Type 2 Diabetes Treatment
Type 2 diabetes is a chronic metabolic condition characterized by insulin resistance and impaired insulin secretion, leading to elevated blood sugar levels. It is a prevalent and potentially serious health concern worldwide.
The primary goals of treating type 2 diabetes are to manage blood glucose levels, prevent complications, and improve overall well-being. Treatment approaches typically include lifestyle modifications, such as diet and exercise, along with medications that enhance insulin sensitivity, stimulate insulin production, or manage blood sugar levels.
Individualized care plans, regular monitoring, and patient education are crucial components of effective type 2 diabetes management.
What Is Type 2 Diabetes?
Type 2 diabetes is a chronic disorder in which increased blood glucose levels result from insulin resistance and insufficient insulin production. It is a prevalent condition globally, primarily associated with lifestyle factors such as obesity, physical inactivity, and genetic predisposition
Diabetes mellitus or adult-onset diabetes was the other name. However, kids and teenagers can also be affected by type 2 diabetes, primarily due to childhood obesity.
Type 2 diabetes is the most common kind. Approximately 10% of people are type 2 diabetics. A third of people have prediabetes, which is characterized by increased blood sugar or blood glucose levels but not yet diabetes.
Diabetes Type 2 Symptoms
Type 2 diabetes can have symptoms that are so insignificant that you are unaware of them. Among the symptoms are:
- Being extremely thirsty
- Frequently urinating
- Blurry vision
- Feelings of numbness or tingling in your feet or hands
- Fatigue or a sense of exhaustion
- Injuries that do not mend
- yeast infections that return repeatedly
- Craving food.
- Loss of weight without effort
- Contracting infections
- See a doctor if someone develops black rashes under their arms or around their neck.
- These are known as acanthosis nigricans, and they could indicate an increasing level of insulin resistance in the body.
Diabetes Types
Diabetes comes in three primary forms:
Diabetes type 2
- Approximately 90–95% of all diabetics have this kind of diabetes.
- Type 2 diabetes is characterized by low pancreatic synthesis of insulin, the hormone that aids in the conversion of glucose, a form of sugar, from food into energy in your cells.
- Insulin resistance is a problem where your cells don’t react to this hormone as they should in certain people.
Diabetes type 1
- In type 1 diabetes, high blood sugar because your immune system kills the insulin-producing cells in your pancreas.
- The cause of this is unknown.
- Type 1 is unrelated to weight or way of living.
- It was once known as pediatric diabetes or insulin-dependent diabetes.
Gestational diabetes
- This particular kind of diabetes only develops during pregnancy.
- Insulin resistance can result from pregnancy-related weight gain and hormonal changes, which is why it occurs.
- After having a kid, it normally fades away.
Type 2 Diabetes Causes
Typically, type 2 diabetes is brought on by several factors. They could consist of:
Genes: Researchers have identified several DNA segments that influence the production of insulin in the body.
Weight: Obesity or excess weight might contribute to insulin resistance.
Metabolic syndrome: Individuals who are insulin resistant frequently suffer from high blood pressure, high blood sugar, high triglycerides, and high cholesterol.
Too much glucose is produced and released by your liver when your blood sugar is low.
When you eat, your blood sugar rises, and your liver typically slows down and stores glucose for later use. However, some people’s livers do not. They continue to produce sugar.
In bad cell communication, cells send inaccurate signals or do not correctly take up communications. Diabetes can develop when these issues impair how your cells produce and use insulin or glucose.
Broken beta cells- When the cells that produce insulin send it out at the incorrect moment, your blood sugar levels fall. High blood sugar levels can potentially be detrimental to these cells.
Risk Factors for Type 2 Diabetes
Few factors make a person more likely to develop type 2 diabetes. Your odds of receiving it are higher if more of these apply to you.
Some things have to do with who you are:
- 45 years of age or older
- Diabetes is in a parent or Relatives
- African Americans, Alaska Natives, Native Americans, Asian Americans, Hispanic or Latino Americans, and Pacific Islander Americans
The following are risk factors related to your medical history and health:
- Insulin sensitivity
- Prediabetes
- Heart and vascular disease
- High blood pressure, even if managed and controlled
- Low levels of HDL (“good”) cholesterol
- Triglyceride levels are high.
- Obesity and being overweight
- Having a child weighing greater than 9 pounds
- You had gestational diabetes while pregnant.
