sessions daily.
Wrist Supination: Stand or sit with an arm at the side, the elbow bent to 90 degrees, and the forearm over the table’s edge. Move the hand upward, facing the roof, without reaching the endpoint. Perform ten times per set per session. Engage in three sessions daily.
Wrist Pronation: Stand or sit with an arm at the side, elbow flexed to 90 degrees, and the forearm over the table’s edge or knee. Move the hand downward, facing the ground, without reaching the endpoint. Perform ten times per session. Engage in three sessions daily.
Wrist Extension Range of Motion Exercise: Support the forearm on a table with the hand hanging off, palm down. Push the hand upward until a mild stretch is sensed. Return to the starting position. Perform ten times in one session. Engage in three sessions daily.
Wrist Extension in Supination Position: Support the forearm on a table with the hand in full supination. Stretch the hand backward slightly without abduction motion. Perform ten repetitions per session. Engage in three sessions daily.
Wrist Ulnar Deviation: Support the forearm on a table or knee, with the thumb upward. Move the wrist downward through the full ulnar deviation range. Perform ten times per session. Engage in three sessions daily.
Wrist Radial Deviation: Support the forearm on a table or knee, with the thumb upward. Move the wrist upward through the full radial deviation range. Perform ten times in one session. Engage in three sessions daily.
Thumb Flexion and Extension: Support the forearm on a table or knee. Position the thumb outward and move it across the palm and back to the starting position. Perform ten times in one session. Engage in three sessions daily.
Strengthening Exercises for Wrist Drop Recovery:
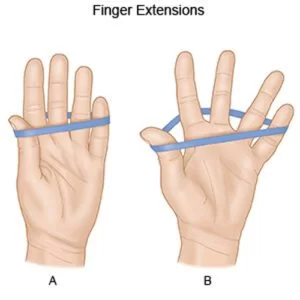
Rubber Band Stretch: Begin by having the patient sit comfortably. Place a rubber band around all five fingers of the affected hand. Encourage the patient to stretch their fingers out as wide as possible against the resistance of the rubber band, then relax. Perform three sets of ten repetitions for both hands. Gradually increase resistance by adding more rubber bands as strength improves.
Hammer Rotation: Choose a lightweight implement such as a hammer or wrench. The patient should sit forward in a chair and rest the chosen implement on their thigh, palm facing inward. Slowly rotate the wrist downwards to face the ground, then return to the starting position and rotate the wrist upwards to face the ceiling. Perform ten repetitions per session for three sessions daily.
Grip Strengthening: Using grippers of varying tensions, have the patient sit comfortably with their arm bent at 90 degrees and palms facing inward. Instruct the patient to squeeze the gripper for a slow count of three, then release without reaching the endpoint. Repeat this ten times per session for three sessions daily. Progress to higher tensions as strength improves.
Fist to Jazz Hand: Have the patient rest their affected arm on a table as if preparing for an arm wrestle. Make a fist, then slowly open the hand wide into a “jazz hand” position. Repeat this ten times per session for three sessions daily.
Finger Spread-Apart with Theraband: Wrap a theraband around the fingers and push against the resistance to spread the fingers as wide as possible. Hold for about ten seconds, then release. Perform ten repetitions per session for three sessions daily, alternating hands.
Dumbbell Windshield Wipers: Position the forearm on a stable surface and hold a lightweight dumbbell in the hand. Rotate the wrist in a windshield wiper motion from right to left. Perform ten repetitions per session for three sessions daily.
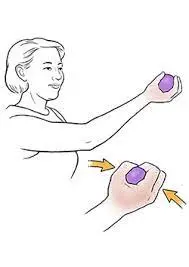
Ball Squeeze: In a standing or sitting position, have the patient hold a stress ball, tennis ball, or similar object in the affected hand. Squeeze the ball as hard as possible for ten seconds, then release it. Perform ten repetitions per session for three sessions daily. Gradually increase repetitions as strength improves.
