Wilson’s Disease
What is Wilson’s disease?
Wilson’s disease, also known as hepatolenticular degeneration, is a rare genetic disorder characterized by the accumulation of copper in the body, primarily affecting the liver and brain. It is an autosomal recessive disorder, which means that an individual must inherit a mutated gene from both parents to develop the condition.
(Wilson’s Disease; Inherited Copper Toxicity)
Also called: hepatolenticular degeneration.
- Wilson disease is a genetic disorder.
- An inherited disorder.
- It prevents the body from removing extra copper. That causes copper to build up in the liver, brain, eyes, and other organs.
- Copper plays a major role in the growth of your healthy nerves, bones, collagen, and the skin pigment melanin. Normally,
- copper is absorbed from your food, and superfluous is excreted through a substance produced in your liver (bile).
- If copper is not eradicated properly and instead of assemble, it possibly may lead to a life-threatening level.
- Your body requires a small amount of copper from food intake to stay healthy, but too much copper is harmful. Without
- treating Wilson’s disease it may lead to high copper levels that cause life-threatening organ damage.
How common is Wilson’s disease?
- Wilson’s disease is rare.
- Less than 100 thousand cases per year (India)
- Earliest studies demonstrate that about 1 in 30,000 people have Wilson’s disease. Another reason might be that some people have gene mutations for Wilson’s disease but don’t develop the disease
Who is more likely to have Wilson’s disease?
- People have a greater possibility of having Wilson’s disease if they had a family history, particularly if they have a first-degree relative—a parent, sibling, or child—who has Wilson’s disease.
- People with Wilson disease usually develop symptoms between the ages of 5 and 40. Few people also develop symptoms at younger or older ages.
Pathophysiology:
The genetic hinder in Wilson disease diminishes copper transport. The diminished enrapture decreases copper secretion into the bile, thus it origin copper profusion and results in an assemblage in the liver, which begins at birth. The impede convey also restrains a confederation of copper into the copper protein ceruloplasmin, which declines serum levels of ceruloplasmin.
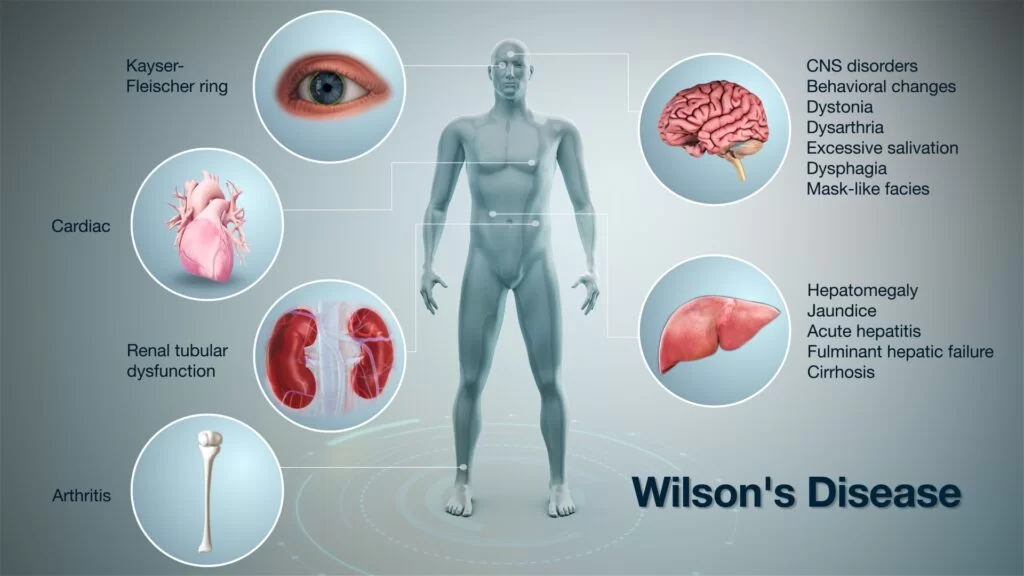
Hepatic fibrosis develops, ultimately causing cirrhosis. Copper disperses out of the liver into the blood, then into other tissues. It is most devastating to the brain, but also it damages the kidneys and reproductive organs and causes hemolytic anemia. Few coppers garner throughout the rim of the cornea and edge of the iris, causing Kayser-Fleischer rings. The rings seem to encircle the iris.
