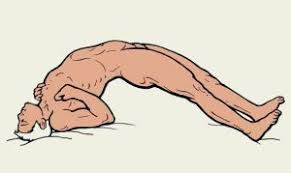
Opisthotonus Posture
What is an Opisthotonus Posture?
Opisthotonus Posture is an abnormal posture in which spastic muscle contraction of the back of muscles of the neck, trunk, and lower extremities that leads to severe abnormal backward arching from neck to heel.
Spasms of the muscles cause backward arching of the head, neck, and spine, as in severe tetanus, some kinds of meningitis, and strychnine poisoning.
Definition of Opisthotonus :
Opisthotonus or opisthotonos is a state of severe hyperextension and spasticity in which an individual’s head, neck, and spinal column enter into a complete “bridging” or “arching” position.
Though relatively rare, the condition is usually a symptom of severe neurological conditions that are life-threatening and require medical care.
Causes and associated conditions :
Opisthotonus is a symptom of some cases of severe cerebral palsy and traumatic brain injury or as a result of the severe muscular spasms associated with tetanus. It can be a feature of severe acute hydrocephalus, poisoning, and drowning.
Meningitis: When an infection causes inflammation of the tissues that surround the brain and spinal chord. The majority of cases in the United States are viral, but bacteria and fungi can also cause the condition.
Tetanus: Caused by toxins produced by the bacteria Clostridium tetani, which damage the nervous system and brain tissue. Tetanus is often called lockjaw because its most common symptoms are a locked jaw, stiff neck, and trouble swallowing.
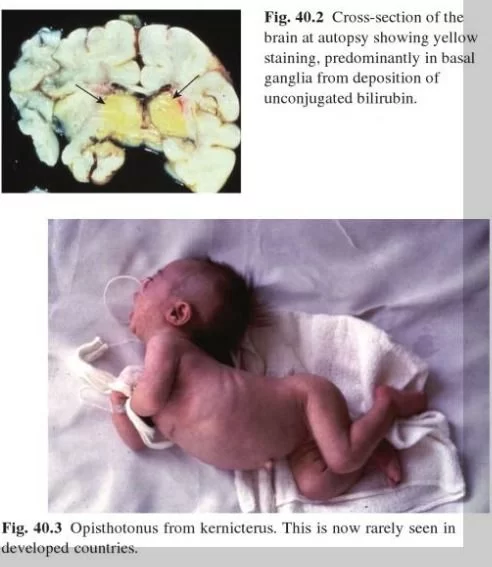
Infants: Opisthotonus is more pronounced in infants. Opisthotonus in the neonate may be a symptom of meningitis, tetanus, severe kernicterus, or the rare Maple syrup urine disease. This marked extensor tone can cause infants to “rear backwards” and stiffen out as the mother or nurse attempts to hold or feed them. Individuals with opisthotonus are quite challenging to position, especially in wheelchairs and car seats.
Opisthotonus can be triggered by any attempt at movement, such as smiling, feeding, speech, or by involuntary movements, such as seizures. Similar tonic posturing may be seen in Sandifer syndrome.
Poisoning: Opisthotonus can sometimes be seen in lithium intoxication. It is a rare extrapyramidal side effect of phenothiazines, haloperidol, and metoclopramide.
Opisthotonus with the presence of the risus sardonicus is also a symptom of strychnine poisoning and prussic acid (hydrogen cyanide) poisoning.
Phenothiazines: These are drugs commonly used to treat certain mental health conditions, such as schizophrenia. Opisthotonos is a rare side effect, and symptoms usually go away once the person has stopped taking the drugs.
Krabbe disease: An inherited condition that mostly impacts infants, young children, and young adults. Krabbe disease causes loss of muscle control and seizures that do not respond to treatment and can lead to premature death.
Gaucher disease: Fat-filled cells build up in organs, especially the liver and spleen, causing them to swell; fat cells also affect the bone marrow, causing bone pain. One severe form of Gaucher disease can cause opisthotonus in infants, but this is rare.