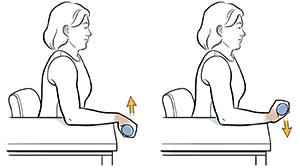
Wrist Extensors Strengthening with Dumbbell in Pronation: Sit comfortably with the forearm resting on a table and the hand hanging off the edge, palm down. Hold a 2-3 pound dumbbell in the affected hand. Slowly lift the hand, palm down, toward the ceiling, then return to the starting position. Perform ten repetitions per session for three sessions daily. After 5-6 days, add a ten-second hold at the endpoint.
Wrist Extensors Strengthening with Dumbbell in Supination: Sit with the forearm resting on a table and the hand hanging off the edge, palm up. Hold a 2-3 pound dumbbell in the affected hand. Slowly move the hand downward, palm up, toward the floor, then return to the starting position. Perform ten repetitions per session for three sessions daily. After 5 days, add a ten-second hold at the endpoint.
Wrist Supination with Dumbbell: Sit with the forearm resting on a table, wrist and hand over the edge. Hold a small dumbbell in the affected hand with the palm facing inwards. Slowly rotate the hand so the palm faces upward, then return to the starting position. Perform ten repetitions per session for three sessions daily. After 5-6 days, add a ten-second hold at the endpoint.
Wrist Pronation with Dumbbell: Sit with the forearm resting on a table, wrist and hand over the edge. Hold a small dumbbell in the affected hand with the palm facing upward. Slowly rotate the hand so the palm faces downward, then return to the starting position. Perform ten repetitions per session for three sessions daily.
Rotation Exercise: Sit with arms bent at 90 degrees and forearms in front, palms facing down. Hold a resistance band or lightweight dumbbell in your hands. Slowly rotate the hands to face upward, then rotate back to the starting position. Perform ten repetitions per session for three sessions daily.
Wrist Curl: Sit with the arm bent at 90 degrees and the palm facing up. Rest the forearm on a stable surface. Curl the wrist upward and then return to the starting position. Perform ten repetitions per session.
Pronated Wrist Curl: Sit with the arm bent at 90 degrees and palm facing down. Rest the forearm on a stable surface. Curl the wrist upward and then return to the starting position. Perform ten repetitions per session.
Squeeze Exercise: Stand or sit and hold a squeezable object in the affected hand, with the palm facing up. Squeeze the object as hard as possible for ten seconds, then release. Perform ten repetitions per session for three sessions daily. Gradually increase repetitions.
Wrist Ulnar Deviators Strengthening with Theraband: Sit on a chair with the hand in mid-pronation position over the edge of a table, supported by a rolled towel. Wrap a theraband around the hand and provide resistance as the patient moves the hand downward. Perform ten repetitions per session for three sessions daily. After 5 days, add a ten-second hold at the endpoint.

Wrist Radial Deviators Strengthening with Theraband: Sit on a chair with the hand in mid-supination position over the edge of a table, supported by a rolled towel. Wrap a theraband around the hand and provide resistance as the patient moves the hand upward. Perform ten repetitions per session for three sessions daily. After 5-6 days, add a ten-second hold at the endpoint.
Wrist Extensors Strengthening with Theraband in Pronation: Sit on a chair with the hand hanging off the edge of a table, palm facing down. Wrap a theraband around the hand and provide resistance as the patient lifts the hand upward. Perform ten repetitions per session for three sessions daily. After 5 days, add a ten-second hold at the endpoint. Gradually increase resistance as strength improves.
Wrist Extensors Strengthening with Theraband in Supination: Sit on a chair with the hand hanging off the edge of a table, palm facing up. Wrap a theraband around the hand and provide resistance as the patient moves the hand downward. Perform ten repetitions per session for three sessions daily. After 5 days, add a ten-second hold at the endpoint. Gradually increase resistance as strength improves.
Supinators Strengthening with Theraband: Sit on a chair with the hand in a neutral position over the edge of a table. Wrap a theraband around the hand and provide resistance as the patient rotates the hand to face upward. Perform ten repetitions per session for two sessions daily. After 5-6 days, add a five-second hold at the endpoint. Gradually increase resistance as strength improves.
Pronators Strengthening with Theraband: Sit on a chair with the hand in full pronation over the edge of a table. Wrap a theraband around the hand and provide resistance as the patient rotates the hand to face downward. Perform ten repetitions per session for three sessions daily. After 5 days, add a ten-second hold at the endpoint. Gradually increase resistance as strength improves.