Staging of Wilson Disease:
Stage 1: initial accretion of copper in the liver
Stage 2: Acute reallocation of copper within the liver, followed by release into the systemic circulation
Stage 3: Chronic assemblage of copper into extrahepatic tissues including brain
Stage 4: Use of chelation therapy to reinstate copper balance
What are the complications of Wilson’s disease?
- Liver failure
- Acute kidney failure
- Cirrhosis
- Encephalopathy
- Splenomegaly
- Ascites
- Variceal bleeding
- Hepatorenal syndrome
- Neuropsychiatric manifestations
- Death
Untreated, Wilson’s disease can be fatal.
Wilson’s disease can initiate complications, but early diagnosis and treatment can decline your feasibility of expanding them.
Acute liver failure:
Wilson disease may escort to acute liver failure, a condition in which your liver fails promptly without warning. This can occur suddenly, or it can develop gradually over the years. Around 5 percent of the people with Wilson disease present with acute liver failure, when they are first diagnosed. It most frequently requires a liver transplant.
Acute kidney failure: People who have acute liver failure due to Wilson’s disease have a type of anemia known to be hemolytic anemia.
Cirrhosis:
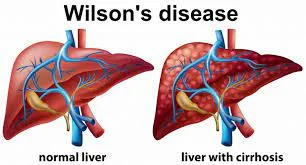
Scarring of the liver is known as cirrhosis. As liver cells try to make mend the damage done by a profusion of copper, scar tissue forms in the liver, essence it more strenuous for the liver to function. In cirrhosis, scar tissue restores healthy liver tissue and inhibits your liver from working ordinarily. Scar tissue also partially inhibits the flow of blood through the liver. As the cirrhosis gets worse, the liver begins to fail. About 35 to 45 percent already have cirrhosis at the time of recognition. Cirrhosis increases your possibility of getting liver cancer. Cirrhosis may ultimately lead to liver failure. Because of liver failure, your liver is badly impaired and stops working. Liver failure is also known as end-stage liver disease. This condition might require a liver transplant.
Persistent neurological problems: Tremors, clumsy gait, involuntary muscle movements, and difficulty in speech frequently get better with treatment. Although, some people have diligent neurological difficulties despite treatment.
Kidney problems: kidney stones
Psychological problems: involves personality changes, depression, irritability, bipolar disorder, or psychosis.
Blood problems: These might include the destruction of red blood cells (hemolysis) leading to anemia and jaundice.
Epidemiology:
Incidence: 1 in each 30,000 population with a bearer frequency of 1 in each 90. There are some individual populations that have a greater incidence due to the increased rate of consanguinous marriages. Both males and females are afflicted equally. The actual age of demonstration is four to 40 years of age, but this disorder has been identified in children as young as three as well as adults as old as 70.
Symptoms:
What are the symptoms of Wilson’s disease?
Symptoms are shown since birth but don’t arrive until the copper builds up in the brain, liver, or other organs. It’s vary depending on the affected parts of your body by the disease. Symptoms typically start between the ages of 12 and 23. Some people do not have symptoms of Wilson’s disease before they are diagnosed with the disease and treated. If symptoms are existing, can be associated with your liver, nervous system, mental health, eyes, and other organs.
Liver symptoms:
People with Wilson disease may evolve symptoms of hepatitis, or inflammation of the liver. In a few cases, people develop these
symptoms when they have acute liver failure.
They can include:
- swelling
- Fatigue, lack of appetite, or abdominal pain
- jaundice
- Golden-brown eye discoloration (Kayser-Fleischer rings)
- Fluid buildup in the legs or abdomen
- Problems with speech, swallowing, or physical coordination
- Uncontrolled movements or muscle stiffness
- feeling tired or weak
- nausea and vomiting
- poor appetite
- pain over the liver, (upper part of the abdomen)
- darkening of the color of urine
- lightening of the color of the stool
- losing weight without trying
- ascites
- edema
- itchy skin
- jaundice
Nervous system and mental health symptoms:
People with Wilson disease may evolve the nervous system and mental health symptoms after copper builds up in their bodies. These symptoms are most common in adults but also occur in children.