- PCOS (polycystic ovary syndrome)
- Depression
Other factors that increase your risk of diabetes include your everyday behaviors and lifestyle.
These are the ones you can influence:
- Little or no physical activity
- Smoking
- Anxiety
- Too little or too much sleep
Diagnosis and Testing for Type 2 Diabetes
Your blood can be tested for indicators of type 2 diabetes by your doctor. They will usually check you on two different days before the diagnosis. However, if your blood glucose level is extremely high or you have several symptoms, one test may suffice.
Blood tests for type 2 diabetes include:
- A1c is the average percentage of your blood glucose over the previous two or three months.
- A fasting plasma glucose test is sometimes referred to as a fasting blood sugar test.
- On an empty stomach, it measures your blood sugar.
- You will be unable to eat or drink anything other than water for 8 hours before to the test.
- Oral glucose tolerance test (OGTT)-This tests your blood glucose levels before and after drinking something sweet to observe how your body reacts to the sugar.
Type 2 Diabetes Stages
Type 2 diabetes has four stages, according to researchers:
Insulin sensitivity
- At this point, your body normally produces enough insulin to keep blood sugar levels within normal limits.
- However, if your cells “resist” insulin (do not use it appropriately), your body will produce more insulin to assist the glucose entering them. Insulin resistance can be temporary or permanent.
- Because there is no test to detect insulin resistance, it might be difficult to diagnose.
Prediabetes
- Insulin resistance eventually leads to glucose buildup in the blood.
- When your blood sugar levels are higher than normal but not high enough to be called diabetes, you have prediabetes.
- Prediabetes is defined as an A1c between 5.7% and 6.4%.
- You may not be experiencing any symptoms.
- Although, prediabetes increases your risk of type 2 diabetes, heart disease, or strokes.
Type 2 diabetes
- You have diabetes if your A1c is 6.5% or above.
- You may experience increased thirst, impaired vision, and numbness in your feet or hands.
- You may possibly experience no symptoms at all.
Diabetes type 2 with vascular problems
- At this point, your diabetes has caused vascular (blood vessel) issues.
- Damage to the vessels in your eyes (retinopathy), kidneys (nephropathy), and some nerves (neuropathy) is possible.
- You could potentially get heart disease, a stroke, or circulatory problems.
Type 2 Diabetes Treatment
Unlike many other medical disorders, you manage T2D primarily on your own, with medical direction and help from your healthcare team. This may include you:
- Endocrinologist or primary care physician (PCP).
- Dietitian who is registered.
- Diabetes education and care specialist (CDCES).
- Ophthalmologist (eye specialist).
- Dentist.
- Family members and other essential persons in your life should be included on your team.
- T2D management might be difficult because you must make multiple judgments every day.
- However, every effort you make to improve your health is worthwhile.
Using insulin
All persons with type 1 diabetes and some people with type 2 diabetes use insulin to keep their blood sugar levels from becoming too high.
There are several forms of insulin, and the majority of them are classified according to how long their impact lasts. Insulins are classified as rapid-acting, short-acting, intermediate-acting, long-acting, or mixed.
Some patients will require long-acting insulin to keep their blood sugar levels consistently low. Short-acting insulin or a combination of insulin types may be used by others. Regardless of the type, a person will normally monitor their blood sugar levels to see how much insulin they require.
A blood glucose monitor, which includes pricking the skin, or a combination of a continuous blood glucose monitor (CGM) and skin pricks can be used to examine blood sugar levels.
Throughout the day, a CGM takes blood sugar levels. They can assist a client in making drug changes.
A person’s blood sugar levels can only be determined through self-monitoring. Assuming the level based on any physical symptoms that occur may be harmful unless a person suspects severely low sugar and believes they require an immediate dosage of glucose.
Diabetes Type 2 Diet
Request a meal plan recommendation from your healthcare professional or certified dietitian. What you eat, how much you eat, and when you eat are all essential factors in keeping your blood sugar levels within the range recommended by your healthcare provider.
The key to eating with Type 2 diabetes is to consume a range of healthful foods from all food categories in the amounts specified in your meal plan.
In most of the cases, the following foods can help manage blood sugar levels:
- Chicken, eggs, fish, and turkey are all examples of lean proteins.
- Broccoli, green beans, salad greens, and cucumbers are examples of non-starchy vegetables.
