Anterior Ankle Impingement and Physiotherapy Management
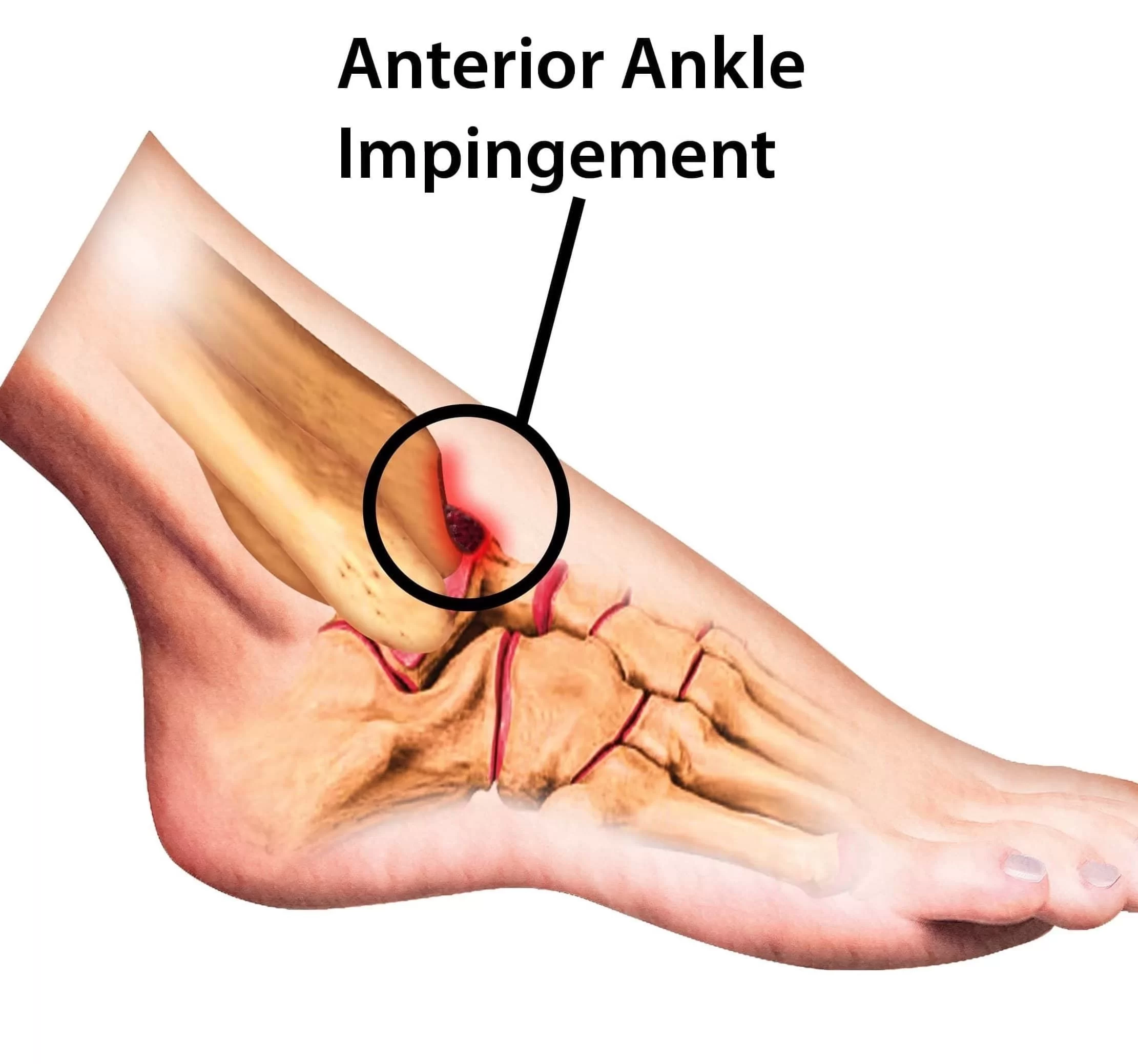
- Anterior ankle impingement syndrome is the result of chronic repetitive trauma with impingement of the anterior tibia against the talus.
- The anterior impingement syndrome of the ankle is strangulation that can be caused by soft tissue, like the joint capsule or scar tissue, and hard tissue which refers to bone tissue.
- Its location is the anterior side of the ankle in the talocrural joint. Due to repeated micro trauma’s little the ankle, the body will respond to this by building extra bone tissue called “osteophytes”. There are 3 types of osteophytes:
- Traction spur.
- Inflammatory spur.
- Osteophyte or chondro-osteophyte.
- The one occurring here is a chondro-osteophyte. It is a defense mechanism of the body that prevents further injury, but reduces mobility and can lead to pain due to impingement.