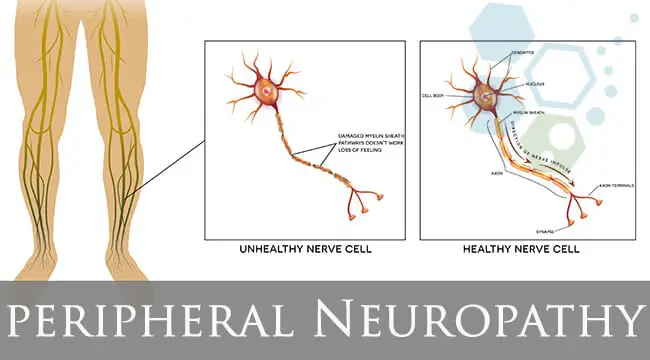
Nervous system symptoms may include:
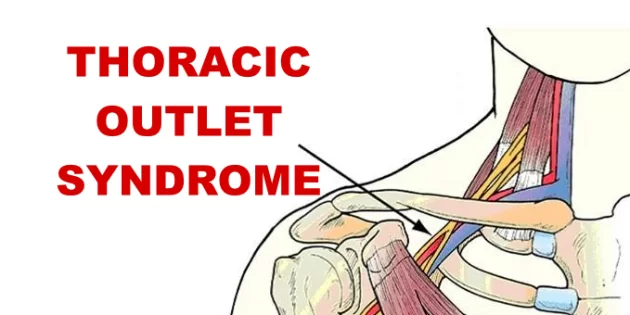
- problems with speech, swallowing, or physical coordination
- stiff muscles
- tremors
- Mental health symptoms may include:
- anxiety
- changes in mood, personality, or behavior
- depression
- psychosis
Eye symptoms:
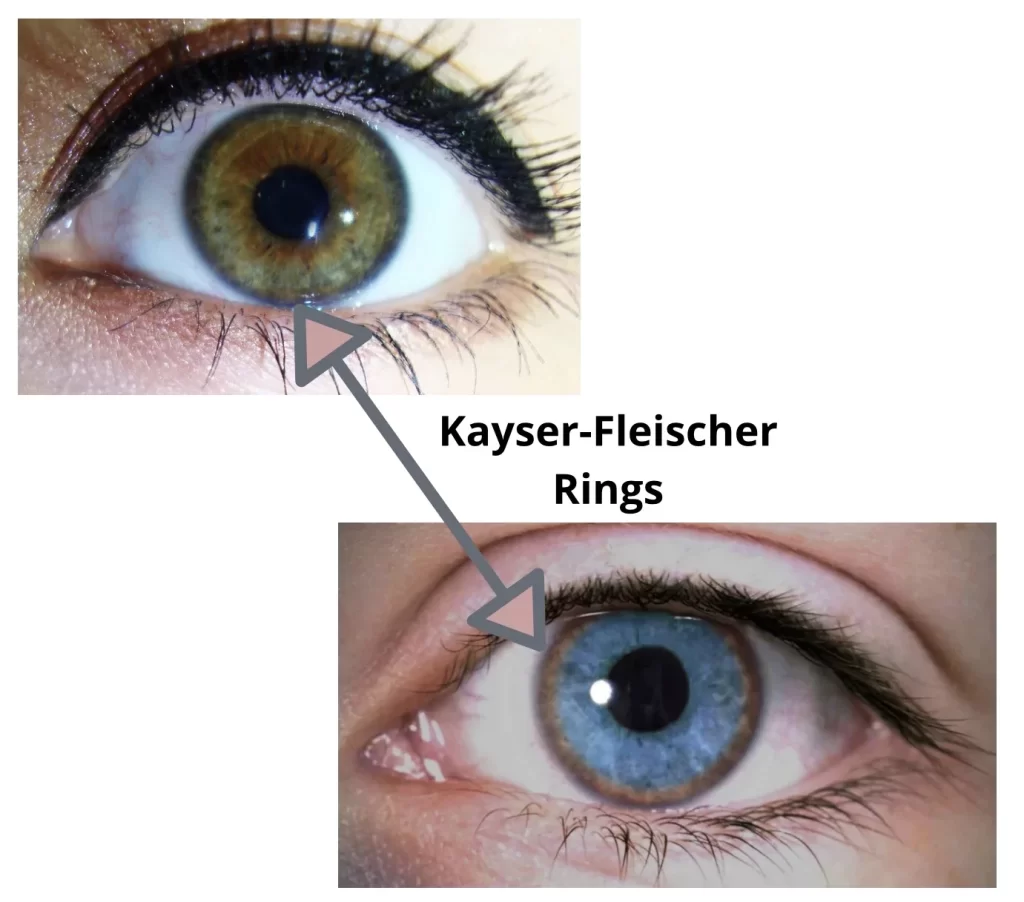
- The people with Wilson disease have Kayser-Fleischer rings. It looks like a greenish, gold, or brownish or reddish-green, 1 to 3mm wide ring around the edge of the corneas. An escalation of copper in the eyes enterprise Kayser-Fleischer rings. A doctor can diagnose these rings during a special eye exam known to be a slit-lamp exam.