- Avocados, almonds, natural peanut butter, and olive oil are examples of healthy fats.
- Beans, cherries, sweet potatoes, and whole-wheat bread are examples of complex carbs.
Monitoring of blood sugar levels
Monitoring your blood sugar levels is critical for determining how well your current treatment strategy is working. It teaches you how to control diabetes on a daily — and sometimes hourly — basis. Blood sugar monitoring information can help you make decisions about food, physical exercise, and insulin dosing.
Several factors can influence your blood sugar levels. Some of these impacts can be predicted with time and practice, while others are extremely difficult or impossible to predict. That is why, if your healthcare practitioner suggests it, you should check your blood sugar on a frequent basis.
If you have diabetes, there are two major techniques to monitor your blood sugar at home:
- With the help of a glucose meter and a finger stick.
- With the help of a continuous glucose meter (CGM).
You can use one or both ways for a number of reasons, including:
- Because of the cost and medical insurance coverage, your access to technology may be different.
- How frequently should you check your blood sugar, according to your doctor?
- You’re taking drugs.
- Your general well-being.
Other diabetes treatments for type 2
To control Type 2 diabetes, your healthcare professional may advise you to take medication in addition to making lifestyle modifications. These are some examples:
Oral diabetic drugs: These are oral drugs that help people with type 2 diabetes who are still producing some insulin to keep their blood sugar levels stable. There are various kinds. Metformin is the most usually prescribed. To obtain the best blood glucose control, your provider may prescribe more than one oral diabetes medication at a time.
GLP-1 and dual GLP-1/GIP agonists: These are injectable drugs that primarily help persons with T2D maintain their blood sugar levels. Some GLP-1 agonists can also help in the treatment of obesity.
Insulin: Synthetic insulin decreases blood sugar levels immediately. Insulin comes in a variety of forms, including long-acting and short-acting insulin. You can inject it using syringes or pens, inhale it, or use an insulin pump.
Other drugs: You may be prescribed additional medications to treat coexisting problems such as high blood pressure and high cholesterol.
What is the most efficient method of treating type 2 diabetes?
Insulin is the quickest technique to treat high blood sugar levels. If a person has dangerously high blood sugar levels and is in DKA or HHS, they must go to the hospital where insulin, replacement fluids, and nutrients will be administered via an intravenous drip.
If you observe symptoms of low blood sugar levels (also known as a hypo), the quickest method to address it is to eat or drink 15 to 20g of fast-acting carbohydrates right away. Learn what to do if someone has a severe hypo.
We know that persons with type 2 diabetes who are overweight or obese can efficiently and rapidly regulate their blood sugar levels by decreasing weight and adopting a very low-calorie diet. They should do so with the assistance of their healthcare team. They may be able to put their diabetes into a cure in some situations. On the NHS, you may learn about low-calorie diets for persons with type 2 diabetes to help them lose weight quickly.
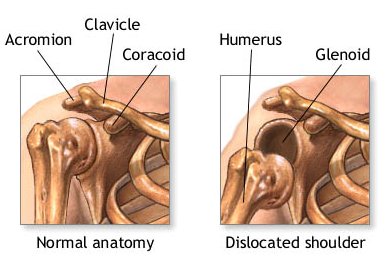
How insulin problems develop
The precise causes of type 1 diabetes is unknown. However, it is easier to identify the reasons of insulin resistance, which can result in type 2 diabetes.
Insulin causes glucose from a person’s diet to enter the cells of their body and provide energy.
- A person’s genes or environment make it more probable that they will be unable to create enough insulin to cover the amount of glucose, or sugar, they consume.
- The body attempts to produce more insulin to digest the increased blood sugar.
- Because the pancreas cannot keep up with the increased demands, excess blood sugar circulates in the blood, causing harm.
- Insulin becomes less effective at introducing glucose into cells with time, and blood sugar levels rise.
- Insulin resistance develops progressively in type 2 diabetes. This is why doctors frequently advise patients to make lifestyle modifications in order to reduce or reverse the cycle.
Self-monitoring tips
The ability to self-monitor blood sugar levels is critical for efficient diabetic control, assisting with food planning, physical activity, and determining whether to take medicine, including insulin.
While self-monitoring blood glucose machines differ, they all feature a meter and a test strip for taking readings. It will also involve pricking the skin using a bouncing device to extract a small amount of blood.