Massage Techniques for Wrist Drop Recovery:
Massage therapy is a time-honored practice that combines stretching and rhythmic pressure to alleviate tension and promote healing. Through massage, specific muscles affected by injury or stress can be relieved of tension. The therapy enhances blood circulation, expediting the recovery process at all levels.
Benefits of Massage Therapy:
- Reduces stress and induces relaxation.
- Alleviates pain, muscle soreness, and tension.
- Enhances circulation, energy levels, and alertness.
- Decreases heart rate and blood pressure.
- Boosts the body’s immune function.
Effleurage (Stroking) Technique: Effleurage involves the rhythmic and continuous movement of hands over the patient’s affected area, typically in one direction. Its purpose is to enhance blood flow, stretch tissues, induce relaxation, and aid in the removal of waste products. This technique is often the introductory and concluding step in a massage session. The pressure and speed of effleurage can be adjusted based on the specific situation and desired outcomes of the massage.
Petrissage (Kneading) Technique: Petrissage entails lifting, pressing, squeezing, pinching, and rolling of the skin and underlying tissues. This alternating action stimulates localized circulation, potentially providing relief from muscular disorders. The core movement is to compress, lift, and then release the soft tissues. It is usually chosen when a deeper effect than effleurage is desired. Petrissage techniques encompass:
- Squeezing: The therapist instructs the patient to find a comfortable position, either supine or seated. A circular hand motion is applied over the entire wrist area, involving circular movement. The therapist lifts and pulls tissues gently between their hands, creating space away from the body.
- Picking Up: Starting with patient comfort, the therapist uses equal pressure on the sides of the tissue, lifting it away from the body. The therapist’s hands remain parallel to the treated limb to prevent excessive extension of the wrist.
- Shaking: Vibration or shaking involves gentle, tremulous movements performed using hands or fingers. This technique can stimulate soft tissues, alleviate muscular tension, and reduce stress. The therapist positions one hand atop the other and applies vibrating motions by stroking over the affected area.
- Rolling: Utilizing the thumb and fingers, the therapist pulls the skin away from the tissue and proceeds to roll it forward in a continuous motion. This technique aids in separating the skin from muscle tissue, especially beneficial around scarred areas.
- Wringing: The wringing technique involves lifting and squeezing muscles in a back-and-forth motion. It targets tight muscles, promotes relaxation, and can be incorporated into post-event massages. Wringing can relieve muscle tightness, reduce delayed onset muscle soreness (DOMS), and expedite recovery.
FAQ
What are the symptoms of the wrist drop nerve?
Numbness from the triceps downwards to the fingers.
Difficulties in opening the fingers.
Lifting & grasping difficulties.
Weakness/inability to maintain muscles from the triceps downwards to the fingers.
Wrist drop when the wrist swings limply & the patient can’t raise it.
Which muscles are weak in wrist drop?
Wrist drop & finger drop are characteristic of damage to the radial nerve within the spiral groove in the upper limb. The brachioradialis muscle may be weak & its tendon reflex failed.
What is the difference between C7 and radial nerve palsy?
C7 radiculopathies can generate sensory differences in the ring finger. Radial neuropathies can induce sensory modifications in the dorsum aspect of the hand between the web of the thumb & 1st finger. Irritative manoeuvres contain Spurling’s manoeuvre & Tinel’s sign.
What is the most common cause of wrist drop?
Wrist drop is an illness induced by radial nerve palsy. Because of the radial nerve’s innervation of the extensor muscles of the wrist & fingers, those whose radial nerve role has been compromised can’t vigorously spread them.
Which nerve is damaged in wrist drop?
Wrist drop is induced by injury to the radial nerve, which spans down the arm & contains the motion of the triceps muscle at the back of the upper limb, because of several circumstances.
What is honeymoon palsy?
Saturday night palsy classically affects a person falling asleep with the arm suspending over a chair/another rigid surface, causing to compression within the axilla. Honeymoon palsy, on the other hand, guides to a person falling asleep on the arm of another & thus compressing that individual’s nerve.



2 Comments