In the population who have nervous system symptoms, more than 9 out of 10 have Kayser-Fleischer rings. In the people who are only present with liver symptoms, 5 or 6 out of 10 have Kayser-Fleischer rings. - They don’t transpire in all persons with Wilson’s disease but may be seen in people with chronic cholestasis. Wilson’s disease is also associated with sunflower cataracts airing by brown or green pigmentation of the anterior and posterior lens capsules. Neither causes reminiscent visual loss.
- KF rings occur in approximately 66% of diagnosed cases (more often in those with neurological symptoms rather than with liver problems).
Kidneys: kidney problems, like renal tubular acidosis, and kidney stones.
Type-2-renal tubular acidosis is a type of disorder of bicarbonate driven by the proximal tubules that lead to nephrocalcinosis (known to be a calcium accumulation in the kidneys), a weakening of bones (because of calcium and phosphate loss), and periodic aminoaciduria (it is a loss of essential amino acids needed for protein synthesis).
Heart: It is a rare, but recognized problem in Wilson’s disease; it may direct to heart failure and cardiac arrhythmias. heart problems, such as cardiomyopathy
Hormones: hypoparathyroidism, infertility, and recurrent miscarriage.
Other symptoms and health problems:
Wilson disease can also affect other parts of your body.
including:
- hemolytic anemia
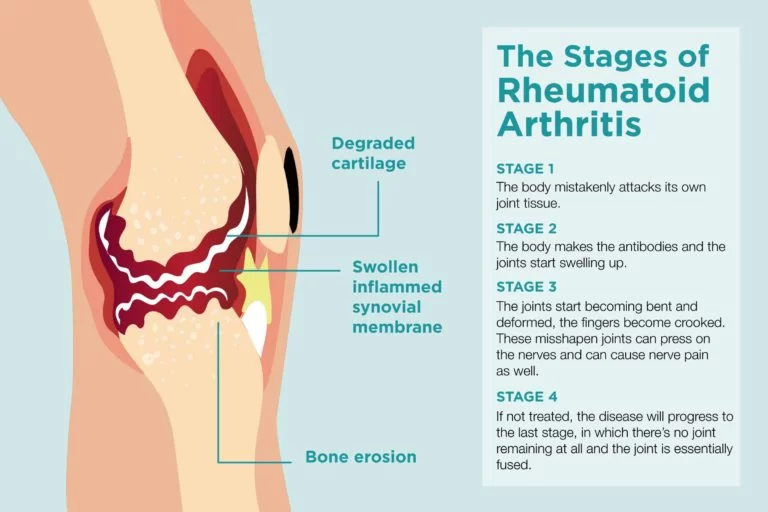
- arthritis or osteoporosis
- kidney problems, like renal tubular acidosis, and kidney stones.
Neuropsychiatric symptoms:
- About half of the people with Wilson’s disease have neurological or psychiatric symptoms.
- Most originally have mild cognitive deterioration and clumsiness, as well as changes in behavior.
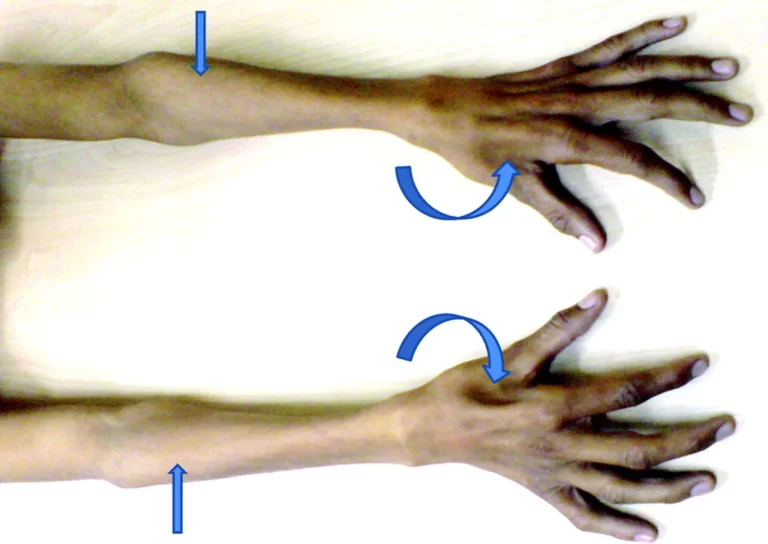
- Specific neurological symptoms frequently then follow, often in the form of parkinsonism with or without a typical hand tremor, masked facial expressions, slurred speech, ataxia, or dystonia.