Bilirubin encephalopathy, or kernicterus: A brain dysfunction that can potentially cause irreversible brain damage. Newborns and adults with pre-existing liver conditions have a higher risk of bilirubin encephalopathy.
Infant alcohol withdrawal: This occurs when a pregnant woman drinks excessive amounts of alcohol while pregnant. Infant alcohol withdrawal can cause reduced or uncontrollable muscle function. It rarely causes opisthotonos, however.
Other causes include conditions that involve increased cranial pressure, such as:
- Brain hemorrhage or bleeding: This occurs when injury, disease, congenital disabilities, or blood vessels in the brain rupture, causing blood to accumulate and put pressure on brain tissues.
- Hydrocephalus: Congenital disability, injury, or disease cause cerebral spinal fluid (CSF) to accumulate, putting pressure on the brain.
- Subarachnoid hemorrhage: This happens when bleeding occurs between the brain and the tissues surrounding it.
- Brain tumor: An abnormal, often uncontrollable cellular growth that can put pressure on the brain tissues and disrupt nerve function.
- Chiari malformation: Part of the lower brain pushes out through the spinal canal, increasing pressure on the spine, brain, and often interfering with fluid flow causing hydrocephalus. Only some types of Chiari malformation do this.
Drowning and the “dinosaur death pose”
Opisthotonus is seen with drowning victims – called the “Opisthotonic Death Pose”. This pose is also common in complete dinosaur skeletal fossils and it has been suggested that this is due to the animal drowning or being immersed in water soon after death.
Other causes :
Opisthotonus is also described as a potential CNS symptom of heat stroke along with bizarre behavior, hallucinations, decerebrate rigidity, oculogyric crisis, and cerebellar dysfunction.
Opisthotonus is a symptom of “Lavender Foal Syndrome”, a lethal genetic disorder in horses.
Symptoms of Opisthotonus Posture
- Opisthotonos causes the back to become extremely rigid and curved or arched. The heels and head usually bend or flex backward as far as possible in response.
- If someone is on their back, they will arch upwards, forming an n-shape. In this position, the back usually lifts the back off floor or mattress to some extent.
- The arms also bend towards the body. In some cases, the head and lower body may be the only part of the body to keep in contact with the ground.
- If someone is on lying on their stomach when opisthotonos occurs, they will bend inward creating a U-shape. The legs and arms usually reach backward and upward.
- If the condition occurs when someone is lying on their side, the arching will form a C-shape. The person’s knees bend, and their arms either bend in or extend straight out. In this position, the backward arching of the neck may be more noticeable or severe.
- Severe spasm in the full body due to tetanus or other causes.
Aside from these postural symptoms, the signs of opisthotonos vary depending on the cause.
When to see a doctor?
People should seek medical attention anytime severe muscle spasms occur. Opisthotonos is considered life-threatening and is associated with serious health complications.
Symptoms that may accompany opisthotonos and require emergency care include:
- trouble breathing
- difficulty swallowing
- rapid heart rate
- a bluish tone in the fingers and toes
- stiff jaw, neck, and abdominal muscles
- extreme pain and soreness in the neck, shoulders, and muscles that surround the spine
- high fever
- convulsions
- uncontrollable vomiting
- reduced alertness or response time
- dilated pupils or vision problems
- extreme and unexplainable exhaustion
Because the condition mostly affects infants and young children, these symptoms may be harder to pinpoint. Uncontrollable, persistent crying with muscle spasms may be a sign of opisthotonos.
Infants may sleep more than usual but are restless, continually waking to adjust or find a more comfortable position.
Diagnosis :
Doctors diagnose opisthotonos by observing the posture when it is happening. Doctors are usually more focused on identifying and quickly treating the underlying cause than confirming opisthotonos.