Precautions
People should always refer to the precise instructions of a meter because equipment varies. The following warnings and measures, however, will apply to many gadgets on the market:
- Be sure that hands are clean and dry prior to touching the test strips and meter.
- To avoid external moisture influencing the result, use a test strip only once and store it in its original container.
- After testing, keep canisters closed.
- Before using, double-check the expiration date.
- Check to see if the machine requires coding before usage, which may be the case with older models.
- Keep the meter and strips in a dry, cold place.
- Bringing the meter and strips to consultations so that a primary care physician or specialist can evaluate their accuracy.
Tips
People who use a blood glucose meter to check their blood sugar levels will also prick their fingertips using a device called a lancet. While extracting blood may create anxiety in some people, bouncing the skin to collect a blood sample should be a peaceful and uncomplicated procedure. Many meters just require a teardrop-sized blood sample.
The following suggestions may also be helpful:
- Taking a blood sample with their fingertips. While some meters accept samples from other areas of the body, such as the thighs and upper arms, the fingers or outside palms provide more precise findings.
- To avoid food residue entering the gadget and altering the readout, they should clean their skin with soapy, warm water.
- Use a small, thin skin for the most comfort.
- Changing the depth settings on the skin for comfort.
- Taking blood from the side of their finger since it is less painful.
- It may be more comfortable to use the middle, ring, and little fingers.
- Using a “milking” motion to draw blood to the surface instead of applying pressure to the lancing spot.
- Observe local restrictions for disposing of sharp objects, such as lancets.
While remembering to self-monitor requires people to make lifestyle changes, it does not have to be an unpleasant task.
Diabetes Type 2 Exercise
Regular physical activity is essential for everyone. It is much more critical if you have diabetes. Your health benefits from exercise because of it:
- Lowers blood sugar levels in the short and long term without the use of medication.
- It also helps you lose weight.
- Increases blood flow and pressure.
- Increases your energy and improves your mood.
- Helps in stress management.
Before beginning any fitness regimen, consult with your clinician. If you use insulin, you may be required to take extra care before, during, and after physical exercise. The basic goal is to engage in at least 150 minutes of moderate-intensity physical activity every week.
Introduction Exercise
Physical exercise adoption and maintenance are essential foci for blood glucose management and general health in people with diabetes and prediabetes.
- Exercise is regarded as an important therapeutic schedule for type 2 diabetes since it promotes cardiovascular benefits by lowering cardiovascular risk and mortality, supporting weight management, and improving glycemic control. Increased tissue sensitivity to insulin has a positive effect on glycemic management.
- Physical inactivity and increased sedentary time have both been identified as separate and independent risk factors for cardiovascular disease, type 2 diabetes, and all-cause mortality.
- According to a comprehensive study, combined aerobic and resistance training appears to be superior to aerobic training alone, but the advantages are minor and the supporting evidence has low dependability.
- Resistance training is not recommended for patients with moderate to severe proliferative retinopathy. A shorter duration of more vigorous aerobic exercise is indicated for physically fit patients.
You can use one or both ways for a number of reasons, including:
Physical Activity and Non-insulin-dependent diabetes mellitus (NIDDM) Prevention
Maintaining an exercise routine in diabetic people is an important goal because it is linked to long-term cardiovascular benefits and lower mortality.
Diabetes risk and exercise
- Moderately active people have a 30-40% lower risk of diabetes than sedentary people.
- During the 8-year follow-up period, women who reported engaging in vigorous exercise at least once a week had a reduced incidence of self-reported type 2 diabetes than women who did not exercise regularly.
- Diabetes incidence was decreased in postmenopausal women aged 55-69 years who participated in PA compared to sedentary women.
Physical activity
- Improvements in insulin sensitivity may directly reduce the incidence of type 2 diabetes.
- This could be independent of activity’s effect on weight loss and fat distribution.
- It Is inversely linked with insulin concentrations in two high-risk diabetes populations that ranged considerably by body mass index.
- A significant amount of the benefit of physical activity on lowering insulin resistance is transient, lasting only a few days. The consistency of an individual’s activity over time is critical to receiving the effects of exercise on insulin sensitivity.
Diabetes Physical Activity Benefits
Physical activity has been demonstrated to
- Reduce cardiovascular disease risk and death
- Enhance your lipid profile and endothelial function.