- Seizures and migraine arrive to be more common in Wilson’s disease.
- A characteristic tremor described as a “wing-beating tremor” is confronted in many people with Wilson’s; this is distracted at rest but can be evoked by abducting the arms and flexing the elbows toward the midline.
- Cognition can also be pretentious in Wilson’s disease, in two, not requite absolute, categories – frontal lobe disorder (may present as impulsivity, impaired judgment, promiscuity, apathy, and executive dysfunction with poor planning and decision-making) and subcortical dementia.
- These cognitive involvements are thought to be associated with and closely linked to psychiatric manifestations of the disease.
Psychiatric problems:
- Wilson’s illness is associated with behavioral abnormalities, depression, anxiety problems, and psychosis.
- Psychiatric symptoms are commonly seen in conjunction with neurological symptoms and are rarely demonstrated on their own.
- These symptoms are often poorly defined and can sometimes be imputed to other causes.
- Because of this, a diagnosis is sporadically made when only psychiatric symptoms are present.
What causes Wilson’s disease?
[Autosomal recessive inheritance pattern]
- Wilson’s disease is an inherited autosomal recessive trait, that develops the disease a mutated copy of the gene from both parents or they are passed from parent to child.
- If you have the gene, only one aberrant gene is present, and you will not become ill, but you are a carrier and can carry the gene and pass it on to your children.
- Wilson’s disease is caused by a mutation in the Wilson disease protein (ATP7B) gene present on chromosome 13 which controls the protein transporter responsible for excreting excess copper into bile and out of the body.
- The gene mutations forbid the body from discarding the extra copper. Conventionally, the liver divulges extra copper into the bile.
- Then bile fascinates the copper, with other toxins and waste products, out of the body through the digestive tract.
- The protein conveyer is located in the trans-Golgi network of the liver and brain. The main route of copper excretion (95%) is through the liver.
- This reserve copper first assembles in the liver and then tumbles into the blood and then into other organ systems.
- The excess copper leads to the generation of free radicals that causes the oxidation of vital proteins and lipids.
- Early swap lean occurs in the mitochondria, nuclei, and peroxisomes.
- This protein transports surfeit copper into the bile, where it is excreted in waste products.
Risk factors:
- People have an increased risk of Wilson’s disease if their parents or siblings have the condition.
Diagnosis of Wilson Disease
How do doctors diagnose Wilson’s disease?
Diagnosed by your medical and family history, a physical exam, an eye exam, and tests.
Medical and family history:
The doctor asks about your family and personal medical history of Wilson’s disease and also involves the other conditions that may lead to your symptoms.
Physical exam:
During a physical exam, the doctor will examine for signs of liver damage such as:
- changes in the skin
- enlargement of the liver or spleen
- tenderness or swelling in the abdomen
- edema
- jaundice
Eye exam:
During a slit-lamp exam, doctors use a slit lamp to examine a patient’s eyes.
Doctors use a slit-lamp exam to diagnose for Kayser-Fleischer rings.
What tests do doctors use to diagnose Wilson’s disease?
Doctors mostly recommended lab tests mainly blood tests and a 24-hour urine collection test to identify Wilson’s disease. And also uses liver biopsy and imaging tests.
Blood tests:
- Including tests that check amounts of ceruloplasmin (it is a protein that carries copper in the bloodstream).
- People who have Wilson disease frequently have low ceruloplasmin levels.
People may also have lower than normal blood copper levels. - Acute liver failure due to Wilson disease can lead to high blood copper levels.
And also have abnormal ALT (alanine transaminase) and AST (aspartate transaminase) levels. - Doctors can also order a blood test to check for the gene mutations that lead to Wilson’s disease if other all medical tests do not validate a diagnosis of the disease.
24-hour urine collection test:
Till 24 hours, your urine will be collected at home in a special container, which is copper-free, that is given by a healthcare professional. Then they will be sent the urine to a lab, where the amount of copper in the urine will be checked. In Wilson’s disease, the copper levels in the urine are always higher than in normal individuals.