Tests used to diagnose the causes of opisthotonos include:
- complete blood and urine tests
- magnetic resonance imagining (MRI) of the brain
- electrolyte tests
- lumbar puncture (spinal tap)
- cerebrospinal fluid (CSF) culture test
- computed tomography (CT) scan
Medical Treatment :
Treatment options depend on the underlying cause of opisthotonos. Commonly used treatment plans include:
- Antibiotics for bacterial-based infections, such as meningitis and tetanus. Antibiotics are also prescribed to prevent infection or further bacterial infections after surgery.
- Over-the-counter pain medications, increased fluid intake, and rest are recommended for most cases, especially viral infections, such as meningitis.
- Intravenous fluids are usually given in severe cases to counteract bronchodilator overdoses.
- Surgery is often necessary in cases of trauma, bleeding, and Chiari malformation to reduce pressure on the brain.
- Antitoxin injections or medications are often given to those with tetanus to limit excess tissue damage associated with severe infection.
- A ventilator and oxygen may be used when breathing is limited, labored, or difficult.
Prevention
There are vaccines that offer protection against some of the conditions that cause opisthotonos, such as tetanus and some types of bacterial meningitis.
Other ways to reduce the chances of developing opisthotonos:
- washing hands frequently
- cleaning bathroom and kitchen surfaces regularly
- avoiding contact with those who have infectious conditions
- monitoring high fevers carefully, especially in infants and young children
- quickly identifying and treating brain injuries
Physiotherapy treatment:
- Remove the cause
- Spasticity and Spasm Management:
Physiotherapy can help with muscle spasms through different methods of treatment. These can be aimed at treating the symptoms and the cause (if there is an underlying injury). Physiotherapy treatment can help decrease the tension in the muscle and provide pain-relieving strategies.
Treatments :
Treatments for muscle spasms can include:
Massage: Massage is a manual technique used to promote healing and reduce muscle tension. It is often used in conjunction with trigger point therapy. There are many different forms of massage but the common type of massage used in physiotherapy is deep friction massage. This treatment involves applying pressure deep into the muscle to relieve tension and promote healing.
Deep friction massage works to release tension in deep muscles either after injury or after high load activity. After an injury or high loading, the muscles are damaged and contract to allow for repair and protection of further damage. It also helps to relax the muscle which actually promotes the healing process and a quicker recovery is made. Pain will be experienced at the time and up to a few days following the massage; however, improvements should be felt after this.
Manual therapy: Manual therapy interventions are found to be very beneficial in the treatment of this condition. Techniques of joint mobilization, deep tissue mobilization and muscular retraining are proven to be significantly effective treatments. Specific exercises to improve blood flow through the muscles are beneficial. An individualized exercise program is developed for each patient’s specific problem often focusing on the deep neck muscles and the postural muscles of the shoulders and shoulder blades. Re-education of breathing patterns is also found to be helpful. Relaxation techniques and assistance in stress management are key components of the treatment when stress is noted to be a significant source of the symptoms. Education on proper techniques and postures for work, athletic and daily activity is an essential component of treatment.
Specific exercises to improve blood flow through the muscles are beneficial. An individualized exercise program is developed for each patient’s specific problem often focusing on the deep neck muscles and the postural muscles of the shoulders and shoulder blades. Re-education of breathing patterns is also found to be helpful. Relaxation techniques and assistance in stress management are key components of the treatment when stress is noted to be a significant source of the symptoms. Education on proper techniques and postures for work, athletic and daily activity is an essential component of treatment.
Forms of Manual Therapy :
There are a lot of different avenues therapists can take to use manual therapy to help the patient’s condition. Some of the different forms include:
- Myofascial trigger point therapy
- Soft tissue mobilization/manipulation
- Muscle energy techniques
- Proprioceptive therapy
- Strain-counterstain
Trigger Point Dry Needling Therapy at Results Physiotherapy
What is Dry Needling: Dry Needling is a specific treatment technique used on muscle trigger points that are creating pain and discomfort. The treatment uses a thin, sterile, solid filament needle inserted into the skin to stimulate the underlying myofascial trigger points. The procedure is called Dry Needling because no liquid or medication is injected into the patient.