- Improves insulin sensitivity, which is not limited to people with NIDDM; patients with IDDM are more insulin resistant than their non-diabetic counterparts.
- When compared to healthy controls, around 50% of patients with IDDM are overweight or obese, with larger waist and hip circumferences.
- Co-morbidities, which are frequently associated with excess body weight, decrease the benefits of good metabolic regulation.
- Controlling body weight in diabetic people is essential for lowering the risk of cardiovascular disease (CVD).
- Exercise improves weight reduction, waist circumference, fasting glucose plasma levels, and insulin serum levels.
- When compared to continuous exercise and a non-exercising control group, high-intensity training improves insulin resistance measures.
Barriers to Physical Activities
To create effective PA-promoting treatments, it is critical to address perceived obstacles to performing prescribed PA levels in this population.
Other barriers include:
Tiredness and a lack of self-motivation
- Inadequate self-efficacy
- Exercise for the elderly.
- Working hours
- Diabetes management issues Fear of being wounded or having already been injured
- Lack of self-management skills, such as the capacity to define personal aims, track progress, and reward accomplishment toward such goals
- Obstacles to exercise facilities such as parks, sidewalks, bicycle tracks, or safe and enjoyable walking paths.
There are fewer hurdles to exercise-
- Understanding of insulin pharmacokinetics
- Strategy implementation to lower the likelihood of exercise-induced hypoglycemia
- Increased social support
- Having someone with whom to engage in physical exercise.
- Long-Term Compliance and an Interprofessional Approach to Promoting Physical Exercise in Diabetes Patients
- Maintaining an exercise routine in type 2 diabetes patients is an important goal because it is linked to long-term cardiovascular benefits and lower mortality.
- Diabetes educators, such as primary care physicians, physiotherapists, and nursing professionals, play a vital role in educating patients about the benefits of exercise programs as a therapeutic alternative for disease management.
- Lifestyle changes can be difficult to implement, particularly in older adults; thus, self-management education and support focusing on general diabetes knowledge, adherence to therapy, lifestyle changes, and self-monitoring of blood glucose are critical to optimizing glycemic control to prevent or delay acute and chronic complications and improve quality of life for people with diabetes.
- In patients completing structured community programs of supervised exercise, exercise controls and confirm a reduction in medication use (and hence a reduction in expenses) as well as an improvement in clinical, metabolic, and anthropometric parameters.
- The majority of these programs demonstrated the possibility of combining a comprehensive educational intervention with a training program to promote Non-insulin-dependent diabetes mellitus (NIDDM) self-management and establish long-term behavioral changes.
Exercise Recommendations/Prescriptions
- Engage in a minimum of 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity physical activity per week, accumulated in bouts of 10 minutes or more, for notable gains in cardiorespiratory fitness and metabolic health in adults.
- The criteria for weight loss are more stringent, implying that 200-300 minutes per week are required for long-term weight loss.
- According to the Association, people with diabetes should engage in moderate-intensity aerobic activity for at least 30 minutes per day, three to seven days per week.
- Aerobic and muscle-strengthening training should be included in exercise routines.
- As a supplement to an organized exercise program, all persons with type 2 diabetes should reduce sedentary behavior time by interrupting prolonged sitting with brief periods of mild activity every 30 minutes.
- As a result, to retain the advantages of exercise, a consistent exercise routine is essential.
- The safe and effective prescription of exercise for the diabetic individual is dependent on the careful consideration of many parameters and competent clinical judgment.
- The medical history and physical examination of the individual will assist in evaluating the level of risk and the most appropriate physical activity.
The general guidelines are as follows:
Aerobic activity: 150 minutes of moderate to intense exercise each week.
Spread out your workouts over 3 to 7 days per week, with no more than 2 days in between.
To enhance insulin activity, daily exercise is advised.
Shorter periods of interval training (at least 75 minutes per week) may be enough for younger and physically fit patients. Continuous or high-intensity interval training is possible.
Resistance exercise: On nonconsecutive days, 2 to 3 times per week, conduct progressive moderate to intense resistance training.
At least 8 to 10 exercises, with two to three sets of 10 to 15 repetitions.
For older persons, flexibility and balance exercises should be done twice a week.
To maximize the benefits of exercise in type 2 diabetes, it is suggested that participants take part in supervised exercise programs.