- There may potentially be swelling of the capsule and connective tissue. The relative contributions of the osseous and soft-tissue abnormalities are variable, but whatever component is dominant there is physical impingement and painful limitation of ankle movement.
Anatomy Related to Anterior Ankle Impingement
The joint capsule is ventral and dorsal minimally present, it is reinforced with ligaments on the lateral side. At the tendons of the lower leg muscles, at the back is the tendon of the medial flexor.
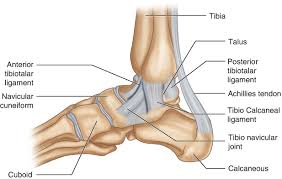
- These muscles prevent the parts of the joint capsule from getting trapped between bones.
- Foot free: In dorsiflexion the distal end of the talus moves lateral and the plantar side of the talus rotates to lateral.
- In plantar flexion the distal end of the talus moves medial, and the plantar side of the talus rotates to the medial.
- Foot stabilized on the floor: dorsal flexion provokes the tibia with the distal end of the tibia moves to medial.
- Plantar flexion provokes an exorotation of the tibia with the distal end of the tibia moves to lateral Stabilityin the talocrural joint is the weakest in neutral position, this is because in this position the ligaments that surround the ankle are less tensed than in dorsal flexion or plantar flexion and there is less contact between joint facets.
- Plantar flexion has more stability, there is more contact between the joint facets and the tibionavicular part as well as the tibiotalar anterior part of the ligament deltoideum.
- The greatest stability occurs in dorsiflexion, the large front part of the trochlea tali now comes in touch with the small, narrow back part of the joint socket, when this happens, the tibia and the fibula widen a bit and keep the talus closely bound helps with the strong tibiofibular ligaments.
Etiology of Anterior Ankle Impingement
- This syndrome is called footballer’s ankle or athlete’s ankle because these sports are responsible for creating pressure on the cartilage in the ankle.
- This is especially common in football where the kicking motion is responsible for reoccurring micro trauma’s, leading to an increased chance of anterior impingement syndrome (AIS).
- These 2 sports together with dance are the majority of AIS patients. Epidemiological figures were not found but because anterior impingement is frequently preceded by an ankle sprain, AIS of the ankle is a chronic disorder.
- Pain occurs in full dorsal flexion or full plantar flexion. AIS does not occur as a result of insidious onset.
- AIS will usually occur when there is pre-existing damage to the ankle. The cause of this damage can be inflammation. Due to inflammation the soft tissue will swell and have reduced elasticity, leading to impingement.
- The second cause can be arthritis, the body responds to arthritis by building extra bone tissue, these are called osteophytes, the body acts this way because it prevents reoccurring micro-trauma due to decreased range of movement.
Symptoms of Anterior Ankle Impingement
- Clinical features of anterior ankle impingement syndrome include painful and limited dorsiflexion and anterior joint line swelling.
- Anterior impingement can occur after a severe previous ankle sprain or repeated weight-bearing activities with ensuing thickening of the injured ligaments, resulting in their impingement between the anterior inferior tibia and the talus. Individuals that suffer from anterior ankle impingement may present with:
- Dull ache at the front of the ankle with rest, which then becomes sharp pain at the front of the ankle with excessive dorsiflexion or weight-bearing
- Increased symptoms following specific activities, including:
- Walking or running excessively (especially up hills or on uneven surfaces)
- Deep squatting or lunging (especially with the knee moving forwards over the toes)
- Landing from a jump (particularly on an incline or a rough surface)
- Performing a calf stretch (particularly with the knee bent)
- Heavy lifting or twisting activities
- Tenderness on palpation of the front of the ankle joint.
- In some cases, a clicking sensation during specific ankle movements.
- Puffiness or swelling of the ankle joint.
Diagnosis of Anterior Ankle Impingement
Diagnosis can be made based on 3 sources of information:
Clinical Investigation:
- X-rays can bring clarity if osteophytes are present. The x-ray should be taken from the lateral side, where the bone structures of the ankle are clearly visible.
- It is also to bear in mind that some osteophytes still may not be visible on the x-ray.
- To solve this problem research has shown that an anteromedial impingement recording, this is an x-ray where the angle is changed for optimal osteophyte recognition, is a useful adjunct to the standard x-ray.
Patient Subjective History
- Taking a thorough and complete subjective history from the patient can be vitally important in diagnosing a case of AIS. In the subjective assessment, the physiotherapist will gain information on any previous injuries at the ankle and will gain insight into the patient’s hobbies and occupation, both influencing factors in the development of AIS.
Patient Objective Assessment
- During the physiotherapist’s objective assessment, they will look for the following: Pain while palpating the anterior side of the joint.
- Pain with forced dorsiflexion. Whether it is possible to reproduce anterior impingement pain by palpating the anterolateral ankle in plantar flexion, then dorsiflexing the ankle while maintaining pressure with the examiner’s digit over the anterolateral ankle. An increase in pain is 95% sensitive and 88% specific for AIS.