How Dry Needling works: When the muscle is stimulated with the needle, a twitch or rapid depolarization of the fibers takes place. This removes the compression on the joint, nerve, or vascular tissue. As a result, the muscle activity reduces dramatically, allowing it to relax and the pain and dysfunction to decrease.
Occasionally, when the needle is inserted a patient will feel “referred pain.” This is usually a positive sign confirming the trigger point as the cause of the patient’s pain.
Treatment for Cramps :
The first and foremost priority of treatment for cramps is identifying the root cause of your cramps. Whether this be tight muscles, over-exercising, or a cause that requires further investigation. Our physiotherapists are experienced in finding out what it is that is causing your cramps and will point you in the right direction.
Depending on what our physiotherapists find, treatment may involve:
- Lengthening of hypertonic muscles.
- Restoring joint range of motion.
- Strengthening weak muscles.
- Lifestyle modifications:
- Fluid intake.
- Reducing coffee/alcohol intake.
- Vitamin/electrolyte balancing.
- Modifying current exercise regimes.
Stretching Exercise:
Stretching the area that has the muscle spasm can usually help improve or stop the spasm from occurring. Below are stretches for the muscles in your calves, thighs, back, and neck.
4 stretches for calf muscle spasms
To do the first stretch:
- Lie down, stretching your leg by pointing or pulling your toes toward your head. (Pointing the toes toward you is called dorsiflexion.)
- Hold for a few seconds or until the spasm stops.
- You can also use a strap or belt looped around your foot to gently pull the top of your foot toward you.
- This also works for a hamstring muscle spasm. Other stretches to do:
- Stand and put your weight on the cramped leg, bending your knee slightly.
- Stand on your tiptoes for a few seconds.
- Lunge forward with the leg that isn’t cramped, keeping the cramped leg straight.
Stretch for thigh spasms
- Stand and hold on to a chair for balance.
- Bend your leg at the knee and reach your leg backward from the hip.
- Holding your ankle, pull your foot up behind you toward your buttock.
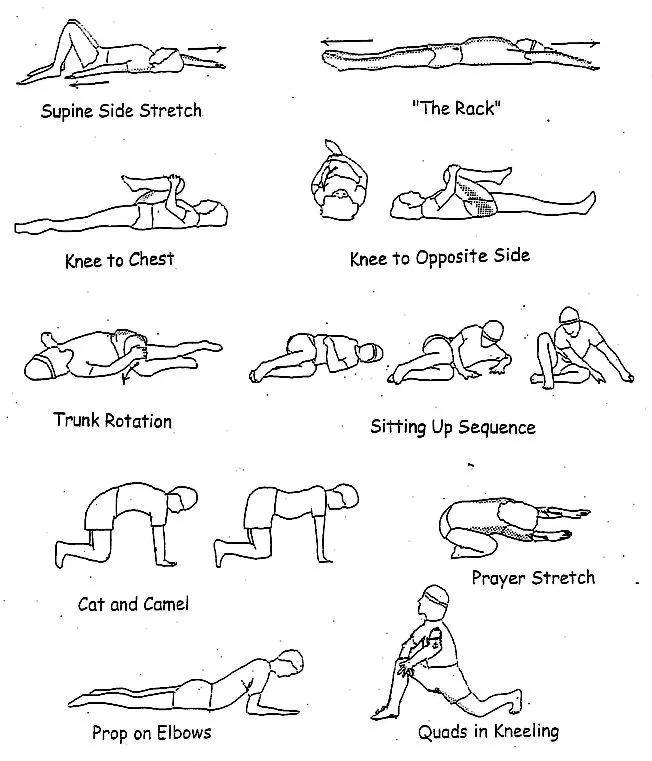
Stretches for back spasms
The first and easiest way to stretch a back spasm is to walk around, which can loosen your back muscles and relieve a spasm. Walk at a slow, steady pace to loosen your back muscles.