Liver biopsy:
If the results of blood and urine tests are unsuccessful, then the doctor may order a liver biopsy. During the time of the liver biopsy, the doctor will take a small specimen of tissue from your liver. The pathologist will examine the tissue to accent the specific liver diseases, for liver damage and cirrhosis, and also to check the amount of copper in the tissue.
Imaging tests:
magnetic resonance imaging (MRI): This uses radio waves and magnets to produce detailed images of organs and soft tissues without using X-rays.
computed tomography (CT) scan:
Differential Diagnosis:
- Differential diagnosis includes conditions causing chronic active hepatitis and hemolytic anemias due to various causes.
Treatment:
Medication:
Medical treatments are available for Wilson’s disease. Some medicines increase the removal of copper from the body, while others prevent the absorption of copper from the diet.
- penicillamine
- trientine hydrochloride
- zinc acetate prescription called Galzin
- dimercaprol
Doctors treat Wilson’s disease with chelating agents and zinc. The medicines which remove the copper from the body are called chelating agents.
And zinc will prevent the intestines from absorbing the copper. In innumerable cases, treatment may improve or prevent symptoms and organ damage. Doctors may also suggest changing your diet to avoid foods that contain high copper. People with Wilson’s disease require lifelong treatment to oversee symptoms and reduce or prevent organ damage. Stopping treatment may cause acute liver failure or cirrhosis with liver failure, may need a liver transplant. Doctors regularly conduct blood and urine tests to check how the treatment is working.
Medicines that are used to remove copper from the body, to treat Wilson’s disease are:
two chelating agents – Penicillamine (Cupramine, Depen) and trientine (Syprine)
Penicillamine is further anticipated to cause side effects than trientine. Side effects of penicillamine are fever, rash, kidney problems, or bone marrow problems. Also, it can decrease the activity of vitamin B6, so doctors may prescribe taking a vitamin B6 supplement along with penicillamine. In a few cases, when people with nervous system symptoms start to take a chelating agent, as their symptoms get worse.
When treatment begins, the dose of chelating agents increases gradually to the doctors. People take higher doses of chelating agents until the extra accumulated copper has been removed from the body. When Wilson’s disease has been identified and confirmed by the tests showing that copper is at defended levels, then doctors may advise lower doses of chelating agents for the continuation of the treatment. Lifetime treatment inhibits copper from accumulating again. Chelating agents may restrain wound healing, and doctors may prescribe a lower dose of chelating agents for people who are preparing to have surgery.
Zinc:
Zinc intercept the intestines from absorbing copper. Doctors may prescribe zinc as a maintenance treatment after chelating agents have removed extra accumulated copper from the body. Doctors can also prescribe zinc but do not yet have symptoms.
The most recurrent side effect of zinc is stomach upset.
How do the doctors treat Wilson’s disease in a pregnant woman?
- In pregnancy, women should continue the treatment for Wilson disease throughout pregnancy. Doctors prescribe a lower dose of chelating agents for women who are pregnant. Since the fetus needs a little amount of copper, lowering the dose may keep copper at safety levels without removing too much copper.
- In most cases, doctors suggest that women must continue to take the full dose of zinc during the pregnancy. Experts advised
women with Wilson disease can’t breastfeed their babies if they are taking chelating agents. Because Penicillamine is present in breast milk and may be harmful to a baby.
Eating, Diet, & Nutrition:
If you have symptoms of Wilson’s disease, talk with your doctor about your diet and foods that contain copper.
When treatment begins, your doctor may recommend avoiding foods that are high in copper, such as
- chocolate
- liver
- mushrooms
- nuts
- shellfish
After maintained treatments have decreased your copper levels, take advice from your doctor about whether you can eat moderate amounts of these foods or not. If you are using tap water, which comes from a well or runs through copper pipes, then make sure that the copper levels in your water are checked. Water gathered in your copper pipes may pick up copper. Always remember to run the water to flush the pipes before you drink the water or use it for cooking. And need to use a water filter to remove copper from your tap water. For safety reasons, take advice from your doctor before using dietary supplements, such as vitamins, or any other complementary or alternative medicines or medical practices. Because some dietary supplements may contain copper.
Can I prevent Wilson’s disease?