Diabetes-specific PA advice:
- Aerobic and resistance training should be the primary focus of the PA program, as they have been found to have clear benefits in the prevention and management of diabetes and metabolic syndrome.
- All individuals with T2D should participate in an exercise regimen that includes aerobic, resistance, flexibility, and balance exercises.
- Aerobic and resistance activities should be undertaken at least three times per week because exercise-induced benefits in insulin action are transient.
- Current standards indicate 3-7 days per week of aerobic exercise, with no more than 2 days between bouts of exertion.
- Resistance exercise should be done 2-3 times a week, but never on subsequent days.
The following are some of the physiological considerations for Type 2 Diabetes:
- Hydration is essential when blood glucose levels rise above 16.7 mml/L after physical exertion. If blood glucose levels are regularly elevated, patients should visit their healthcare provider and/or a diabetes specialist before continuing their usual exercise regimen.
- If a person has type 1 diabetes, their blood glucose level should be checked for ketones if it is more than 300 mg/dl or 16.7 mm/L.
- If elevated ketones are present, activities should be postponed, the individual should hydrate, and the plan of care for elevated ketones should be followed.
- However, if the patient feels well and urine and/or blood ketones are trace or missing, it is not necessary to postpone physical activity solely because of hyperglycemia.
- When it comes to foot injuries, peripheral neuropathy is a major problem. Individuals who do not have acute ulcers can engage in light weight-bearing exercise.
- It is critical to pay close attention to appropriate footwear and any indicators of foot damage. Balance may also be impaired, which should be examined due to the increased risk of falling. Consult with a foot doctor to establish the patient’s risk.
- The risk of a heart attack and hypotension is increased by neuropathy.
- If there are unknown symptoms and feelings of acute weariness that last for more than a few minutes, physical activity should be discontinued and the individual should be advised to see their healthcare physician immediately.
- The individual may also have difficulties adjusting to temperature extremes, which should be taken into account while selecting a physical activity for that day.
- A medical evaluation is recommended, and the individual may be referred to a cardiac rehabilitation program for monitoring during exercise.
- Those who have a history of uncontrolled proliferative retinopathy should avoid activities that raise the risk of intra-ocular pressure, such as the Valsalva maneuver, which includes lifting heavy weights or unexpected loads, as may occur in contact sports.
- Individuals can engage in moderate activity in the absence of hemorrhaging.
FAQ
What foods should people with type 2 diabetes avoid?
It is preferable to avoid goods labeled ‘diabetic’ or suitable for diabetics,’ as well as consuming too much red and processed meat, as well as highly processed carbs such as white bread. Cutting back on them lowers your chances of certain malignancies and heart disorders.
Can I have a regular life despite having type 2 diabetes?
When a person is diagnosed with type 2 diabetes at a young age, it is more likely that diabetes-related complications may shorten their life. However, by using effective treatment, a person with type 2 diabetes has a high chance of living as long as who does not have diabetes.
How can I manage type 2 diabetes without taking medication?
Type 2 diabetes can be treated without medication by focusing on eating a healthy, balanced diet.
Losing weight to achieve a healthy BMI.
Having an active lifestyle.
Monitoring your blood glucose levels regularly.
What are the top three drinks that diabetics should avoid?
The three worst beverages
Soda on the regular. Soda ranks first on the list of drinks to avoid.
Energy beverages. Caffeine and carbs can both be high in energy drinks.
Fruit juices, sweetened or unsweetened.
References
- Type 2 diabetes: symptoms, causes, treatment. (2006, December 31). WebMD. https://www.webmd.com/diabetes/type-2-diabetes
- Professional, C. C. M. (n.d.-f). Type 2 diabetes. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21501-type-2-diabetes
- BridgetChapple. (n.d.). Type 2 diabetes treatments. Diabetes UK. https://www.diabetes.org.uk/diabetes-the-basics/types-of-diabetes/type-2/treatments
- Crna, R. N. M. (2023, December 20). An overview of diabetes types and treatments. https://www.medicalnewstoday.com/articles/323627#how-insulin-problems-develop
- Physical activity in diabetes. (2010, March 1). Physiopedia. https://www.physio-pedia.com/Physical_Activity_in_Diabetes#:~:text=For%20all%20adults%20with%20T2D,insulin%20action%20is%20short%2Dlived.






2 Comments