Tennis ball stretch:
- Lie down on the floor or on a bed with a tennis ball (or another small ball) under the area with the spasm for a few minutes.
- Try to relax and breathe normally.
- Move the ball to an adjoining spot and repeat.

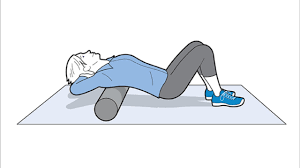
Foam roller stretch:
- Lie on the floor with a foam roller perpendicular to your spine.
- Move your back over the roller, up to your shoulder blades, and down to your belly button.
- Keep your arms crossed on your chest.
Exercise ball stretch:

- Sit on an exercise ball and lie back, so that your back, shoulders, and buttocks are stretched out on the ball, with your feet flat on the floor. Do this near a chair or couch so that you can hold on if you lose your balance.
- Lie stretched out for a few minutes.
Stretch for neck spasms
- While sitting or standing, circle your shoulders by rolling your shoulders forward, up, back, and down. Repeat this motion 10 times.
- Then roll your shoulders in the opposite direction by moving your shoulders back, up, forward, and down. Repeat 10 circles in this direction.
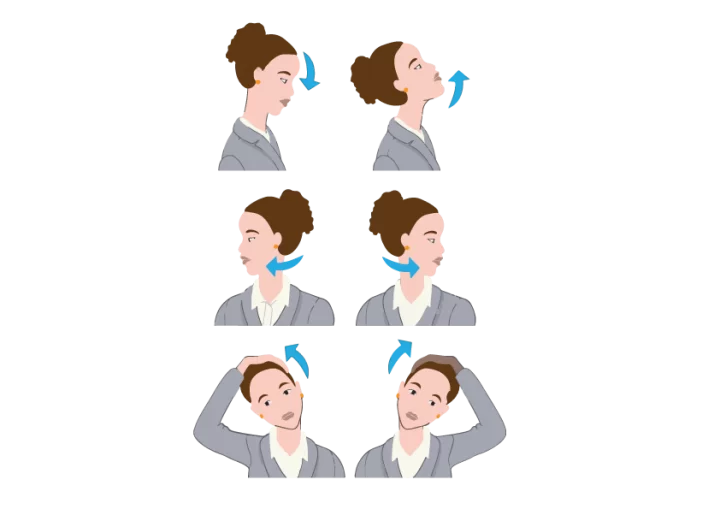
- You can perform shoulder rolls anywhere, while sitting in a car, at a desk, or if you’re standing in line somewhere waiting.
- Different upper limb stretch :
Pain Management: TENS (Transcutaneous electrical nerve stimulation) :
A TENS unit has controls that allow people to administer an appropriate level of pain relief. People can achieve this by altering the following aspects of the electrical current:
Intensity: A dial allows the user to adjust the intensity of the electrical stimulation.
Frequency: The frequency refers to the number of electrical pulses per second. High-frequency (HF) pulses range from 80 to 120 cycles per second and may help manage acute pain. Low-frequency (LF) pulses range from 1 to 20 cycles per second and are suitable for the treatment of chronic pain.
Duration: The duration is the number of microseconds that the current enters the skin during each pulse.
Heat therapy or Ice therapy
Treating pain and spasms with hot or cold therapy can be extremely effective.
For a persistent spasm, apply an ice pack on the muscle for 15 to 20 minutes at a time, a few times a day. Make sure to wrap the ice in a thin towel or cloth so that the ice isn’t directly on your skin.
A heating pad on the area may also be effective for 15 to 20 minutes at a time, but follow this with an ice pack. This is because while heat feels good for pain, it may worsen inflammation. Ice will calm down the inflammation.
Other heat options include a warm bath, hot shower, or a hot tub or spa if you have access to one, which can all help relax your muscles.