You can’t prevent Wilson’s disease. If there is a presence of a first-degree relative—a parent, sibling, or a child—present with
the Wilson disease, talk with your doctor about testing you and other family members for the disease. A doctor may begin
treating Wilson’s disease before symptoms appear. Early diagnosis and treatment can decrease or prevent organ damage.
Physical Therapy :
Test:
- Timed Up and Go (TUG)-Fall Risk
- 10 Meter Walk Test (10MWT)-Gait Speed
- Clinical Test for Sensory Interaction on Balance
- Static Balance – Functional Gait Assessment (FGA)
- Dynamic Balance – Activities-specific Balance and Confidence Scale (ABC Scale)
- Medical Research Council (MRC)-Limb muscle strength testing
- Videofluoroscopic swallowing study(VFSS) – [Evaluation of dysphagia according to the functional dysphagia scale].
Treatment goals were to decrease the risk of falls and the difficulty to conquer architectural barriers. The treatment was rest on static and dynamic balance exercises and functional capacity training.
Exercises aimed at:
- improving static balance
- improving dynamic balance
- functional capacity training
The exercise protocol is as follows:
Exercises aimed at improving static balance:
The training starts with standing position exercises, on a stable surface, with feet together,
- Standing position – half/semi tandem Tandem, One foot
- Somatosensory – open eyes and close eyes
In these positions, the patient was instructed with keeping the eyes closed trying to amend sensory weighting in the benevolence of somatosensory information.
These exercises were performed in 4 series of 1-minute duration with a break of 3 minutes.
Exercises aimed at improving dynamic balance:
This training was done on a treadmill (Treadmill Walking) under the supervision of a kinesiologist. Walking on a Treadmill intensity focuses on gaining stability using upper body balance. Initially, the patient might not keep up the gait without the help of his upper limb, so your first goal was to get the stability to accomplish the release. A cognitive task was added to the exercises as a modification of difficulty. Once it is achieved, the gait was conducted with eyes open horizontally and vertical head turns eyes closed. The dosage was furnished according to the patient’s tolerance, allowing him to perform cycles of approximately 3 minutes with breaks of 5 minutes this type of training lasted approximately 1 hour per session.
Exercises aimed at functional capacity training:
The initial training stage was aimed at the patient’s daily activities in which he found some difficulties, for occurrence, walking up and down stairs or ramps, picking up an object from the floor, and unstable surface gait. The patient’s dosage is given according to his tolerance, with rest periods between 3 and 5 minutes, with a total time of 30 minutes. The session ended with stretching the muscles of the lower limbs for 15 minutes.. On the other hand, the patient reported being satisfied with it.
Prognosis:
Assorted scoring systems have been put ahead for prognostication. Some of these assimilate levels of AST, bilirubin, prothrombin time, etc. on presentation.
Patients who have a prognostic score of 7 or more should be referred for a liver transplant. Patients with this score are basically dead within 8 weeks without treatment. After a liver transplant, the prognosis is better. A survival ratio of 87% at 15 years has been reported.
FAQs:
Where is Wilson’s disease most commonly seen?
This condition is most common in eastern Europeans, Sicilians, and southern Italians, but it can be seen in any group.
What deficiency causes Wilson’s disease?
It is caused by an overindulgence of copper that leads to accumulation of copper mainly in the liver, and brain and needs
lifelong de-coppering therapy. The overutilization of anti-copper agents may lead to a copper deficiency.
What is the first line for Wilson’s disease?
Chelating agents are recommended first-line for treating Wilson’s disease. Zinc may also be used which inhibits the absorption
of copper.
What foods contain copper?
The abundant dietary copper sources from food are shellfish, seeds and nuts, organ meats, wheat-bran cereals, whole-grain
products, and chocolate.
What is the gold standard test for Wilson’s disease?
The initial evaluation usually involves checking an individual’s eyes for signs of Wilson’s disease and a blood test for
caeruloplasmin, as this is the most widely accessible biochemical test for Wilson’s disease.
What foods to avoid copper?
The exhortation is to avoid the foods that contain the highest in copper: organ meats, shellfish, chocolate, nuts, and
mushrooms.
Are almonds high in copper?
Nuts and seeds, particularly almonds, cashews, and sesame seeds contain a good source of copper.
What is a normal copper level?
(in the blood) is 62 to 140 micrograms per deciliter (mcg/dL) is the normal level of copper.
What is Wilson’s disease’s common name?
Wilson’s disease is also known as hepatolenticular degeneration.


One Comment