- AIS test should be positive: standing on both feet and leaning forwards, positive is defined as pain and possibly a difference of approximately 5 degrees between the two ankles.
- The ankle may be swollen and can be read.
Medical Management of Anterior Ankle Impingement
Limitation:
- The first advice that has to be given to the patient is that he or she should stop any activity that increases pain, this allows the body to start the healing process without further tissue damage while at the same time preventing a worsening of the situation and the problem becoming chronic.
- Later on, the activity can gradually start building up before returning to the original levels. Alternative exercises can be used with which generates less force on the ankle, this includes; swimming, cycling, water sport, etc.
- Another option is to use a slightly raised heel, this means that the foot does not need to go as far up as normal. The use of crutches is another method to prevent further damage to the ankle.
Reducing Pain:
- Cryotherapy is an effective way of managing the pain created by AIS. Based on the available evidence, cryotherapy seems to be effective in decreasing pain. In comparison with other rehabilitation techniques, the efficacy of cryotherapy has been questioned.
- Additionally, the low methodological quality of the available evidence is of concern. Many more high-quality studies are required to create evidence-based guidelines on the use of cryotherapy.
- These must focus on developing modes, durations, and frequencies of ice application that will optimize outcomes after injury. (Does Cryotherapy Improve Outcomes With Soft Tissue Injury?
- Corticoid injection: An occasional injection of corticosteroids into the ankle joint may be helpful particularly
if there is some underlying ankle arthritis present.
Surgery:
- In some instances of AIS, operative treatment may be helpful. If the main cause of a patient’s symptoms is from impingement (rather than ankle arthritis) removing the prominent impinging bony spurs can relieve symptoms.
- Surgical treatment of ankle impingement involves removing the prominent bone spurs either by arthroscopic surgery or by opening up the ankle joint with an incision.
- If the bone spurs are large it is often easier and faster to simply open up the ankle joint and remove the bone spurs rather than attempt to do this arthroscopic.
- Surgery to remove impinging bone spurs from the front of the ankle will not typically help symptoms if the pain is generalized around the ankle due to significant ankle arthritis rather than specifically located in the front of the ankle.
- In some instances, surgery to remove the bony spurs can make a patient’s symptoms worse if it allows the ankle joint to move more and the ankle joint itself has significant arthritis. The bony spurs themselves will tend to grow back over time.
- Recurrence of symptoms is not uncommon. At long-term follow-up, arthroscopic excision of both soft-tissue overgrowths and osteophytes was shown to be an effective way of treating anterior impingement, provided that there was no preoperative narrowing of the joint space.
- Other Management Options:
- Soft tissue massage can help reduce pain. Use of heat improves blood circulation and stimulates the healing process
- Taping/Bracing of the ankle helps to control movement and support the natural structure of the ankle.
- These methods are questionable as there is a lack of detailed research supporting their use meaning it is not supported by evidence-based practice, one of the core principles of physiotherapy.
Physiotherapy Management:
Physiotherapy can be given following the KNGF guidelines, which are complementary to the different
Phases of inflammation:
- Phase 1 of recovery: inflammation 0-3 days

- Rest and immobilization, but a frequent movement within pain limits.
- Use pain as a guideline to base your exercises on.
- Eating behaviors (vitamin C, proteins, anti-oxidants,…).
- Exercise basic functions, move feet, and toes to improve blood circulation.
- Limit painkillers to the bare minimum.
- Phase 2 of recovery: limited functionality 4-10 days
- Mobilization to improve scar tissue quality.
- Muscle endurance training within free ROM.
- Proprioceptive training.
- Train muscle strength of “foot raiser muscles” (tricep surae muscles or the plantar flexor muscles. The
- Gastrocnemius and soleus muscles) using more weight and fewer repetitions.
- Normal ROM should be reached.
- Phase 3 of recovery: early revalidation 11-21 days

- Mobilizations with a progressively enhancing ROM
- Proprioceptive training
- Muscle strength training
- Research and estimate the level of daily activity, modify therapy with this info
- Phase 4 of recovery: late revalidation 3-6 weeks
- Improve load capacity, running, and climbing stairs.
- Coordination training with ADL.
- The goal is to end exercises with a load like before the incident.
- Progressive build-up of schedule: static dynamic/selective functional.
- Phase 5 of recovery: early sporting: 6-8 weeks
- Phase 6 of recovery: late sporting starting week 8
- Improve sporting: practice and improve functions and activities based on sports. Sufficient rest and repair moments.
- Prevention: It is recommended to improve the awareness of injury prevention strategies for players and athletes.
- These strategies were identified as: use of shin pads during training, carbohydrate intake before and after training and after matches, cool downs after training and matches, and flexibility work



One Comment