Relaxation therapy: Progressive muscle relaxation is a relaxation technique that requires an individual to focus on flexing and holding a certain set of muscles and then slowly relaxing those same muscles. As the individual flexes and releases those muscles from top to bottom they will feel a deep sense of relaxation.
The long-term goal of this relaxation technique is to be able to identify when your body’s muscles are suffering the effects of stress and to be able to relax the individual and the individual’s muscles when directed.
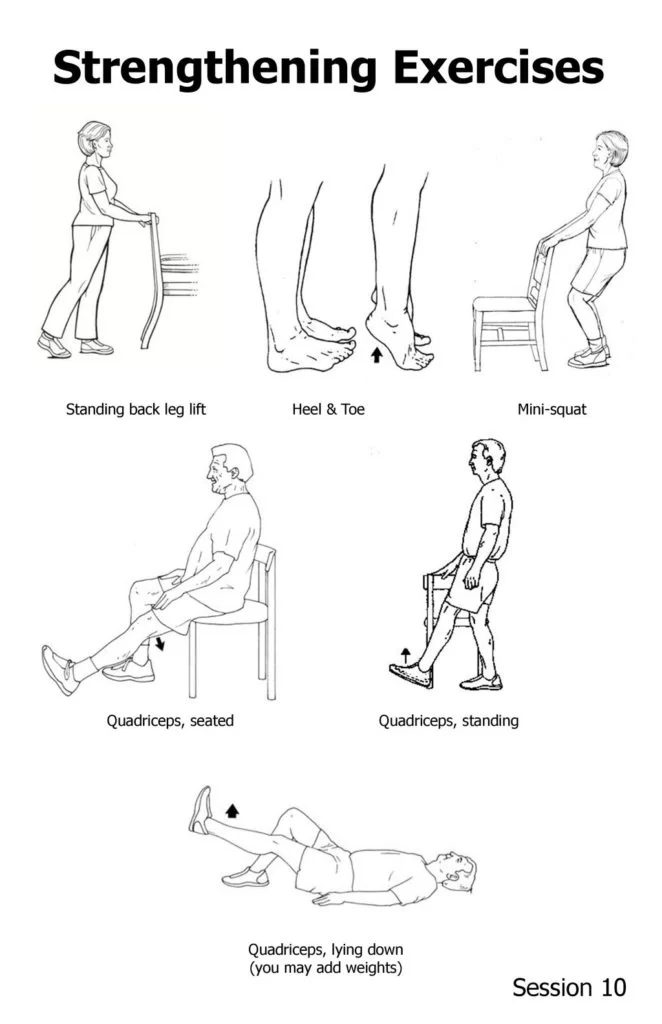
Strengthening exercise:
FAQs
What causes opisthotonus?
Opisthotonus is caused by various medical conditions affecting the nervous system. It involves severe and sustained muscle spasms that lead to the body arching backward and becoming rigid. Common causes include tetanus, a bacterial infection affecting the nervous system, and conditions like meningitis and encephalitis, which cause inflammation of the brain or its protective membranes. Brain injuries, seizures, and poisoning with certain toxins can also lead to opisthotonus. Birth-related trauma or neurological disorders may result in this condition, particularly in infants.
What is opisthotonos position in tetanus?
Opisthotonus is a type of abnormal posture in which muscular spasms cause the back to arch significantly. Typically, the condition is a symptom of more severe brain disorders such as meningitis, tetanus, and trauma.
What is opisthotonus position in newborns?
Opisthotonosis is a disorder of abnormal posture caused by severe muscle spasms. Due to the incomplete development of their neurological systems, infants and young children are the most affected. It can cause very serious conditions, thus immediate medical care is frequently required.
Which position is seen in Opisthotonus?
In opisthotonus, the body assumes a characteristic position characterized by severe and sustained muscle spasms. The position typically involves arching of the back and neck, with the head and heels being the only points of contact with the surface. The body forms a rigid, arched bridge-like shape with the back and neck hyperextended, and the arms and legs may be stiffly extended as well.



One Comment